Key Points
-
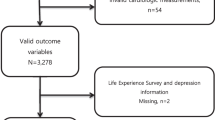
Pooling of individual-level data and published data from multiple cohorts into mega-studies has allowed for a more precise assessment of the association between stress and cardiovascular disease
-
In the general population, adults with work stress or private-life stress have a 1.1-fold to 1.6-fold increased risk of incident coronary heart disease and stroke
-
The excess risk of cardiovascular disease associated with adulthood stress is less marked than the risks associated with smoking, high blood pressure, high serum cholesterol levels, obesity, or multiple severe stressful experiences in childhood
-
Stress in adulthood has an important role as a disease trigger in individuals with high atherosclerotic plaque burden and as a determinant of prognosis and outcomes in those with pre-existing cardiovascular or cerebrovascular disease
-
Potential pathophysiological effects of stress involve increased cardiac electrical instability, myocardial ischaemia, plaque disruption, and thrombus formation, contributing to clinical events such as arrhythmia, myocardial infarction, cardiomyopathy, and stroke
-
Only European guidelines for cardiovascular disease prevention acknowledge stress as a clinically meaningful risk factor in individuals with a high overall risk of cardiovascular disease or with established cardiovascular disease
Abstract
Cardiovascular disease remains the leading cause of disease burden globally, which underlies the continuing need to identify new complementary targets for prevention. Over the past 5–10 years, the pooling of multiple data sets into 'mega-studies' has accelerated progress in research on stress as a risk and prognostic factor for cardiovascular disease. Severe stressful experiences in childhood, such as physical abuse and household substance abuse, can damage health and increase the risk of multiple chronic conditions in adulthood. Compared with childhood stress and adulthood classic risk factors, such as smoking, high blood pressure, and high serum cholesterol levels, the harmful effects of stress in adulthood are generally less marked. However, adulthood stress has an important role as a disease trigger in individuals who already have a high atherosclerotic plaque burden, and as a determinant of prognosis and outcome in those with pre-existing cardiovascular or cerebrovascular disease. In real-life settings, mechanistic studies have corroborated earlier laboratory-based observations on stress-related pathophysiological changes that underlie triggering, such as lowered arrhythmic threshold and increased sympathetic activation with related increases in blood pressure, as well as pro-inflammatory and procoagulant responses. In some clinical guidelines, stress is already acknowledged as a target for prevention for people at high overall risk of cardiovascular disease or with established cardiovascular disease. However, few scalable, evidence-based interventions are currently available.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Keys, A. et al. Coronary heart disease among Minnesota business and professional men followed fifteen years. Circulation 28, 381–395 (1963).
Mahmood, S. S., Levy, D., Vasan, R. S. & Wang, T. J. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet 383, 999–1008 (2014).
Doll, R. & Hill, A. B. The mortality of doctors in relation to their smoking habits; a preliminary report. BMJ 1, 1451–1455 (1954).
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1151–1210 (2017).
Tzoulaki, I., Elliott, P., Kontis, V. & Ezzati, M. Worldwide exposures to cardiovascular risk factors and associated health effects: current knowledge and data gaps. Circulation 133, 2314–2333 (2016).
Ezzati, M. et al. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat. Rev. Cardiol. 12, 508–530 (2015).
GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1260–1344 (2017).
Kivimäki, M. & Kawachi, I. Work stress as a risk factor for cardiovascular disease. Curr. Cardiol. Rep. 17, 630–639 (2015).
Dragano, N. et al. Effort-reward imbalance at work and incident coronary heart disease: a multi-cohort study of 90,164 individuals. Epidemiology 28, 619–626 (2017).
Kivimäki, M. et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet 386, 1739–1746 (2015).
Huang, Y. et al. Association between job strain and risk of incident stroke: a meta-analysis. Neurology 85, 1648–1654 (2015).
Nyberg, S. T. et al. Job strain as a risk factor for type 2 diabetes: a pooled analysis of 124 808 men and women. Diabetes Care 37, 2268–2275 (2014).
Ferrie, J. E. et al. Job insecurity and risk of diabetes: a meta-analysis of individual participant data. CMAJ 188, E447–E455 (2016).
Hackett, R. A. & Steptoe, A. Type 2 diabetes mellitus and psychological stress — a modifiable risk factor. Nat. Rev. Endocrinol. 13, 547–560 (2017).
Madsen, I. E. H. et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol. Med. 47, 1342–1356 (2017).
Heikkilä, K. et al. Work stress and risk of cancer: meta-analysis of 5700 incident cancer events in 116,000 European men and women. BMJ 346, f165 (2013).
Heikkilä, K. et al. Long working hours and cancer risk: a multi-cohort study. Br. J. Cancer 114, 813–818 (2016).
Heikkilä, K. et al. Job strain and the risk of inflammatory bowel diseases: individual-participant meta-analysis of 95,000 men and women. PLoS ONE 9, e88711 (2014).
Heikkilä, K. et al. Job strain and COPD exacerbations: an individual-participant meta-analysis. Eur. Resp. J. 44, 247–251 (2014).
Heikkilä, K. et al. Job strain and the risk of severe asthma exacerbations: a meta-analysis of individual-participant data from 100 000 European men and women. Allergy 69, 775–783 (2014).
Brotman, D. J., Golden, S. H. & Wittstein, I. S. The cardiovascular toll of stress. Lancet 370, 1089–1100 (2007).
Steptoe, A. & Kivimäki, M. Stress and cardiovascular disease. Nat. Rev. Cardiol. 9, 360–370 (2012).
Steptoe, A. & Kivimäki, M. Stress and cardiovascular disease: an update on current knowledge. Annu. Rev. Public Health 34, 337–354 (2013).
Rozanski, A., Blumenthal, J. A., Davidson, K. W., Saab, P. G. & Kubzansky, L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J. Am. Coll. Cardiol. 45, 637–651 (2005).
Rozanski, A., Blumenthal, J. A. & Kaplan, J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 99, 2192–2217 (1999).
McEwen, B. S. Protective and damaging effects of stress mediators. N. Engl. J. Med. 338, 171–179 (1998).
Orth-Gomer, K. et al. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA 284, 3008–3014 (2000).
Lee, S., Colditz, G. A., Berkman, L. F. & Kawachi, I. Caregiving and risk of coronary heart disease in U. S. women: a prospective study. Am. J. Prev. Med. 24, 113–119 (2003).
Carey, I. M. et al. Increased risk of acute cardiovascular events after partner bereavement: a matched cohort study. JAMA Intern. Med. 174, 598–605 (2014).
Kario, K., McEwen, B. S. & Pickering, T. G. Disasters and the heart: a review of the effects of earthquake-induced stress on cardiovascular disease. Hypertens. Res. 26, 355–367 (2003).
Qureshi, E. A., Merla, V., Steinberg, J. & Rozanski, A. Terrorism and the heart: implications for arrhythmogenesis and coronary artery disease. Card. Electrophysiol. Rev. 7, 80–84 (2003).
Smyth, A. et al. Physical activity and anger or emotional upset as triggers of acute myocardial infarction: the INTERHEART study. Circulation 134, 1059–1067 (2016).
Vahtera, J. et al. Organisational downsizing, sickness absence, and mortality: 10-town prospective cohort study. BMJ 328, 555–560 (2004).
Correll, C. U. et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 16, 163–180 (2017).
Gan, Y. et al. Depression and the risk of coronary heart disease: a meta-analysis of prospective cohort studies. BMC Psychiatry 14, 371 (2014).
Gathright, E. C., Goldstein, C. M., Josephson, R. A. & Hughes, J. W. Depression increases the risk of mortality in patients with heart failure: a meta-analysis. J. Psychosom. Res. 94, 82–89 (2017).
Celano, C. M. et al. Association between anxiety and mortality in patients with coronary artery disease: a meta-analysis. Am. Heart. J. 170, 1105–1115 (2015).
Russ, T. C. et al. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ 345, e4933 (2012).
Cohen, R., Bavishi, C., Haider, S., Thankachen, J. & Rozanski, A. Meta-analysis of relation of vital exhaustion to cardiovascular disease events. Am. J. Cardiol. 119, 1211–1216 (2017).
Edmondson, D., Kronish, I. M., Shaffer, J. A., Falzon, L. & Burg, M. M. Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review. Am. Heart J. 166, 806–814 (2013).
Hemingway, H. & Marmot, M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ 318, 1460–1467 (1999).
Grande, G., Romppel, M. & Barth, J. Association between type D personality and prognosis in patients with cardiovascular diseases: a systematic review and meta-analysis. Ann. Behav. Med. 43, 299–310 (2012).
Chida, Y. & Steptoe, A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J. Am. Coll. Cardiol. 53, 936–946 (2009).
Bandodkar, A. J. & Wang, J. Non-invasive wearable electrochemical sensors: a review. Trends Biotechnol. 32, 363–371 (2014).
Kuhn, E. et al. Preliminary evaluation of PTSD Coach, a smartphone app for post-traumatic stress symptoms. Mil. Med. 179, 12–18 (2014).
Mitchell, J. S., Lowe, T. E. & Ingram, J. R. Rapid ultrasensitive measurement of salivary cortisol using nano-linker chemistry coupled with surface plasmon resonance detection. Analyst 134, 380–386 (2009).
Lampert, R. et al. Triggering of symptomatic atrial fibrillation by negative emotion. J. Am. Coll. Cardiol. 64, 1533–1534 (2014).
Kivimäki, M. et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet 380, 1491–1497 (2012).
Kivimäki, M., Singh-Manoux, A., Ferrie, J. E. & Batty, G. D. Post hoc decision-making in observational epidemiology — is there need for better research standards? Int. J. Epidemiol. 42, 367–370 (2013).
Balshem, H. et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 64, 401–406 (2011).
Sarwar, N. et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375, 2215–2222 (2010).
Lewington, S. et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360, 1903–1913 (2002).
Lewington, S. et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet 370, 1829–1839 (2007).
Kivimäki, M. et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2, e277–e285 (2017).
Parish, S. et al. Cigarette smoking, tar yields, and non-fatal myocardial infarction: 14,000 cases and 32,000 controls in the United Kingdom. BMJ 311, 471 (1995).
Valtorta, N. K., Kanaan, M., Gilbody, S., Ronzi, S. & Hanratty, B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 102, 1009–1016 (2016).
Fransson, E. I. et al. Job strain and the risk of stroke: an individual-participant data meta-analysis. Stroke 46, 557–559 (2015).
Hughes, K. et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2, e356–366 (2017).
O'Donnell, M. J. et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 388, 761–775 (2016).
Mostofsky, E., Penner, E. A. & Mittleman, M. A. Outbursts of anger as a trigger of acute cardiovascular events: a systematic review and meta-analysis. Eur. Heart J. 35, 1404–1410 (2014).
Li, J., Zhang, M., Loerbroks, A., Angerer, P. & Siegrist, J. Work stress and the risk of recurrent coronary heart disease events: a systematic review and meta-analysis. Int. J. Occup. Med. Environ. Health 28, 8–19 (2015).
Arnold, S. V., Smolderen, K. G., Buchanan, D. M., Li, Y. & Spertus, J. A. Perceived stress in myocardial infarction: long-term mortality and health status outcomes. J. Am. Coll. Cardiol. 60, 1756–1763 (2012).
Wilbert-Lampen, U. et al. Cardiovascular events during World Cup soccer. N. Engl. J. Med. 358, 475–483 (2008).
Stewart, R. A. H. et al. Persistent psychological distress and mortality in patients with stable coronary artery disease. Heart http://dx.doi.org/10.1136/heartjnl-2016-311097 (2017).
Wei, J. et al. Meta-analysis of mental stress-induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease. Am. J. Cardiol. 114, 187–192 (2014).
Fleshner, M. & Crane, C. R. Exosomes, DAMPs and miRNA: features of stress physiology and immune homeostasis. Trends Immunol. 38, 768–776 (2017).
Chrousos, G. P. & Gold, P. W. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA 267, 1244–1252 (1992).
Huang, Q. H., Takaki, A. & Arimura, A. Central noradrenergic system modulates plasma interleukin-6 production by peripheral interleukin-1. Am. J. Physiol. 273, R731–738 (1997).
Goebel, M. U., Mills, P. J., Irwin, M. R. & Ziegler, M. G. Interleukin-6 and tumor necrosis factor-alpha production after acute psychological stress, exercise, and infused isoproterenol: differential effects and pathways. Psychosom. Med. 62, 591–598 (2000).
Carrive, P. Dual activation of cardiac sympathetic and parasympathetic components during conditioned fear to context in the rat. Clin. Exp. Pharmacol. Physiol. 33, 1251–1254 (2006).
Tsigos, C. & Chrousos, G. P. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. J. Psychosomat. Res. 53, 865–871 (2002).
Munck, A., Guyre, P. M. & Holbrook, N. J. Physiological functions of glucocorticoids in stress and their relation to pharmacological actions. Endocrin. Rev. 5, 25–44 (1984).
Smyth, G. P. et al. Glucocorticoid pretreatment induces cytokine overexpression and nuclear factor-κB activation in macrophages. J. Surg. Res. 116, 253–261 (2004).
Yeager, M. P., Pioli, P. A. & Guyre, P. M. Cortisol exerts bi-phasic regulation of inflammation in humans. Dose Response 9, 332–347 (2011).
Frank, M. G., Watkins, L. R. & Maier, S. F. Stress-induced glucocorticoids as a neuroendocrine alarm signal of danger. Brain Behav. Immun. 33, 1–6 (2013).
Babu, G. R. et al. Is hypertension associated with job strain? A meta-analysis of observational studies. Occup. Environ. Med. 71, 220–227 (2014).
Nyberg, S. et al. Job strain and cardiovascular disease risk factors: an individual-participant data meta-analysis of 47,000 men and women. PLoS ONE 8, e67323 (2013).
Magnusson-Hanson, L. et al. Work stress, anthropometry, lung function, blood pressure, and blood-based biomarkers: a cross-sectional study of 43,593 French men and women. Sci. Rep. 7, 9282 (2017).
Kivimäki, M. et al. Long working hours as a risk factor for atrial fibrillation: a multi-cohort study. Eur. Heart J. 8, 2621–2628 (2017).
Sparrenberger, F. et al. Does psychosocial stress cause hypertension? A systematic review of observational studies. J. Hum. Hypertens. 23, 12–19 (2009).
Heikkilä, K. et al. Job strain and tobacco smoking: an individual-participant data meta-analysis of 166,130 adults in 15 European studies. PLoS ONE 7, e35463 (2012).
Virtanen, M. et al. Long working hours and alcohol use: systematic review and meta-analysis of published studies and unpublished individual participant data. BMJ 350, g7772 (2015).
Fransson, E. I. et al. Job strain as a risk factor for leisure-time physical inactivity: An individual-participant meta-analysis of up to 170 000 men and women: the IPD-Work Consortium. Am. J. Epidemiol. 176, 1078–1089 (2012).
Chandola, T. et al. Work stress and coronary heart disease: what are the mechanisms? Eur. Heart J. 29, 640–648 (2008).
Wardle, J., Chida, Y., Gibson, E. L., Whitaker, K. L. & Steptoe, A. Stress and adiposity: a meta-analysis of longitudinal studies. Obesity 19, 771–778 (2011).
Nyberg, S. T. et al. Job strain in relation to body mass index: pooled analysis of 160 000 adults from 13 cohort studies. J. Intern. Med. 272, 65–73 (2012).
Kivimäki, M., Singh-Manoux, A., Nyberg, S. N., Jokela, M. & Virtanen, M. Job strain and risk of obesity: systematic review and meta-analysis of cohort studies. Int. J. Obes. 39, 597–600 (2015).
Arri, S. S., Ryan, M., Redwood, S. R. & Marber, M. S. Mental stress-induced myocardial ischaemia. Heart 102, 472–480 (2016).
Heberden, W. Commentaries on the History and Cure of Diseases (Wells and Lilly, 1818).
Rozanski, A. et al. Mental stress and the induction of silent myocardial ischemia in patients with coronary artery disease. N. Engl. J. Med. 318, 1005–1012 (1988).
Blumenthal, J. A. et al. Mental stress-induced ischemia in the laboratory and ambulatory ischemia during daily life. Association and hemodynamic features. Circulation 92, 2102–2108 (1995).
Deanfield, J. E. et al. Silent myocardial ischaemia due to mental stress. Lancet 2, 1001–1005 (1984).
Krantz, D. S., Sheps, D. S., Carney, R. M. & Natelson, B. H. Effects of mental stress in patients with coronary artery disease: evidence and clinical implications. JAMA 283, 1800–1802 (2000).
Gottdiener, J. S. et al. Induction of silent myocardial ischemia with mental stress testing: relation to the triggers of ischemia during daily life activities and to ischemic functional severity. J. Am. Coll. Cardiol. 24, 1645–1651 (1994).
Gullette, E. C. et al. Effects of mental stress on myocardial ischemia during daily life. JAMA 277, 1521–1526 (1997).
Strike, P. C. & Steptoe, A. Systematic review of mental stress-induced myocardial ischaemia. Eur. Heart J. 24, 690–703 (2003).
Strike, P. C. et al. Pathophysiological processes underlying emotional triggering of acute cardiac events. Proc. Natl Acad. Sci. USA 103, 4322–4327 (2006).
Arbab-Zadeh, A., Nakano, M., Virmani, R. & Fuster, V. Acute coronary events. Circulation 125, 1147–1156 (2012).
Anderson, J. L. & Morrow, D. A. Acute myocardial infarction. N. Engl. J. Med. 376, 2053–2064 (2017).
Naghavi, M. et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part II. Circulation 108, 1772–1778 (2003).
Edmondson, D., Newman, J. D., Whang, W. & Davidson, K. W. Emotional triggers in myocardial infarction: do they matter? Eur. Heart J. 34, 300–306 (2013).
Ackland, G. L. et al. Autonomic regulation of systemic inflammation in humans: a multi-center, blinded observational cohort study. Brain Behav. Immun. http://dx.doi.org/10.1016/j.bbi.2017.08.010 (2017).
Lampert, R. Mental stress and ventricular arrhythmias. Curr. Cardiol. Rep. 18, 118 (2016).
Steptoe, A. & Marmot, M. Psychosocial, hemostatic, and inflammatory correlates of delayed poststress blood pressure recovery. Psychosom. Med. 68, 531–537 (2006).
Landsbergis, P. A., Dobson, M., Koutsouras, G. & Schnall, P. Job strain and ambulatory blood pressure: a meta-analysis and systematic review. Am. J. Public Health 103, e61–e71 (2013).
Heikkilä, K. et al. Job strain and alcohol intake: a collaborative meta-analysis of individual-participant data from 140,000 men and women. PLoS ONE 7, e40101 (2012).
Park, H. W. et al. Neural mechanisms of atrial fibrillation. Curr. Opin. Cardiol. 27, 24–28 (2012).
Tawakol, A. et al. Relation between resting amygdalar activity and cardiovascular events: a longitudinal and cohort study. Lancet 389, 834–845 (2017).
Muscatell, K. A. et al. Greater amygdala activity and dorsomedial prefrontal-amygdala coupling are associated with enhanced inflammatory responses to stress. Brain Behav. Immun. 43, 46–53 (2015).
Silvestrini, N. Psychological and neural mechanisms associated with effort-related cardiovascular reactivity and cognitive control: an integrative approach. Int. J. Psychophysiol. 119, 11–18 (2017).
Gianaros, P. J. et al. An inflammatory pathway links atherosclerotic cardiovascular disease risk to neural activity evoked by the cognitive regulation of emotion. Biol. Psychiatry 75, 738–745 (2014).
Eisenberger, N. I., Taylor, S. E., Gable, S. L., Hilmert, C. J. & Lieberman, M. D. Neural pathways link social support to attenuated neuroendocrine stress responses. NeuroImage 35, 1601–1612 (2007).
Meschia, J. F. et al. Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45, 3754–3832 (2014).
Kessing, D., Denollet, J., Widdershoven, J. & Kupper, N. Psychological determinants of heart failure self-care: systematic review and meta-analysis. Psychosom. Med. 78, 412–431 (2016).
Rieckmann, N. et al. Course of depressive symptoms and medication adherence after acute coronary syndromes: an electronic medication monitoring study. J. Am. Coll. Cardiol. 48, 2218–2222 (2006).
Doyle, F. et al. Systematic review and meta-analysis of the impact of depression on subsequent smoking cessation in patients with coronary heart disease: 1990 to 2013. Psychosom. Med. 76, 44–57 (2014).
Richardson, S. et al. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am. J. Cardiol. 110, 1711–1716 (2012).
Toren, K., Schioler, L., Soderberg, M., Giang, K. W. & Rosengren, A. The association between job strain and atrial fibrillation in Swedish men. Occup. Environ. Med. 72, 177–180 (2015).
Fransson, E. I. et al. The association between job strain and atrial fibrillation: results from the Swedish WOLF study. BioMed Res. Int. 2015, 371905 (2015).
Leor, J., Poole, W. K. & Kloner, R. A. Sudden cardiac death triggered by an earthquake. N. Engl. J. Med. 334, 413–419 (1996).
Trichopoulos, D., Katsouyanni, K., Zavitsanos, X., Tzonou, A. & Dalla-Vorgia, P. Psychological stress and fatal heart attack: the Athens (1981) earthquake natural experiment. Lancet 321, 441–444 (1983).
Jiao, Z. et al. Effect of Hurricane Katrina on incidence of acute myocardial infarction in New Orleans three years after the storm. Am. J. Cardiol. 109, 502–505 (2012).
Meisel, S. R. et al. Effect of Iraqi missile war on incidence of acute myocardial infarction and sudden death in Israeli civilians. Lancet 338, 660–661 (1991).
Witte, D. R., Bots, M. L., Hoes, A. W. & Grobbee, D. E. Cardiovascular mortality in Dutch men during 1996 European football championship: longitudinal population study. BMJ 321, 1552 (2000).
Carroll, D. et al. Blood pressure reactions to acute psychological stress and future blood pressure status: a 10-year follow-up of men in the Whitehall II study. Psychosom. Med. 63, 737–743 (2001).
Nawrot, T. S., Perez, L., Kunzli, N., Munters, E. & Nemery, B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet 377, 732–740 (2011).
Tofler, G. H. et al. Triggers and timing of acute coronary syndromes. Am. J. Cardiol. 119, 1560–1565 (2017).
Mittleman, M. A. & Mostofsky, E. Physical, psychological and chemical triggers of acute cardiovascular events: preventive strategies. Circulation 124, 346–354 (2011).
Fang, F. et al. Suicide and cardiovascular death after a cancer diagnosis. N. Engl. J. Med. 366, 1310–1318 (2012).
Maclure, M. & Mittleman, M. A. Should we use a case-crossover design? Annu. Rev. Public Health 21, 193–221 (2000).
Koton, S., Tanne, D., Bornstein, N. M. & Green, M. S. Triggering risk factors for ischemic stroke: a case-crossover study. Neurology 63, 2006–2010 (2004).
Guiraud, V., Touze, E., Rouillon, F., Godefroy, O. & Mas, J. L. Stressful life events as triggers of ischemic stroke: a case-crossover study. Int. J. Stroke 8, 300–307 (2013).
Kivimäki, M., Vahtera, J., Pentti, J. & Ferrie, J. E. Factors underlying the effect of organisational downsizing on health of employees: longitudinal cohort study. BMJ 320, 971 (2000).
Ghadri, J. R. et al. Happy heart syndrome: role of positive emotional stress in takotsubo syndrome. Eur. Heart J. 37, 2823–2829 (2016).
Dawson, D. K. Acute stress-induced (takotsubo) cardiomyopathy. Heart http://dx.doi.org/10.1136/heartjnl-2017-311579 (2017).
Templin, C. et al. Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. N. Engl. J. Med. 373, 929–938 (2015).
Wittstein, I. S. et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N. Engl. J. Med. 352, 539–548 (2005).
Steinberg, J. S. et al. Increased incidence of life-threatening ventricular arrhythmias in implantable defibrillator patients after the World Trade Center attack. J. Am. Coll. Cardiol. 44, 1261–1264 (2004).
Aboa-Eboule, C. et al. Job strain and risk of acute recurrent coronary heart disease events. JAMA 298, 1652–1660 (2007).
Laszlo, K. D., Ahnve, S., Hallqvist, J., Ahlbom, A. & Janszky, I. Job strain predicts recurrent events after a first acute myocardial infarction: the Stockholm Heart Epidemiology Program. J. Intern. Med. 267, 599–611 (2010).
Biering, K., Andersen, J. H., Lund, T. & Hjollund, N. H. Psychosocial working environment and risk of adverse cardiac events in patients treated for coronary heart disease. J. Occup. Rehabil. 25, 770–775 (2015).
Aboa-Eboule, C. et al. Effort-reward imbalance at work and recurrent coronary heart disease events: a 4-year prospective study of post-myocardial infarction patients. Psychosom. Med. 73, 436–447 (2011).
Georgiades, A., Janszky, I., Blom, M., Laszlo, K. D. & Ahnve, S. Financial strain predicts recurrent events among women with coronary artery disease. Int. J. Cardiol. 135, 175–183 (2009).
Ruberman, W., Weinblatt, E., Goldberg, J. D. & Chaudhary, B. S. Psychosocial influences on mortality after myocardial infarction. N. Engl. J. Med. 311, 552–559 (1984).
Nieuwlaat, R., Schwalm, J. D., Khatib, R. & Yusuf, S. Why are we failing to implement effective therapies in cardiovascular disease? Eur. Heart J. 34, 1262–1269 (2013).
Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 14, 32–38 (1985).
Brugts, J. J. et al. Impact of renin-angiotensin system inhibitors on mortality and major cardiovascular endpoints in hypertension: a number-needed-to-treat analysis. Int. J. Cardiol. 181, 425–429 (2015).
Lear, S. A. et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet http://dx.doi.org/10.1016/S0140-6736(17)31634-3 (2017).
Yusuf, S. et al. Blood-pressure and cholesterol lowering in persons without cardiovascular disease. N. Engl. J. Med. 374, 2032–2043 (2016).
Collins, R. et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 388, 2532–2561 (2016).
Cholesterol Treatment Trialists Collaboration et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380, 581–590 (2012).
Macleod, J. & Davey Smith, G. Psychosocial factors and public health: a suitable case for treatment? J. Epidemiol. Comm. Health 57, 565–570 (2003).
Masi, C. M., Chen, H. Y., Hawkley, L. C. & Cacioppo, J. T. A meta-analysis of interventions to reduce loneliness. Pers. Soc. Psychol. Rev. 15, 219–266 (2011).
Lucini, D. & Pagani, M. From stress to functional syndromes: an internist's point of view. Eur. J. Intern. Med. 23, 295–301 (2012).
Buchholz, L. Working late, courting stroke. JAMA 314, 1679–1680 (2015).
Ministère du Travail. Droit à la déconnexion [French]. Ministère du Travail http://travail-emploi.gouv.fr/archives/archives-courantes/loi-travail-2016/les-principales-mesures-de-la-loi-travail/article/droit-a-la-deconnexion (2017).
Tofler, G. H. & Muller, J. E. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation 114, 1863–1872 (2006).
Ruzek, J. I., Kuhn, E., Jaworski, B. K., Owen, J. E. & Ramsey, K. M. Mobile mental health interventions following war and disaster. mHealth 2, 37 (2016).
Rozanski, A. Exercise as medical treatment for depression. J. Am. Coll. Cardiol. 60, 1064–1066 (2012).
Rebar, A. L. et al. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 9, 366–378 (2015).
Fonarow, G. C. et al. Workplace wellness recognition for optimizing workplace health: a presidential advisory from the American Heart Association. Circulation 131, e480–497 (2015).
Kornitzer, M. et al. Belgian heart disease prevention project: incidence and mortality results. Lancet 321, 1066–1070 (1983).
Linden, W., Phillips, M. J. & Leclerc, J. Psychological treatment of cardiac patients: a meta-analysis. Eur. Heart J. 28, 2972–2984 (2007).
Gulliksson, M. et al. Randomized controlled trial of cognitive behavioral therapy versus standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary Prevention in Uppsala Primary Health Care project (SUPRIM). Arch. Intern. Med. 171, 134–140 (2011).
Blumenthal, J. A. et al. Enhancing cardiac rehabilitation with stress management training: A randomized, clinical efficacy trial. Circulation 133, 1341–1350 (2016).
Richards, S. H. et al. Psychological interventions for coronary heart disease. Cochrane Database Syst. Rev. 4, CD002902 (2017).
Anderson, L. et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J. Am. Coll. Cardiol. 67, 1–12 (2016).
Pogosova, N. et al. Psychosocial aspects in cardiac rehabilitation: from theory to practice. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation of the European Society of Cardiology. Eur. J. Prev. Cardiol. 22, 1290–1306 (2015).
van Halewijn, G. et al. Lessons from contemporary trials of cardiovascular prevention and rehabilitation: a systematic review and meta-analysis. Int. J. Cardiol. 232, 294–303 (2017).
West, R. R., Jones, D. A. & Henderson, A. H. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 98, 637–644 (2012).
Herring, M. P., Puetz, T. W., O'Connor, P. J. & Dishman, R. K. Effect of exercise training on depressive symptoms among patients with a chronic illness: a systematic review and meta-analysis of randomized controlled trials. Arch. Intern. Med. 172, 101–111 (2012).
Frieden, T. R. Evidence for health decision making - Beyond randomized, controlled trials. N. Engl. J. Med. 377, 465–475 (2017).
Piepoli, M. F. et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Eur. Heart J. 37, 2315–2381 (2016).
Anderson, T. J. et al. 2016 Canadian cardiovascular society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can. J. Cardiol. 32, 1263–1282 (2016).
Goff, D. C. Jr. et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 63, 2935–2959 (2014).
World Health Organization. Hearts: technical package for cardiovascular disease management in primary health care (WHO, 2016).
Kernan, W. N. et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45, 2160–2236 (2014).
Pesah, E., Supervia, M., Turk-Adawi, K. & Grace, S. L. A review of cardiac rehabilitation delivery around the world. Prog. Cardiovasc. Dis. 60, 267–280 (2017).
Collins, F. S. & Varmus, H. A new initiative on precision medicine. N. Engl. J. Med. 372, 793–795 (2015).
Becker, C. M., Lee, J. G. L., Hudson, S., Hoover, J. & Civils, D. A. 14-year longitudinal study of the impact of clean indoor air legislation on state smoking prevalence, USA, 1997–2010. Prev. Med. 99, 63–66 (2017).
White, V. M. et al. What impact have tobacco control policies, cigarette price and tobacco control programme funding had on Australian adolescents' smoking? Findings over a 15-year period. Addiction 106, 1493–1502 (2011).
Pulakka, A. et al. Association between distance from home to tobacco outlet and smoking cessation and relapse. JAMA Intern. Med. 76, 1512–1519 (2016).
Briggs, A. D. M. et al. Health impact assessment of the UK soft drinks industry levy: a comparative risk assessment modelling study. Lancet Public Health 2, e15–e22 (2017).
Acknowledgements
M.K.'s work was supported by the UK Medical Research Council (K013351), NordForsk (75021), the Academy of Finland (311492), and a Helsinki Institute of Life Science Fellowship.
Author information
Authors and Affiliations
Contributions
Both authors researched the data for the article, provided substantial contributions to discussions of its content, wrote the article, and undertook review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Kivimäki, M., Steptoe, A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol 15, 215–229 (2018). https://doi.org/10.1038/nrcardio.2017.189
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2017.189
This article is cited by
-
Effect of mindfulness-based interventions on people with prehypertension or hypertension: a systematic review and meta-analysis of randomized controlled trials
BMC Cardiovascular Disorders (2024)
-
CVD phenotyping in oncologic disorders: cardio-miRNAs as a potential target to improve individual outcomes in revers cardio-oncology
Journal of Translational Medicine (2024)
-
Stress-induced stenotic vascular remodeling via reduction of plasma omega-3 fatty acid metabolite 4-oxoDHA by noradrenaline
Scientific Reports (2024)
-
Effects of lifestyle factors on leukocytes in cardiovascular health and disease
Nature Reviews Cardiology (2024)
-
Interrelationship about body composition on sleep quality, physical activity, and heart rate variability in young adults: a cross-sectional study
Sport Sciences for Health (2024)