Key Points
-
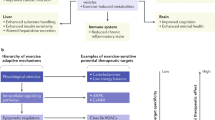
Myokines are proteins or peptides that are upregulated and secreted from skeletal muscle to carry out paracrine or endocrine functions.
-
The concept that stimulated muscle secretes factors that partially mediate the benefits of exercise on health is attractive, as it raises the possibility that these peptides might be manipulated for therapeutic gain.
-
There are many technical hurdles to the discovery of new myokines, but developing methodologies such as proteomics, genetic modification of mice by CRISPR and parabiosis are well suited for myokine discovery and validation.
-
With the increasing realization that brown fat and the 'browning' of adipose tissue represents a therapeutic avenue for treating obesity and metabolic disease, putative myokines irisin and meteorin-like may have a role in this research setting. The myokines interleukin-6 (IL-6) and SPARC (secreted protein acidic and rich in cysteine) have been implicated in the prevention of cancers by exercise.
-
It is anticipated that future research will uncover more novel myokines with the potential to treat diseases that are known to be prevented by regular exercise.
Abstract
Exercise reduces the risk of a multitude of disorders, from metabolic disease to cancer, but the molecular mechanisms mediating the protective effects of exercise are not completely understood. The realization that skeletal muscle is an endocrine organ capable of secreting proteins termed 'myokines', which participate in tissue crosstalk, provided a critical link in the exercise–health paradigm. However, the myokine field is still emerging, and several challenges remain in the discovery and validation of myokines. This Review considers these challenges and highlights some recently identified novel myokines with the potential to be therapeutically exploited in the treatment of metabolic disease and cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pedersen, B. K. & Febbraio, M. A. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 8, 457–465 (2012).
Booth, F. W., Roberts, C. K. & Laye, M. J. Lack of exercise is a major cause of chronic diseases. Comp. Physiol. 2, 1143–1211 (2012).
Hawley, J. A., Hargreaves, M., Joyner, M. J. & Zierath, J. R. Integrative biology of exercise. Cell 159, 738–749 (2014).
Starkie, R., Ostrowski, S., Jauffred, S., Febbraio, M. & Pedersen, B. Exercise and IL-6 infusion inhibit endotoxin-induced TNF-α production in humans. FASEB J. 17, 884–886 (2003).
Walhin, J.-P., Richardson, J., Betts, J. & Thompson, D. Exercise counteracts the effects of short-term overfeeding and reduced physical activity independent of energy imbalance in healthy young men. J. Physiol. 591, 6231–6243 (2013).
Hagobian, T. A. & Braun, B. Interactions between energy surplus and short-term exercise on glucose and insulin responses in healthy people with induced, mild insulin insensitivity. Metabolism 55, 402–408 (2006).
Goldstein, M. S. Humoral nature of the hypoglycemic factor of muscular work. Diabetes 10, 232–234 (1961). The first paper to propose that skeletal muscle might secrete 'exercise factors'.
Febbraio, M. A., Hiscock, N., Sacchetti, M., Fischer, C. P. & Pedersen, B. K. Interleukin-6 is a novel factor mediating glucose homeostasis during skeletal muscle contraction. Diabetes 53, 1643–1648 (2004). A significant finding in the identification of IL-6 as a secreted product of skeletal muscle that carries out endocrine functions.
Pedersen, B. K. & Febbraio, M. A. Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol. Rev. 88, 1379–1406 (2008).
Febbraio, M. A. & Pedersen, B. K. Muscle-derived interleukin-6: mechanisms for activation and possible biological roles. FASEB J. 16, 1335–1347 (2002).
Pal, M., Febbraio, M. A. & Whitham, M. From cytokine to myokine: the emerging role of interleukin-6 in metabolic regulation. Immunol. Cell Biol. 92, 331–339 (2014).
Benatti, F. B. & Pedersen, B. K. Exercise as an anti-inflammatory therapy for rheumatic diseases-myokine regulation. Nat. Rev. Rheumatol. 11, 86–97 (2015).
Görgens, S. W., Eckardt, K., Jensen, J., Drevon, C. A. & Eckel, J. Exercise and regulation of adipokine and myokine production. Prog. Mol. Biol. Transl. Sci. 135, 313–336 (2015).
Schnyder, S. & Handschin, C. Skeletal muscle as an endocrine organ: PGC-1α, myokines and exercise. Bone 80, 115–125 (2015).
Uhlen, M. et al. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Catoire, M., Mensink, M., Kalkhoven, E., Schrauwen, P. & Kersten, S. Identification of human exercise-induced myokines using secretome analysis. Physiol. Genom. 46, 256–267 (2014).
Geiger, T. et al. Initial quantitative proteomic map of twenty-eight mouse tissues using the SILAC mouse. Mol. Cell. Proteom. 12, 1709–1722 (2013).
Su, A. I. et al. A gene atlas of the mouse and human protein-encoding transcriptomes. Proc. Natl Acad. Sci. USA 101, 6062–6067 (2004).
Azimifar, S. B., Nagaraj, N., Cox, J. & Mann, M. Cell-type-resolved quantitative proteomics of murine liver. Cell. Metab. 20, 1076–1087 (2014).
Williams, E. G. et al. Systems proteomics of liver mitochondria function. Science 352, aad0189 (2016).
Kawamoto, S., Matsumoto, Y., Mizuno, K., Okubo, K. & Matsubara, K. Expression profiles of active genes in human and mouse livers. Gene 174, 151–158 (1996).
Steen, H. & Mann, M. The ABC's (and XYZ's) of peptide sequencing. Nat. Rev. Mol. Cell. Biol. 5, 699–711 (2004).
Matthiesen, R. & Bunkenborg, J. Introduction to mass spectrometry-based proteomics. Methods Mol. Biol. 1007, 1–45 (2013).
Hartwig, S. et al. Secretome profiling of primary human skeletal muscle cells. Biochim. Biophys. Acta 1844, 1011–1017 (2014).
Henningsen, J., Rigbolt, K. T., Blagoev, B., Pedersen, B. K. & Kratchmarova, I. Dynamics of the skeletal muscle secretome during myoblast differentiation. Mol. Cell. Proteom. 9, 2482–2496 (2010).
Norheim, F. et al. Proteomic identification of secreted proteins from human skeletal muscle cells and expression in response to strength training. Am. J. Physiol. Endocrinol. Metab. 301, E1013–E1021 (2011).
Henningsen, J., Pedersen, B. K. & Kratchmarova, I. Quantitative analysis of the secretion of the MCP family of chemokines by muscle cells. Mol. Biosyst. 7, 311–321 (2011).
Yoon, J. H. et al. Comparative proteomic analysis of the insulin-induced L6 myotube secretome. Proteomics 9, 51–60 (2009).
Yoon, J. H. et al. Proteomic analysis of the palmitate-induced myotube secretome reveals involvement of the annexin A1-formyl peptide receptor 2 (FPR2) pathway in insulin resistance. Mol. Cell. Proteom. 14, 882–892 (2015).
Chan, C. Y., McDermott, J. C. & Siu, K. W. Secretome analysis of skeletal myogenesis using SILAC and shotgun proteomics. Int. J. Proteom. 2011, 329467 (2011).
Raschke, S., Eckardt, K., Bjørklund Holven, K., Jensen, J. & Eckel, J. Identification and validation of novel contraction-regulated myokines released from primary human skeletal muscle cells. PLoS ONE 8, e62008 (2013).
Haugen, F. et al. IL-7 is expressed and secreted by human skeletal muscle cells. Am. J. Physiol. Cell Physiol. 298, C807–C816 (2010).
Deshmukh, A. S. et al. Deep proteomics of mouse skeletal muscle enables quantitation of protein isoforms, metabolic pathways, and transcription factors. Mol. Cell. Proteom. 14, 841–853 (2015). The deepest quantitation of the skeletal muscle proteome thus far and an insight into the power of discovery-based proteomics.
Anderson, N. L. & Anderson, N. G. The human plasma proteome: history, character, and diagnostic prospects. Mol. Cell. Proteom. 1, 845–867 (2002).
Omenn, G. S. et al. Overview of the HUPO Plasma Proteome Project: results from the pilot phase with 35 collaborating laboratories and multiple analytical groups, generating a core dataset of 3020 proteins and a publicly-available database. Proteomics 5, 3226–3245 (2005).
States, D. J. et al. Challenges in deriving high-confidence protein identifications from data gathered by a HUPO plasma proteome collaborative study. Nat. Biotechnol. 24, 333–338 (2006).
Pernemalm, M., Lewensohn, R. & Lehtio, J. Affinity prefractionation for MS-based plasma proteomics. Proteomics 9, 1420–1427 (2009).
Liu, X. et al. Mapping the human plasma proteome by SCX-LC-IMS-MS. J. Am. Soc. Mass Spectrom. 18, 1249–1264 (2007).
Pocsfalvi, G. et al. Mass spectrometry of extracellular vesicles. Mass Spectrom. Rev. 35, 3–21 (2015).
Harel, M., Oren-Giladi, P., Kaidar-Person, O., Shaked, Y. & Geiger, T. Proteomics of microparticles with SILAC Quantification (PROMIS-Quan): a novel proteomic method for plasma biomarker quantification. Mol. Cell. Proteom. 14, 1127–1136 (2015).
Forterre, A. et al. Proteomic analysis of C2C12 myoblast and myotube exosome-like vesicles: a new paradigm for myoblast-myotube cross talk? PLoS ONE 9, e84153 (2014).
Kalra, H. et al. Vesiclepedia: a compendium for extracellular vesicles with continuous community annotation. PLoS Biol. 10, e1001450 (2012).
Lancaster, G. I. & Febbraio, M. A. Exosome-dependent trafficking of HSP70: a novel secretory pathway for cellular stress proteins. J. Biol. Chem. 280, 23349–23355 (2005).
Steensberg, A. et al. Production of interleukin-6 in contracting human skeletal muscles can account for the exercise-induced increase in plasma interleukin-6. J. Physiol. 529, 237–242 (2000).
Wiles, M. V., Qin, W., Cheng, A. W. & Wang, H. CRISPR–Cas9-mediated genome editing and guide RNA design. Mamm. Genome 26, 501–510 (2015).
Yang, Y. et al. A dual AAV system enables the Cas9-mediated correction of a metabolic liver disease in newborn mice. Nat. Biotechnol. 34, 334–338 (2016).
Kamran, P. et al. Parabiosis in mice: a detailed protocol. J. Vis. Exp. http://dx.doi.org/10.3791/50556 (2013).
Chambers, A. G., Percy, A. J., Simon, R. & Borchers, C. H. MRM for the verification of cancer biomarker proteins: recent applications to human plasma and serum. Exp. Rev. Proteom. 11, 137–148 (2014).
Peterson, A. C., Russell, J. D., Bailey, D. J., Westphall, M. S. & Coon, J. J. Parallel reaction monitoring for high resolution and high mass accuracy quantitative, targeted proteomics. Mol. Cell. Proteom. 11, 1475–1488 (2012).
Horsley, V., Jansen, K. M., Mills, S. T. & Pavlath, G. K. IL-4 acts as a myoblast recruitment factor during mammalian muscle growth. Cell 113, 483–494 (2003).
Nieman, D. C. et al. Carbohydrate ingestion influences skeletal muscle cytokine mRNA and plasma cytokine levels after a 3-h run. J. Appl. Physiol. 94, 1917–1925 (2003).
Ouchi, N. et al. Follistatin-like 1, a secreted muscle protein, promotes endothelial cell function and revascularization in ischemic tissue through a nitric-oxide synthase-dependent mechanism. J. Biol. Chem. 283, 32802–32811 (2008).
Hamrick, M. W., McNeil, P. L. & Patterson, S. L. Role of muscle-derived growth factors in bone formation. J. Musculoskelet. Neuronal Interact. 10, 64–70 (2010).
McPherron, A. C., Lawler, A. M. & Lee, S. J. Regulation of skeletal muscle mass in mice by a new TGF-β superfamily member. Nature 387, 83–90 (1997).
Hittel, D. S., Berggren, J. R., Shearer, J., Boyle, K. & Houmard, J. A. Increased secretion and expression of myostatin in skeletal muscle from extremely obese women. Diabetes 58, 30–38 (2009).
McPherron, A. C. & Lee, S. J. Suppression of body fat accumulation in myostatin-deficient mice. J. Clin. Invest. 109, 595–601 (2002).
Wilkes, J. J., Lloyd, D. J. & Gekakis, N. Loss-of-function mutation in myostatin reduces tumor necrosis factor α production and protects liver against obesity-induced insulin resistance. Diabetes 58, 1133–1143 (2009).
Camporez, J-. P. G. et al. Anti-myostatin antibody increases muscle mass and strength and improves insulin sensitivity in old mice. Proc. Natl Acad. Sci. USA 113, 2212–2217 (2016).
Moon, H. Y. et al. Running-induced systemic cathepsin B secretion is associated with memory function. Cell. Metab. http://dx.doi.org/10.1016/j.cmet.2016.05.025 (2016).
Bartelt, A. & Heeren, J. Adipose tissue browning and metabolic health. Nat. Rev. Endocrinol. 10, 24–36 (2014).
Cousin, B. et al. Occurrence of brown adipocytes in rat white adipose tissue: molecular and morphological characterization. J. Cell Sci. 103, 931–942 (1992).
Barbatelli, G. et al. The emergence of cold-induced brown adipocytes in mouse white fat depots is determined predominantly by white to brown adipocyte transdifferentiation. Am. J. Physiol. Endocrinol. Metab. 298, E1244–E1253 (2010).
Yoshida, T. et al. Nicotine induces uncoupling protein 1 in white adipose tissue of obese mice. Int. J. Obes. Relat. Metab. Disord. 23, 570–575 (1999).
Boström, P. et al. A PGC1-α-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 481, 463–468 (2012).
Lin, J. et al. Transcriptional co-activator PGC-1α drives the formation of slow-twitch muscle fibres. Nature 418, 797–801 (2002).
Raschke, S. et al. Evidence against a beneficial effect of irisin in humans. PLoS ONE 8, e73680 (2013).
Albrecht, E. et al. Irisin – a myth rather than an exercise-inducible myokine. Sci. Rep. 5, 8889 (2015).
Erickson, H. P. Irisin and FNDC5 in retrospect: an exercise hormone or a transmembrane receptor? Adipocyte 2, 289–293 (2013).
Schumacher, M. A., Chinnam, N., Ohashi, T., Shah, R. S. & Erickson, H. P. The structure of irisin reveals a novel intersubunit β-sheet fibronectin type III (FNIII) dimer: implications for receptor activation. J. Biol. Chem. 288, 33738–33744 (2013).
Jedrychowski, M. P. et al. Detection and quantitation of circulating human irisin by tandem mass spectrometry. Cell. Metab. 22, 734–740 (2015). An example of how targeted proteomics can validate myokine expression in exercise contexts.
Lee, P. et al. Irisin and FGF21 are cold-induced endocrine activators of brown fat function in humans. Cell. Metab. 19, 302–309 (2014).
Rao, R. R. et al. Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell 157, 1279–1291 (2014).
Izumiya, Y., Hopkins, T., Morris, C., Sato, K. & Zeng, L. Fast/glycolytic muscle fiber growth reduces fat mass and improves metabolic parameters in obese mice. Cell. Metab. 7, 159–172 (2008).
Izumiya, Y. et al. FGF21 is an Akt-regulated myokine. FEBS Lett. 582, 3805–3810 (2008).
Kim, K. H. et al. Acute exercise induces FGF21 expression in mice and in healthy humans. PLoS ONE 8, e63517 (2013).
Kharitonenkov, A. et al. FGF-21 as a novel metabolic regulator. J. Clin. Invest. 115, 1627–1635 (2005).
Coskun, T. et al. Fibroblast growth factor 21 corrects obesity in mice. Endocrinology 149, 6018–6027 (2008).
Hansen, J. S. et al. Glucagon-to-insulin ratio is pivotal for splanchnic regulation of FGF-21 in humans. Mol. Met. 4, 551–560 (2015). An insightful examination of the source of circulating FGF21 during exercise.
Markan, K. R. et al. Circulating FGF21 is liver derived and enhances glucose uptake during refeeding and overfeeding. Diabetes 63, 4057–4063 (2014).
Hondares, E. et al. Thermogenic activation induces FGF21 expression and release in brown adipose tissue. J. Biol. Chem. 286, 12983–12990 (2011).
Fisher, F. M. et al. FGF21 regulates PGC-1α and browning of white adipose tissues in adaptive thermogenesis. Genes Dev. 26, 271–281 (2012).
Samms, R. J. et al. Discrete aspects of FGF21 in vivo pharmacology do not require UCP1. Cell Rep. 11, 991–999 (2015).
Véniant, M. M. et al. Pharmacologic effects of FGF21 are independent of the “browning” of white adipose tissue. Cell. Metab. 21, 731–738 (2015).
Degirolamo, C., Sabbà, C. & Moschetta, A. Therapeutic potential of the endocrine fibroblast growth factors FGF19, FGF21 and FGF23. Nat. Rev. Drug. Discov. 15, 51–69 (2016).
Roberts, L. D. et al. β-Aminoisobutyric acid induces browning of white fat and hepatic β-oxidation and is inversely correlated with cardiometabolic risk factors. Cell. Metab. 19, 96–108 (2014).
Seldin, M. M., Peterson, J. M., Byerly, M. S., Wei, Z. & Wong, G. W. Myonectin (CTRP15), a novel myokine that links skeletal muscle to systemic lipid homeostasis. J. Biol. Chem. 287, 11968–11980 (2012).
Seldin, M. M. et al. Skeletal muscle-derived myonectin activates the mammalian target of rapamycin (mTOR) pathway to suppress autophagy in liver. J. Biol. Chem. 288, 36073–36082 (2013).
Yang, L., Li, P., Fu, S., Calay, E. S. & Hotamisligil, G. S. Defective hepatic autophagy in obesity promotes ER stress and causes insulin resistance. Cell. Metab. 11, 467–478 (2010).
Leitzmann, M. et al. European Code against Cancer 4th Edition: physical activity and cancer. Cancer Epidemiol. 39 (Suppl. 1), 46–55 (2015).
Brown, J. C., Winters-Stone, K., Lee, A. & Schmitz, K. H. Cancer, physical activity, and exercise. Comp. Physiol. 2, 2775–2809 (2012).
Goh, J. et al. Exercise training in transgenic mice is associated with attenuation of early breast cancer growth in a dose-dependent manner. PLoS ONE 8, e80123 (2013).
Pedersen, L. et al. Voluntary running suppresses tumor growth through epinephrine- and IL-6-dependent NK cell mobilization and redistribution. Cell. Metab. 23, 554–562 (2016). A comprehensive demonstration that voluntary wheel running in mouse models of cancer is a beneficial effect partially mediated by the myokine IL-6.
Hojman, P. et al. Exercise-induced muscle-derived cytokines inhibit mammary cancer cell growth. Am. J. Physiol. Endocrinol. Metab. 301, E504–E510 (2011).
Aoi, W. et al. A novel myokine, secreted protein acidic and rich in cysteine (SPARC), suppresses colon tumorigenesis via regular exercise. Gut 62, 882–889 (2013).
Kanzleiter, T. et al. The myokine decorin is regulated by contraction and involved in muscle hypertrophy. Biochem. Biophys. Res. Comm. 450, 1089–1094 (2014).
Soria-Valles, C. et al. The anti-metastatic activity of collagenase-2 in breast cancer cells is mediated by a signaling pathway involving decorin and miR-21. Oncogene 33, 3054–3063 (2014).
Araki, K. et al. Decorin suppresses bone metastasis in a breast cancer cell line. Oncology 77, 92–99 (2009).
Laye, M. J. et al. Cessation of daily wheel running differentially alters fat oxidation capacity in liver, muscle, and adipose tissue. J. Appl. Physiol. 106, 161–168 (2009).
Carotta, S. Targeting, N. K. Cells for anticancer immunotherapy: clinical and preclinical approaches. Front. Immunol. 7, 152 (2016).
Morikawa, T. et al. Prospective analysis of body mass index, physical activity, and colorectal cancer risk associated with β-catenin (CTNNB1) status. Cancer Res. 73, 1600–1610 (2013).
Je, Y., Jeon, J. Y., Giovannucci, E. L. & Meyerhardt, J. A. Association between physical activity and mortality in colorectal cancer: a meta-analysis of prospective cohort studies. Int. J. Cancer 133, 1905–1913 (2013).
Murphy-Ullrich, J. E. & Sage, E. H. Revisiting the matricellular concept. Matrix Biol. 37, 1–14 (2014).
Brekken, R. A. et al. Enhanced growth of tumors in SPARC null mice is associated with changes in the ECM. J. Clin. Invest. 111, 487–495 (2003).
Neill, T., Schaefer, L. & Iozzo, R. V. Decorin: a guardian from the matrix. Am. J. Pathol. 181, 380–387 (2012).
Rahman, M., Chan, A. P. K. & Tai, I. T. A peptide of SPARC interferes with the interaction between caspase8 and Bcl2 to resensitize chemoresistant tumors and enhance their regression in vivo. PLoS ONE 6, e26390 (2011).
Nishizawa, H. et al. Musclin, a novel skeletal muscle-derived secretory factor. J. Biol. Chem. 279, 19391–19395 (2004).
Subbotina, E. et al. Musclin is an activity-stimulated myokine that enhances physical endurance. Proc. Natl Acad. Sci. USA 112, 16042–16047 (2015).
Myers, J. et al. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 346, 793–801 (2002).
Korpelainen, R. et al. Exercise capacity and mortality - a follow-up study of 3033 subjects referred to clinical exercise testing. Ann. Med. http://dx.doi.org/10.1080/07853890.2016.1178856 (2016).
Lua, L. H. L. & Chuan, Y. P. in Biopharmaceutical Production Technology Vol. 1 & Vol. 2 43–77 (Wiley-VCH Verlag GmbH & Co. KGaA, 2012).
Pisal, D. S., Kosloski, M. P. & Balu-Iyer, S. V. Delivery of therapeutic proteins. J. Pharm. Sci. 99, 2557–2575 (2010).
Harris, J. M. & Chess, R. B. Effect of pegylation on pharmaceuticals. Nat. Rev. Drug. Discov. 2, 214–221 (2003).
Jazayeri, J. A. & Carroll, G. J. Fc-based cytokines: prospects for engineering superior therapeutics. Biodrugs 22, 11–26 (2008).
Huang, C. Receptor-Fc fusion therapeutics, traps, and MIMETIBODY technology. Curr. Opin. Biotechnol. 20, 692–699 (2009).
Rath, T. et al. Fc-fusion proteins and FcRn: structural insights for longer-lasting and more effective therapeutics. Crit. Rev. Biotechnol. 35, 235–254 (2015).
Panyam, J. & Labhasetwar, V. Biodegradable nanoparticles for drug and gene delivery to cells and tissue. Adv. Drug. Deliv. Rev. 55, 329–347 (2003).
Davis, M. E., Chen, Z. G. & Shin, D. M. Nanoparticle therapeutics: an emerging treatment modality for cancer. Nat. Rev. Drug. Discov. 7, 771–782 (2008).
Popielarski, S. R., Hu-Lieskovan, S., French, S. W., Triche, T. J. & Davis, M. E. A nanoparticle-based model delivery system to guide the rational design of gene delivery to the liver. 2. In vitro and in vivo uptake results. Bioconjug. Chem. 16, 1071–1080 (2005).
Febbraio, M. A. gp130 receptor ligands as potential therapeutic targets for obesity. J. Clin. Invest. 117, 841–849 (2007).
Ostrowski, K., Rohde, T., Zacho, M., Asp, S. & Pedersen, B. Evidence that interleukin-6 is produced in human skeletal muscle during prolonged running. J. Physiol. 508, 949–953 (1998).
Febbraio, M. A. et al. Hepatosplanchnic clearance of interleukin-6 in humans during exercise. Am. J. Physiol. Endocrinol. Metab. 285, E397–E402 (2003).
Hiscock, N., Chan, M., Bisucci, T., Darby, I. & Febbraio, M. Skeletal myocytes are a source of interleukin-6 mRNA expression and protein release during contraction: evidence of fiber type specificity. FASEB J. 18, 992–994 (2004).
Starkie, R. L., Arkinstall, M. J., Koukoulas, I., Hawley, J. A. & Febbraio, M. A. Carbohydrate ingestion attenuates the increase in plasma interleukin-6, but not skeletal muscle interleukin-6 mRNA, during exercise in humans. J. Physiol. 533, 585–591 (2001).
Steensberg, A. et al. Interleukin-6 production in contracting human skeletal muscle is influenced by pre-exercise muscle glycogen content. J. Physiol. 537, 633–639 (2001).
Richter, E. A. & Galbo, H. Diabetes, insulin and exercise. Sports Med. 3, 275–288 (1986).
Wasserman, D. H. Regulation of glucose fluxes during exercise in the postabsorptive state. Annu. Rev. Physiol. 57, 191–218 (1995).
Whitham, M. et al. Contraction-induced interleukin-6 gene transcription in skeletal muscle is regulated by c-Jun terminal kinase/activator protein-1. J. Biol. Chem. 287, 10771–10779 (2012).
Kelly, M. et al. AMPK activity is diminished in tissues of IL-6 knockout mice: the effect of exercise. Biochem. Biophys. Res. Comm. 320, 449–454 (2004).
Al-Khalili, L. et al. Signaling specificity of interleukin-6 action on glucose and lipid metabolism in skeletal muscle. Mol. Endocrinol. 20, 3364–3375 (2006).
Carey, A. L. et al. Interleukin-6 increases insulin-stimulated glucose disposal in humans and glucose uptake and fatty acid oxidation in vitro via AMP-activated protein kinase. Diabetes 55, 2688–2697 (2006).
Petersen, A. M. & Pedersen, B. K. The anti-inflammatory effect of exercise. J. Appl. Physiol. 98, 1154–1162 (2005).
van Hall, G. et al. Interleukin-6 stimulates lipolysis and fat oxidation in humans. J. Clin. Endocrinol. Metab. 88, 3005–3010 (2003).
Ellingsgaard, H. et al. Interleukin-6 enhances insulin secretion by increasing glucagon-like peptide-1 secretion from L cells and alpha cells. Nat. Med. 17, 1481–1489 (2011).
Shirazi, R. et al. Glucagon-like peptide 1 receptor induced suppression of food intake, and body weight is mediated by central IL-1 and IL-6. Proc. Natl Acad. Sci. USA 110, 16199–16204 (2013).
ALS CNTF Treatment Study Group. A double-blind placebo-controlled clinical trial of subcutaneous recombinant human ciliary neurotrophic factor (rHCNTF) in amyotrophic lateral sclerosis. Neurology 46, 1244–1249 (1996).
Duff, E. & Baile, C. A. Ciliary neurotrophic factor: a role in obesity? Nutr. Rev. 61, 423–426 (2003).
Ettinger, M. P. et al. Recombinant variant of ciliary neurotrophic factor for weight loss in obese adults: a randomized, dose-ranging study. J. Am. Med. Assoc. 289, 1826–1832 (2003).
Kraakman, M. et al. Targeting gp130 to prevent inflammation and promote insulin action. Diabetes Obes. Metab. 15 (Suppl. 3), 170–175 (2013).
Tsiloulis, T. & Watt, M. J. Exercise and the regulation of adipose tissue metabolism. Prog. Mol. Biol. Transl. Sci. 135, 175–201 (2015).
Vosselman, M. J. et al. Low brown adipose tissue activity in endurance-trained compared with lean sedentary men. Int. J. Obes. 39, 1696–1702 (2015).
Acknowledgements
M.W. and M.A.F. are supported by the National Health and Medical Research Council of Australia (NHMRC Project Grant APP1062436 to M.A.F and M.W; Research Fellowship APP11021168 to M.A.F.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
M.A.F is a holder of patents for IC7, a gp130 receptor ligand.
Glossary
- VO2max
-
The term given to the maximal oxygen uptake; an indicator of aerobic capacity and cardiorespiratory fitness.
- Myokine
-
A cytokine or peptide that is produced by skeletal muscle cells and subsequently released into the circulation to exert paracrine or endocrine effects.
- Omics
-
A term given to the comprehensive biological assessment of entities with the suffix 'ome', such as the geneome, transcriptome and proteome (or proteinome).
- Liquid chromatography tandem mass spectrometry
-
(LC–MS/MS). A technique used to identify proteins in complex mixtures via ionization and manipulation of the resultant ions to derive amino acid sequence information.
- CRISPR
-
A gene editing tool that facilitates the establishment of genetically modified rodent models.
- Adeno-associated viruses
-
Methods of gene transfer, in vivo, used to create transgenic overexpression mouse models in specific tissues.
- Parabiosis
-
A mouse model of shared circulation, whereby surgical suturing initiates skin-to-skin contact of paired mice. After a period of 2 weeks, inflammation induces the development of microcirculation between mice so that the effect of a circulating factor from one animal can be assessed in the partner animal.
- AMP-activated protein kinase
-
(AMPK). A kinase that is considered to be a master regulator of metabolism by sensing changes in AMP:ATP ratio.
- PPARγ coactivator 1α
-
(PGC1α). A transcription factor that regulates genes involved in energy metabolism, of which there are at least four variants (PGC1α1 to PGC1α4).
- PEGylation
-
Process of covalently adding repeating units of (polymerized) ethelene glycol to proteins with a view to improving stability, pharmacokinetics and therapeutic utility.
- Fc fusion
-
Addition of the crystallizable fragment (Fc) domain of IgG molecules to therapeutic agents to improve pharmacokinetics and pharmacodynamics.
Rights and permissions
About this article
Cite this article
Whitham, M., Febbraio, M. The ever-expanding myokinome: discovery challenges and therapeutic implications. Nat Rev Drug Discov 15, 719–729 (2016). https://doi.org/10.1038/nrd.2016.153
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrd.2016.153
This article is cited by
-
Meteorin-like protein overexpression ameliorates fulminant hepatitis in mice by inhibiting chemokine-dependent immune cell infiltration
Acta Pharmacologica Sinica (2023)
-
Körperliche Aktivität im Kontext Diabetes mellitus
Die Diabetologie (2023)
-
Circadian rhythms and cancers: the intrinsic links and therapeutic potentials
Journal of Hematology & Oncology (2022)
-
A systematic review and meta-analysis demonstrating Klotho as an emerging exerkine
Scientific Reports (2022)
-
Exercise serum regulates uric acid transporters in normal rat kidney cells
Scientific Reports (2022)