Key Points
-
T cells constantly survey the body for signs of infection or malignancy through the recognition of fragments of antigens (peptides) complexed to molecules of the major histocompatibility complex.
-
These peptides (T-cell epitopes) are more diverse than originally thought.
-
Vaccine design must take into account both chemical modifications to antigens and heterogeneous length of these important targets of immunity, as well as the challenge of the diversity in human immunogenetics.
-
Peptide-based vaccines offer excellent alternatives to traditional vaccination approaches because of the ease with which chemical modifications can be introduced.
-
Peptide-based vaccines can be modified to produce peptide mimotopes with enhanced stability, thereby allowing for the precise delivery of the vaccine constituents with fixed peptide length and chemical fidelity.
-
Vaccines of the future will require a systematic approach to tailor the desired immune response to individuals. Advances in the identification of patient specific epitopes, and delivery, stability and design of peptide therapeutics will open new avenues for vaccine design.
Abstract
The use of peptides as therapeutics is experiencing renewed enthusiasm owing to advances in delivery, stability and design. Moreover, there is a growing emphasis on the use of peptides in vaccine design as insights into tissue-specific processing of the immunogenic epitopes of proteins and the discovery of unusually long cytotoxic T-lymphocyte epitopes broaden the range of targets and give clues to enhancing peptide immunogenicity. Peptides can also be synthesized with known post-translational modifications and/or deliberately introduced protease-resistant peptide bonds to regulate their processing independent of tissue-specific proteolysis and to stabilize these compounds in vivo. We discuss the potential of peptide-based vaccines for the treatment of chronic viral diseases and cancer, and review recent developments in the field of peptide-based vaccines.
Similar content being viewed by others
Main
Vaccination is one of the most successful public health initiatives ever achieved, with the global eradication of diseases such as smallpox and the virtual eradication of poliomyelitis. Despite such noteworthy successes, vaccines for many diseases remain elusive and as such several strategies have been devised to deliver specific and immunogenic vaccine components to the immune system in the hope of eliciting a therapeutic or prophylactic immune response. Traditionally, vaccines have consisted of live attenuated microorganisms or inactivated microorganisms delivered by injection. However, many pathogenic microorganisms are difficult to culture in vitro, and therefore production of live attenuated or inactivated vaccines of these pathogens are impractical. Moreover, features of even attenuated microorganisms may result in detrimental immune responses, or the pathogen may contain material that initiates unwanted host responses. As our knowledge of the targets of immune responses has grown, so too has the sophistication with which vaccines are designed and delivered. Thus, it is often a beneficial strategy to select particular protein antigens from the microorganism for inclusion into recombinant vaccines. Focusing on a limited set of antigens is also relevant to cancer vaccination in which tumour cells or lysates may contain predominantly normal self-proteins that are of no therapeutic benefit, or contain material that potentially carries the capacity to induce further malignancy. Therefore, the identification and administration of tumour-specific antigens rather than crude tumour preparations is also highly desirable in this case.
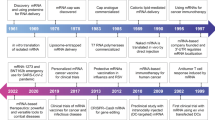
Taking this reductionist approach one step further, the most precise selection of vaccine components exists in epitope-based peptide vaccines, which are the subject of this Review. These peptide epitopes represent the minimal immunogenic region of a protein antigen and allow for precise direction of immune responses. As yet, there are no human peptide-based vaccines on the market — this stems primarily from the difficulties associated with peptide stability and delivery, and the challenge posed by the diversity of human immunogenetics. However, similar to therapeutic peptides that have been investigated for other indications, strategies have become available to modify peptides to enhance both their immunogenicity and stability, which will be discussed below. Given the long development time experienced with therapeutic peptides, and their recent emergence into the pharmaceutical arena, it is likely that peptide-based vaccines will enter the human therapeutics marketplace in the near future. Several such vaccines are currently in development (Table 1a,b).
In this Review, after briefly introducing the key immunological concepts of vaccine design, we will discuss the latest developments in the design of peptide vaccines that have led to the return of epitope-based strategies to the forefront of vaccine design.
Key concepts of peptide vaccine immunology
The adaptive immune system comprises two arms, one that is responsible for the cytotoxic immune response and one for the humoral immune response. Cytotoxic T lymphocytes (CTLs; also referred to as CD8+ T cells) eradicate infected cells or tumour cells through direct cytotoxic action on these targets. B cells are the main players of the humoral immune response and generate antibodies towards pathogen-derived molecules. Both processes are further dependent on T-helper cells (TH cells; also referred to as CD4+ T cells). CTLs detect infected or malignant cells through the recognition of major histocompatibility complex class I (MHC class I) molecules that are complexed with peptides derived from proteins expressed within the cell. TH cells recognize MHC class II molecules that are complexed to peptides derived from predominantly exogenous proteins. All nucleated cells present peptides that are derived from intracellular proteins on their surface bound to MHC I, whereas peptides derived from extracellular proteins are mainly presented by MHC II on specialized antigen-presenting cells (APCs), such as dendritic cells and macrophages. In both cases the T-cell receptor (TCR) on the surface of the CTL or TH-cell forms a complex with the MHC I/peptide-epitope complex or the MHC II/peptide-epitope complex, respectively; these interactions are aided by the CD8/CD4 co-receptors, respectively. The intricate interplay of these peptide-dependent recognition processes results in the propagation of immune responses that control infection and cancer in humans as depicted in Fig. 1. The goal of vaccination is to induce immunity towards these states by selectively stimulating antigen-specific CTLs or B cells and TH cells. A vaccine must therefore contain two antigenic epitopes: a TH-epitope and an epitope that will either induce specific B-cell or CTL responses. In some cases these can overlap substantially within the sequence of an antigen, and in others they might be present in discrete regions of the antigen or present in different antigens from the targeted pathogen.
The first step in the generation of an antibody response is the uptake of an immunogen by an antigen-presenting cell (APC). Antigens undergo proteolysis to form peptides, some of which are bound by major histocompatibility complex (MHC) class II molecules that are then transported to the APC surface. T-helper cells (TH cells; also known as CD4+ T cells) that bear receptors capable of interacting with the peptide/MHC II complexes can then interact with the APC (a). Additional interactions occur through co-stimulatory molecules that are expressed on APCs and their ligands on the TH-cell. These recognition events result in the transmission of activation signals to the TH-cell, and the activated TH-cell is now poised to respond to those B cells that display the same peptide/MHC II complexes on their surfaces, acquired as a result of the internalization of the immunogen through specific surface-immunoglobulin receptors (for example, B-cell antigen receptors (BCRs) (b). It is this interaction between TH cells and B cells that is termed 'help,' and results in the triggering of the B-cell to differentiate into a plasma cell that is capable of secreting antibody of the same specificity as that of the immunoglobulin receptor. The interaction of activated TH cells with certain subsets of APC can also bring these to a state capable of stimulating naive CD8+ T cells (c). Presentation of appropriate peptide epitopes to a naive CD8+ T cell by an activated APC results in the generation of cytotoxic T cells (CTLs) that are able to recognize and kill target cells that display a viral or tumour peptide in the context of MHC class I molecules (d). Cytokines are also produced by each cell type, which profoundly influence the type of immune response that is elicited.
Synthetic peptides as vaccines
Compared with conventional vaccines, which are based on attenuated or inactivated microorganisms, synthetic peptides offer several advantages over other forms of vaccines, particularly with regards to safety and ease of production (Box 1). However, drawbacks include poor immunogenicity of the simple peptides and the need to potently stimulate T cells and elicit immunological memory. Adjuvant science, lipopeptide conjugation and direct delivery to dendritic cells are some of the approaches currently being used to overcome these problems (see Box 2 and below).
Use of epitope-based vaccines are also restricted to patients of a given tissue type (human leukocyte antigen (HLA) haplotype), and as such need to be tailored to accommodate the natural variation in HLA genes. Although initially thought to be a major impediment, new technologies have made this personalized-medicine approach feasible1. Moreover, the existence of HLA supertypes can simplify the use of epitope-based vaccines that target MHC-I-restricted cytotoxic T cells to essentially nine superfamilies with shared peptide-binding specificity and shared epitope presentation (Supplementary information S1 (table)). Supertype motifs generally allow for a significant reduction in the number of epitopes required to give excellent population coverage for a given pathogen; however, it should be noted that supertypes are not always predictive of stable peptide binding and significant variations, even between closely related alleles, can occur2,3,4. The binding of class II MHC ligands is more promiscuous and as such motifs have been difficult to delineate with any reliability. An alternative approach to the delivery of peptides with a broad relevance to different HLA allotypes is to use longer peptides and to rely on their accurate processing to shorter allele-specific peptides. The use of longer peptide precursors is not always desirable as tissue-specific processing and the frequent non-concordance of processing of longer exogenous peptides compared with endogenous antigens can result in unwanted immune responses (disussed in more detail later).
The administration of a peptide epitope taken out of context of the whole antigen can be challenging as the exogenously administered peptide will not necessarily follow the same pathway of processing as the native pathogen or the cancer-cell derived antigen, and consequently might not elicit the same type of immune responses (Box 3). Furthermore, in order to activate B cells to generate a specific antibody response to a given antigen, the peptide epitope needs to possess a conformation that is similar to that of the native antigen. Several approaches are available to induce peptides to fold correctly5, but any approach in which conformational elements are incorporated requires some knowledge of the structure of the native antigen. The induction of CTL responses on the other hand has little requirement for epitope conformation, and simple peptide epitopes composed of 8–10 amino acids are able to induce cytotoxic responses. As the induction of CTL and B-cell responses are generally dependent on the additional stimulation of TH cells, a typical approach to peptide-epitope vaccine design is to covalently couple the antibody or CTL epitope to a carrier protein, such as tetanus toxoid, which provides a source of TH epitopes. In a clinical setting, the provision of T-cell help is more readily achieved using defined TH epitopes that are matched to the haplotype of the patient5.
Peptide binding to MHC I. CTLs are generally activated by antigens that are derived from intracellular proteins, which are presented in a complex with MHC I on the surface of cells. Intracellular proteins (for example, viral proteins) are degraded to oligopeptides in the cytoplasm through the action of a multicatalytic protease structure known as the proteasome. These peptides are transported into the lumen of the endoplasmic reticulum where they assemble with MHC I and transit through the Golgi to the cell surface (Box 3). The path that exogenously administered extracellular peptides follow post-immunization is poorly understood, although it appears that the extracellular environment is rich in proteases and peptides are rapidly cleared from the body. Peptide-based vaccination strategies therefore must take into account the inherent instability of native peptides. Importantly, to design effective peptide-epitope-based vaccines, the requirements for their incorporation into the MHC I/peptide complex need to be better understood.
MHC I molecules consist of a polymorphic heavy chain, a monomorphic light chain (β2 microglobulin) and an antigenic peptide ligand (corresponding to the antigenic epitope of a given protein). The heavy chain forms an antigen-binding groove that can accommodate antigenic peptides that are typically 8–10 amino-acid residues in length (Supplementary information S2 (figure)). Amino-acid residues that line the binding groove are the focus for most MHC polymorphisms that determine the peptide-binding specificity of allelic forms of MHC molecules. Structural and biochemical studies of bound peptides have contributed significantly to our knowledge of the binding characteristics of different HLA (MHC I) alleles (Supplementary information S1 (table)). In particular, these studies have highlighted the role of conserved amino acids at different positions of all allele-specific peptide ligands that are involved in binding to the cleft of MHC I molecules (anchor residues). The studies have also highlighted the role of the more variable amino acids at other positions within the peptide that project out of the antigen-binding cleft and make crucial specificity-determining contacts with receptors on the surface of T cells. This approach has allowed the identification of specific binding motifs, which have been used to successfully predict T-cell epitopes. Listings of motifs are conveniently web based (for example, SYFPEITHI, a database of MHC ligands and peptide motifs). However, the success rate for de novo prediction of T-cell epitopes, even for well-studied and abundant MHC alleles, is only about 60% for many alleles (and for new alleles or MHC I molecules from poorly studied ethnic populations no binding motifs are available). However, recent studies have improved the predictive capacity of algorithms for some well-studied alleles substantially3,6,7,8,9,10. Reasons for poor predictability include the occurrence of non-motif-based ligands, peptides of unusual length, post-translationally modified ligands or the failure of antigen processing to liberate the predicted peptides7,11,12,13,14,15,16,17. Furthermore, many T-cell responses are focused on one or two immunodominant peptides that are selected from the numerous potential MHC ligands of a given pathogen18. The participation of so few epitopes limits the number of distinct epitopes that are required in a peptide-based vaccine to elicit a protective immune response. Thus, predictive markers of immunogenicity must take into account not only peptide binding but also the abundance and density of the antigen that is present on the cell surface; the time of expression of the antigen during the infection or pathological process; the correct processing and luminal transport of the epitope; and the available T-cell repertoire in the host organism. Nonetheless, epitope prediction remains a popular first-screening method to identify candidate T-cell determinants for subsequent biological validation, and predictive algorithms are frequently combined with in vitro MHC-binding assays to confirm that the predicted ligands bind to the targeted MHC molecule19,20.
Peptide binding to MHC II. The humoral immune response (antibody production by B cells) is generally induced in response to extracellular antigens, which are presented in a complex with MHC II on the surface of APCs (for example, dendritic cells, macrophages and B cells). In cells that are capable of receptor-mediated uptake of immune complexes (for example, Fc-receptor-positive cells), exogenous antigen is endocytosed via receptor-mediated processes and degraded in the early and late endosomes. These compartments are also the destination of antigens that are taken up less selectively by highly phagocytic APC-like dendritic cells and macrophages. The late endosomes therefore provide a rich reservoir of antigenic peptides that are transported to the cell surface for display and scrutiny by TH cells. This process is mechanistically and physically distinct from the MHC-class-I-processing pathway (Fig. 2). Likewise, MHC II is physically distinct from MHC I and is composed of two polymorphic polypeptide chains (α and β) that form an αβ heterodimer, which forms a binding cleft that accommodates peptide antigen. B cells that bind to a given antigen via their clonally distributed surface-immunoglobulin receptor, and display a specific MHC II/peptide complex by virtue of the capture of antigen, can be triggered to differentiate into antibody-producing plasma cells with the help of TH cells (Fig. 1).
Processing of intact exogenous antigen and peptide vaccines is similar, and both are loaded onto the major histocompatibility complex (MHC) class II molecules. Similar to MHC-I-targeted epitopes, peptide antigens can access surface MHC II molecules and replace existing peptides by a surface-exchange mechanism113,114,115 (a). Peptide that is administered outside the context of the native antigen will be subjected to an array of cell-surface and extracellular proteases during this process. Exogenous antigen and peptide vaccines are taken up into the endosomal pathway by macropinocytosis or by receptor-mediated events, such as B-cell-surface-immunoglobulin uptake of antigen or Fc-receptor-mediated uptake of immune complexes (b). Once the intact antigen or peptide enters the endocytic compartment they are exposed to various proteases, notably the cathepsin family, which are responsible for antigen degradation (c). Peptide vaccines therefore need to survive this environment as they are transported to a compartment known as MIIC (a MHC-II-rich endosomal compartment). Here peptides are loaded into MHC II molecules, a process that is facilitated by the chaperone human leukocyte antigen-DM (HLA-DM) that is responsible for removing the invariant (Ii) chain. Another molecule, HLA-DO, also modulates this process in B cells (d).
The mode of binding and repertoire of peptide ligands that are bound by MHC II differs from the binding of peptides to class I molecules. The interactions that close the peptide-binding cleft of class I molecules are not apparent in MHC II, which allows the termini of the bound class II peptide to project out of the ends of the cleft. Hence, MHC II peptides are typically longer than class I ligands, averaging around 13 amino-acids in length, but can be considerably longer. Similar to MHC I, polymorphic amino-acid residues line the pockets of the binding cleft. Both structural and biochemical studies indicate that amino-acid side chains at residues 1, 4, 6 and 9 of the class-II-bound peptide typically interact with these pockets, therby conferring allelic specificity21 and 'anchoring' the peptide into the cleft. It has also been suggested that the binding of ligands to MHC II is more promiscuous than the binding of peptides to MHC I, owing to their free termini and ability to use a range of anchor residues or induce a shift in the binding register. This observation makes it more difficult to define anchor residues and to predict which peptides will be able to bind to particular MHC II molecules. Amino- and carboxy-terminal exopeptidase activities can trim peptides that are bound to class II molecules during their transit to the cell surface, further hampering efforts to define MHC-II-binding motifs and to reliably predict MHC II ligands22.
Novel insights into the nature of T-cell epitopes
CTL epitopes of unusual length, and conformational dependence of their recognition. Despite antigen processing in the class I compartment predisposing towards peptides of 8–10 amino acids in length, peptides considerably longer than this bind to and are naturally presented by MHC I. These include naturally presented self-peptides of which at least 5% are over 10 amino acids in length23. The structures of several peptides that are considerably longer than 10 residues in complex with MHC I have been studied, and, in each case, the peptide adopts a bulging conformation while maintaining a conserved hydrogen-bonding network at the peptide amino termini and carboxy termini24,25,26,27,28. These bulged epitopes can be rigid and display a defined conformation or exhibit a considerable degree of flexibility when bound to the antigen-binding cleft. For example, we have recently studied a highly immunogenic region from the BZLF1 antigen of the Epstein–Barr virus (EBV) that is presented by the HLA-B35 family members in a length and conformation-specific manner15. Some of these unusually long epitopes contain within their sequences peptides of more conventional length that score well using predictive class-I-binding algorithms, but nevertheless are not reported to induce CTL responses14. Moreover, these shorter fragments are often naturally presented on MHC I but fail to be immunogenic24,29. Why, in circumstances such as EBV infection of HLA-B35 individuals, these longer immunogenic peptides are presented on MHC I and preferentially selected as targets of CTL is poorly understood. It is most likely the result of biases in antigen processing and T-cell repertoire towards the longer peptide15,16. The existence of such epitopes presents new challenges to vaccine design, both in terms of controlling the processing of these long peptides and ensuring the correct conformation is assumed by the epitope that is bound to MHC I.
T-cell recognition of post-translationally modified peptides. T-cell epitopes that have been characterized include glycopeptides; phosphopeptides; deamidated peptides, both through the action of N-glycanases and enzymes such as transglutaminase; peptides exhibiting asparagine-bond isomerism, acetylation, methylation, cysteinylation and nitration; and peptides containing disulphide bonds11,17,30,31,32,33,34,35,36,37,38,39,40,41. In addition to modifications that occur spontaneously during ageing, and exposure of proteins to hostile cellular and extracellular environments (for example, oxidation, deamidation), many of these post-translational modifications (PTMs) are performed within or outside the cell by specific enzymes in processes that have complex feedback mechanisms. Breakdown of these feedback mechanisms is frequently associated with pathological processes that result in the accumulation of aberrantly or excessively post-translationally modified material42,43,44. PTMs can be reliably and accurately incorporated into peptides at the time of their synthesis, thereby allowing the end product of complex antigen presentation to be mimicked by a simple compound and the desired immune response to be elicited. Recent reports have described perhaps the most extreme form of PTM, whereby epitopes are generated from discontinuous peptide sequences45,46 by a protein-splicing mechanism — a mechanism that remains to be fully elucidated. Such processing might occur in a tissue-specific manner and therefore such epitopes are not only impossible to predict but peptide-based vaccines might be the only reliable way of delivering such epitopes to the immune system. Nonetheless, if they are properly characterized they can be easily synthesized for incorporation into subunit vaccines.
Tissue-specific antigen presentation
The proteasome can exist in several different forms depending on the exposure of the cell to pro-inflammatory stimuli12. The different forms of the proteasome engender various proteolytic activities and consequently produce an array of peptide precursors for transport into the lumen of the endoplasmic reticulum where they assemble with MHC I. APCs predominantly express the immunoproteasome and potentially present different peptides compared with target tissues, be they infected epithelium or tumour cells that might express the constitutive proteasome without interferon-γ (IFNγ)-inducible subunits. More recently, the interplay of the various forms of the proteasome with other peptidases has been elucidated, adding to the complexity of the processing of antigens to generate the peptides bound to MHC class I molecules that are destined for export to the cell surface47,48,49. This presents a challenge when administering antigens exogenously. To elicit an immune response that mimics natural immunity, the correct, potentially tissue-specific processing events will need to take place to generate immune responses towards epitopes of clinical efficacy. Natural antigen processing also involves the editing of the peptide repertoire by the peptide-editing molecules HLA-DM and HLA-DO. Allelic variation in MHC II molecules can also vary in their dependence on peptide editing by HLA-DM and HLA-DO50. A role for tapasin, a putative peptide-editing chaperone involved in the assembly of MHC I with peptide, has also been reported51,52,53. Expression levels of tapasin vary between different tissues, with particularly high levels in activated dendritic cells54. Moreover, MHC I molecules also vary in their dependence on tapasin for peptide loading2,52,55,56,57,58,59,60,61. These features of antigen presentation further complicate the selection of epitopes and prediction of natural immunogenic peptides.
Engineering peptide-based vaccines
Several strategies have been adopted to enhance the effectiveness of peptide therapeutics, including glycosylation, amino-acid-sequence modification, pegylation and cyclization. Of these modalities only the replacement of amino acids within the sequence of a peptide epitope is directly relevant to vaccination studies. Simple epitope modifications have typically consisted of MHC-anchor substitutions in which suboptimal anchor residues are substituted to improve MHC binding and immunogenicity62. In addition, heteroclitic analogues with substitutions outside the MHC-anchor residues have been described that have the capacity to induce hyperstimulation of T cells63. These analogues are of interest in the development of vaccines as they can achieve more potent immune responses. This observation might be explained by the increased stability of the MHC/peptide complex, and the increased avidity and residence time of the TCR–peptide/MHC complex64. Heteroclitic antigens can also break T-cell tolerance65,66,67, which has the potential to assist in the development of antitumour immunity, which frequently involves self-antigens. Although these approaches can produce better vaccine components, they have until recently been constrained to making substitutions using only naturally occurring amino acids63. To improve class I binding and TCR avidity, and to introduce favourable biophysical properties to the epitope such as protease resistance and oral stability, it is often desirable to introduce non-natural amino-acid analogues into the peptide epitope.
Several studies have explored modifications that not only provide subtle conformational changes to the peptide/MHC structure, but also incorporate resistance against proteases. The incorporation of β-amino-acids into epitopes can increase the binding affinity of the mimetic for the MHC molecule relative to the wild-type peptide67,68,69,70. The side chains of β-amino-acids are identical to their parent α-amino-acid, which is of particular importance to maintaining the same properties as the natural epitope. The introduction of a methylene moiety (Table 2) into peptides that are solely composed of β-amino-acids results in complete resistance to proteolytic degradation71. Furthermore, it has been shown that even single amino-acid substitutions of the naturally occurring α-amino-acid with the homologous β-amino-acid residue can have dramatic effects on the overall stability of the entire peptide70. Other methods used to achieve protease resistance and to maintain T-cell crossreactivity, including peptide-backbone modifications, D-amino-acids or retroinversion of sequences (in which all amino-acids in a epitope are converted to D-amino-acids and the sequence reversed) are summarized in Table 2. Modification of the N and C termini of a peptide can also prevent its degradation by exopeptidases72. These modifications usually involve N-acetylation and C-amidation, respectively. The ability to stabilize short peptide epitopes and to control the proteolysis of longer precursor peptides by protecting scissile-peptide bonds or by directing antigen processing allows for the precise delivery of peptide-based therapeutics to the immune system.
Current developments
As discussed before, there is no peptide vaccine on the market yet. However, several promising preclinical and clinical trials for vaccines that involve peptide-based strategies are currently being carried out. For example, recent reports have shown that a multi-epitope approach has been successful for the treatment of hepatitis C viral infections73, and peptide trials for vaccination in numerous cancers have been reported extensively (see Ref. 74 for a review). However, perhaps the most encouraging development is the number of clinical trials supported by both small and large pharmaceutical companies that are based on the use of peptide-based vaccines (Table 1a,b). In addition, several new modalities in delivery of vaccines have been developed75,76,77 (Box 2), including the combination of peptide-based and more traditional vaccine approaches. The marriage of epitope engineering and chemical optimization with these new delivery mechanisms promises to provide the next generation of immunotherapeutics.
Future outlook
It is clear that vaccines of the future will require a systematic approach to tailor the desired immune response to individuals. Technology has evolved rapidly to allow for the identification of patient-specific epitopes based on their HLA haplotypes, and these forms of molecular medicines are becoming a reality. Armed with new technologies, immunologists can examine the molecular ingredients of a successful immune response, which have revealed a tremendous amount of biochemical diversity in clinically important epitopes. The use of peptides offers a flexible and simple way to deal with much of this complexity by bypassing the requirements for antigen processing and delivery of a precise and chemically defined payload to the APC. Moreover, peptides display more drug-like properties than recombinant proteins or whole pathogen vaccines, which will open up new avenues for vaccine delivery, and therefore attract increasing interest from the pharmaceutical industry.
References
Singh-Jasuja, H., Emmerich, N. P. & Rammensee, H. G. The Tubingen approach: identification, selection, and validation of tumor-associated HLA peptides for cancer therapy. Cancer Immunol. Immunother. 53, 187–195 (2004).
Macdonald, W. A. et al. A naturally selected dimorphism within the HLA-B44 supertype alters class I structure, peptide repertoire and T cell recognition. J. Exp. Med. 198, 679–691 (2003).
Zhang, G. L., Bozic, I., Kwoh, C. K., August, J. T. & Brusic, V. Prediction of supertype-specific HLA class I binding peptides using support vector machines. J. Immunol. Methods 320, 143–154 (2007).
Peters, B. et al. A community resource benchmarking predictions of peptide binding to MHC-I molecules. PLoS Comput. Biol. 2, e65 (2006).
Purcell, A. W. et al. Dissecting the role of peptides in the immune response: theory, practice and the application to vaccine design. J. Pept. Sci. 9, 255–281 (2003).
Moutaftsi, M. et al. A consensus epitope prediction approach identifies the breadth of murine T (CD8+)-cell responses to vaccinia virus. Nature Biotech. 24, 817–819 (2006).
Andersen, M. H. et al. Poor correspondence between predicted and experimental binding of peptides to class I MHC molecules. Tissue Antigens 55, 519–531 (2000).
Rammensee, H., Bachmann, J., Emmerich, N. P., Bachor, O. A. & Stevanovic, S. SYFPEITHI: database for MHC ligands and peptide motifs. Immunogenetics 50, 213–219 (1999).
Schafer, J. R., Jesdale, B. M., George, J. A., Kouttab, N. M. & De Groot, A. S. Prediction of well-conserved HIV-1 ligands using a matrix-based algorithm, EpiMatrix. Vaccine 16, 1880–1884 (1998).
Brusic, V., Rudy, G., Honeyman, G., Hammer, J. & Harrison, L. Prediction of MHC class II-binding peptides using an evolutionary algorithm and artificial neural network. Bioinformatics 14, 121–130 (1998).
Engelhard, V. H., Altrich-Vanlith, M., Ostankovitch, M. & Zarling, A. L. Post-translational modifications of naturally processed MHC-binding epitopes. Curr. Opin. Immunol. 18, 92–97 (2006).
Kuckelkorn, U. et al. Link between organ-specific antigen processing by 20S proteasomes and CD8(+) T cell-mediated autoimmunity. J. Exp. Med. 195, 983–990 (2002). This paper establishes that different arrays of antigenic peptides are produced by different tissues, highlighting the complexities of antigen processing and the challenges to vaccine design.
Del-Val, M. & Lopez, D. Multiple proteases process viral antigens for presentation by MHC class I molecules to CD8(+) T lymphocytes. Mol. Immunol. 39, 235–247 (2002).
Burrows, S. R., Rossjohn, J. & McCluskey, J. Have we cut ourselves too short in mapping CTL epitopes? Trends Immunol. 27, 11–16 (2005).
Tynan, F. E. et al. T cell receptor recognition of a 'super-bulged' major histocompatibility complex class I-bound peptide. Nature Immunol. 6, 1114–1122 (2005).
Tynan, F. E. et al. A T cell receptor flattens a bulged antigenic peptide presented by a major histocompatibility complex class I molecule. Nature Immunol. 8, 268–276 (2007). References 15 and 16 demonstrate alternative strategies that T-cell receptors adopt to recognize bulged T-cell epitopes while maintaining MHC-restriction.
Mannering, S. I. et al. The insulin A-chain epitope recognized by human T cells is posttranslationally modified. J. Exp. Med. 202, 1191–1197 (2005).
Yewdell, J. W. & Bennink, J. R. Immunodominance in major histocompatibility complex class I-restricted T lymphocyte responses. Annu. Rev. Immunol. 17, 51–88 (1999).
Chang, L. et al. Novel strategy for identification of candidate cytotoxic T-cell epitopes from human preproinsulin. Tissue Antigens 62, 408–417 (2003).
Buus, S. Description and prediction of peptide-MHC binding: the 'human MHC project'. Curr. Opin. Immunol. 11, 209–213 (1999).
Rammensee, H. G. Chemistry of peptides associated with MHC class I and class II molecules. Curr. Opin. Immunol. 7, 85–96 (1995).
Watts, C. Capture and processing of exogenous antigens for presentation on MHC molecules. Annu. Rev. Immunol. 15, 821–850 (1997).
Hickman, H. D. et al. Toward a definition of self: proteomic evaluation of the class I peptide repertoire. J. Immunol. 172, 2944–2952 (2004).
Tynan, F. E. et al. High resolution structures of highly bulged viral epitopes bound to major histocompatibility complex class I. Implications for T-cell receptor engagement and T-cell immunodominance. J. Biol. Chem. 280, 23900–23909 (2005).
Guo, H. -C. et al. Diferent length peptides bind to HLA-Aw68 similarly at their ends but bulge out in the middle. Nature 360, 364–366 (1992).
Speir, J. A., Stevens, J., Joly, E., Butcher, G. W. & Wilson, I. A. Two different, highly exposed, bulged structures for an unusually long peptide bound to rat MHC class I RT1-Aa. Immunity 14, 81–92 (2001).
Probst-Kepper, M. et al. Conformational restraints and flexibility of 14-meric peptides in complex with HLA-B*3501. J. Immunol. 173, 5610–5616 (2004).
Miles, J. J. et al. CTL Recognition of a bulged viral peptide involves biased TCR selection. J. Immunol. 175, 3826–3834 (2005).
Tynan, F. E. et al. The immunogenicity of a viral cytotoxic T cell epitope is controlled by its MHC-bound conformation. J. Exp. Med. 202, 1249–1260 (2005).
Ireland, J., Herzog, J. & Unanue, E. R. Cutting Edge: Unique T cells that recognize citrullinated peptides are a feature of protein immunization. J. Immunol. 177, 1421–1425 (2006).
Van den Steen, P. E. et al. Generation of glycosylated remnant epitopes from human collagen type II by gelatinase B. Biochemistry 43, 10809–10816 (2004).
Backlund, J. et al. Predominant selection of T cells specific for the glycosylated collagen type II epitope (263–270) in humanized transgenic mice and in rheumatoid arthritis. Proc. Natl Acad. Sci USA 99, 9960–9965 (2002).
Anderson, R. P., Degano, P., Godkin, A. J., Jewell, D. P. & Hill, A. V. In vivo antigen challenge in celiac disease identifies a single transglutaminase-modified peptide as the dominant A-gliadin T-cell epitope. Nature Med. 6, 337–342 (2000).
Cao, L., Goodin, R., Wood, D., Moscarello, M. A. & Whitaker, J. N. Rapid release and unusual stability of immunodominant peptide 45–89 from citrullinated myelin basic protein. Biochemistry 38, 6157–6163 (1999).
Speir, J. A., Abdel-Motal, U. M., Jondal, M. & Wilson, I. A. Crystal structure of an MHC class I presented glycopeptide that generates carbohydrate-specific CTL. Immunity 10, 51–61 (1999).
Haurum, J. S. et al. Recognition of carbohydrate by major histocompatibility complex class I-restricted, glycopeptide-specific cytotoxic T lymphocytes. J. Exp. Med. 180, 739–744 (1994).
Meadows, L. et al. The HLA-A*0201-restricted H-Y antigen contains a posttranslationally modified cysteine that significantly affects T cell recognition. Immunity 6, 273–281 (1997).
Skipper, J. C. et al. An HLA-A2-restricted tyrosinase antigen on melanoma cells results from posttranslational modification and suggests a novel pathway for processing of membrane proteins. J. Exp. Med. 183, 527–534 (1996). This paper gives one of the first demonstrations that T cells can recognize chemically modified peptides.
McAdam, S. N. et al. T cell recognition of the dominant I-A(k)-restricted hen egg lysozyme epitope: critical role for asparagine deamidation. J. Exp. Med. 193, 1239–1246 (2001).
van Stipdonk, M. J. et al. T cells discriminate between differentially phosphorylated forms of αB-crystallin, a major central nervous system myelin antigen. Int. Immunol. 10, 943–950 (1998).
Chen, W., Ede, N. J., Jackson, D. C., McCluskey, J. & Purcell, A. W. CTL recognition of an altered peptide associated with asparagine bond rearrangement. Implications for immunity and vaccine design. J. Immunol. 157, 1000–1005 (1996).
Anderton, S. M. Post-translational modifications of self antigens: implications for autoimmunity. Curr. Opin. Immunol. 16, 753–758 (2004).
Williamson, N. A., Rossjohn, J. & Purcell, A. W. Tumors reveal their secrets to cytotoxic T cells. Proc. Natl Acad. Sci. USA 103, 14649–14650 (2006).
Zarling, A. L. et al. Identification of class I MHC-associated phosphopeptides as targets for cancer immunotherapy. Proc. Natl Acad. Sci. USA 103, 14889–14894 (2006). The first demonstration that peptides derived from aberrant phosphorylation in tumour cells can be targeted by antitumor CTL.
Hanada, K. -I., Yewdell, J. W. & Yang, J. C. Immune recognition of a human renal cancer antigen through post-translational protein splicing. Nature 427, 252–256 (2004).
Vigneron, N. et al. An antigenic peptide produced by peptide splicing in the proteasome. Science 304, 587–590 (2004). References 45 and 46 identified T-cell epitopes resulting from protein splicing to produce novel non-genetically encoded peptides.
Kloetzel, P. M. & Ossendorp, F. Proteasome and peptidase function in MHC-class-I-mediated antigen presentation. Curr. Opin. Immunol. 16, 76–81 (2004).
Rock, K. L., York, I. A. & Goldberg, A. L. Post-proteasomal antigen processing for major histocompatibility complex class I presentation. Nature Immunol. 5, 670–677 (2004).
Kloetzel, P. M. Generation of major histocompatibility complex class I antigens: functional interplay between proteasomes and TPPII. Nature Immunol. 5, 661–669 (2004).
Brooks, A. G., Campbell, P. L., Reynolds, P., Gautam, A. M. & McCluskey, J. Antigen presentation and assembly by mouse I-Ak class II molecules in human APC containingdeleted or mutated HLA DM genes. J. Immunol. 153, 5382–5392 (1994).
Purcell, A. W. The peptide-loading complex and ligand selection during the assembly of HLA class I molecules. Mol. Immunol. 37, 483–492 (2000).
Purcell, A. W. et al. Quantitative and qualitative influences of tapasin on the class I peptide repertoire. J. Immunol. 166, 1016–1027 (2001).
Sesma, L. et al. Qualitative and quantitative differences in peptides bound to HLA-B27 in the presence of mouse versus human tapasin define a role for tapasin as a size-dependent peptide editor. J. Immunol. 174, 7833–7844 (2005).
Ackerman, A. L., Kyritsis, C., Tampe, R. & Cresswell, P. Early phagosomes in dendritic cells form a cellular compartment sufficient for cross presentation of exogenous antigens. Proc. Natl Acad. Sci. USA 100, 12889–12894 (2003).
Peh, C. A. et al. HLA-B27-restricted antigen presentation in the absence of tapasin reveals polymorphism in mechanisms of HLA class I peptide loading. Immunity 8, 531–542 (1998).
Purcell, A. W., Kelly, A. J., Peh, C. A., Dudek, N. L. & McCluskey, J. Endogenous and exogenous factors contributing to the surface expression of HLA B27 on mutant APC. Hum. Immunol. 61, 120–130 (2000).
Williams, A. P., Peh, C. A., Purcell, A. W., McCluskey, J. & Elliott, T. Optimization of the MHC class I peptide cargo is dependent on tapasin. Immunity 16, 509–520 (2002).
Zernich, D. et al. Natural HLA class I polymorphism controls the pathway of antigen presentation and susceptibility to viral evasion. J. Exp. Med. 200, 13–24 (2004).
Park, B., Lee, S., Kim, E. & Ahn, K. A single polymorphic residue within the peptide-binding cleft of MHC class I molecules determines spectrum of tapasin dependence. J. Immunol. 170, 961–968 (2003).
Myers, N. B. et al. K(b), k(d), and L(d) molecules share common tapasin dependencies as determined using a novel epitope tag. J. Immunol. 165, 5656–5663 (2000).
Braud, V. M., Allan, D. S., Wilson, D. & McMichael, A. J. TAP- and tapasin-dependent HLA-E surface expression correlates with the binding of an MHC class I leader peptide. Curr. Biol. 8, 1–10 (1998).
Sette, A. et al. The relationship between class I binding affinity and immunogenicity of potential cytotoxic T cell epitopes. J. Immunol. 153, 5586–5592 (1994). An important study that highlights the relationship between MHC affinity and immunogenicity of peptides.
Sette, A. & Fikes, J. Epitope-based vaccines: an update on epitope identification, vaccine design and delivery. Curr. Opin. Immunol. 15, 461–470 (2003).
Slansky, J. E. et al. Enhanced antigen-specific antitumor immunity with altered peptide ligands that stabilize the MHC–peptide–TCR complex. Immunity 13, 529–538 (2000).
Dyall, R. et al. Heteroclitic immunization induces tumor immunity. J. Exp. Med. 188, 1553–1561 (1998).
Du, A. P. et al. Structural and immunological characterisation of heteroclitic peptide analogues corresponding to the 600–612 region of the HIV envelope gp41 glycoprotein. J. Mol. Biol. 323, 503–521 (2002).
Tangri, S. et al. Structural features of peptide analogs of human histocompatibility leukocyte antigen class I epitopes that are more potent and immunogenic than wild-type peptide. J. Exp. Med. 194, 833–846 (2001).
Guichard, G. et al. Melanoma peptide MART-1 (27–35) analogues with enhanced binding capacity to the human class I histocompatibility molecule HLA-A2 by introduction of a β-amino acid residue: implications for recognition by tumor-infiltrating lymphocytes. J. Med. Chem. 43, 3803–3808 (2000).
Reinelt, S. et al. β-amino acid scan of a class I major histocompatibility complex-restricted alloreactive T-cell epitope. J. Biol. Chem. 276, 24525–24530 (2001).
Webb, A. I. et al. T Cell determinants incorporating β-amino acid residues are protease resistant and remain immunogenic in vivo. J. Immunol. 175, 3810–3818 (2005). References 68 and 70 highlight the use of protease-resistant β-amino-acids to stabilize T-cell epitopes while maintaining immunogenicity.
Steer, D. L., Lew, R. A., Perlmutter, P., Smith, A. I. & Aguilar, M. I. β-amino acids: versatile peptidomimetics. Curr. Med. Chem. 9, 811–822 (2002).
Marschutz, M. K. et al. Improvement of the enzymatic stability of a cytotoxic T-lymphocyte-epitope model peptide for its oral administration. Peptides 23, 1727–1733 (2002).
Firbas, C. et al. Immunogenicity and safety of a novel therapeutic hepatitis C virus (HCV) peptide vaccine: a randomized, placebo controlled trial for dose optimization in 128 healthy subjects. Vaccine 24, 4343–4353 (2006).
Pietersz, G. A., Pouniotis, D. S. & Apostolopoulos, V. Design of peptide-based vaccines for cancer. Curr. Med. Chem. 13, 1591–1607 (2006).
Gentilucci, L., Tolomelli, A. & Squassabia, F. Peptides and peptidomimetics in medicine, surgery and biotechnology. Curr. Med. Chem. 13, 2449–2466 (2006).
Palena, C., Abrams, S. I., Schlom, J. & Hodge, J. W. Cancer vaccines: preclinical studies and novel strategies. Adv. Cancer Res. 95, 115–145 (2006).
Toth, I. A novel chemical approach to drug delivery: lipid amino acid conjugates. J. Drug Target. 2, 217–239 (1994).
Moss, D. J. et al. Strategies involved in developing an effective vaccine for EBV- associated diseases. Adv. Cancer Res. 69, 213–245 (1996).
Kotb, M., Courtney, H. S., Dale, J. B. & Beachey, E. H. Cellular and biochemical responses of human T lymphocytes stimulated with streptococcal M proteins. J. Immunol. 142, 966–970 (1989).
Pruksakorn, S. et al. Identification of T cell autoepitopes that cross-react with the C- terminal segment of the M protein of group A Streptococci. Int. Immunol. 6, 1235–1244 (1994).
Suto, R. & Srivastava, P. K. A mechanism for the specific immunogenicity of heat shock protein-chaperoned peptides. Science 269, 1585–1588 (1995).
Blachere, N. E. et al. Heat shock protein-peptide complexes, reconstituted in vitro, elicit peptide-specific cytotoxic T lymphocyte response and tumor immunity. J. Exp. Med. 186, 1315–1322 (1997).
Tamura, Y., Peng, P., Liu, K., Daou, M. & Srivastava, P. K. Immunotherapy of tumors with autologous tumor-derived heat shock protein preparations. Science 278, 117–120 (1997).
Basu, S. & Srivastava, P. K. Calreticulin, a peptide-binding chaperone of the endoplasmic reticulum, elicits tumor- and peptide-specific immunity. J. Exp. Med. 189, 797–802 (1999).
Castellino, F. et al. Receptor-mediated uptake of antigen/heat shock protein complexes results in major histocompatibility complex class I antigen presentation via two distinct processing pathways. J. Exp. Med. 191, 1957–1964 (2000).
Binder, R. J., Karimeddini, D. & Srivastava, P. K. Adjuvanticity of α 2-macroglobulin, an independent ligand for the heat shock protein receptor CD91. J. Immunol. 166, 4968–4972 (2001).
Linderoth, N. A., Simon, M. N., Hainfeld, J. F. & Sastry, S. Binding of antigenic peptide to the endoplasmic reticulum-resident protein gp96/GRP94 heat shock chaperone occurs in higher order complexes. Essential role of some aromatic amino acid residues in the peptide-binding site. J. Biol. Chem. 276, 11049–11054 (2001).
Noessner, E. et al. Tumor-derived heat shock protein 70 peptide complexes are cross-presented by human dendritic cells. J. Immunol. 169, 5424–5432 (2002).
Aguilar, J. C. & Rodriguez, E. G. Vaccine adjuvants revisited. Vaccine 16 Feb 2007 (doi:10.1016/j.vaccine.2007.01.111).
Brown, L. E. & Jackson, D. C. Lipid-based self-adjuvanting vaccines. Curr. Drug Deliv. 2, 383–393 (2005).
Dranoff, G. GM-CSF-based cancer vaccines. Immunol. Rev. 188, 147–154 (2002).
Markovic, S. N. et al. Peptide vaccination of patients with metastatic melanoma: improved clinical outcome in patients demonstrating effective immunization. Am. J. Clin. Oncol. 29, 352–360 (2006).
Lee, P. et al. Effects of interleukin-12 on the immune response to a multipeptide vaccine for resected metastatic melanoma. J. Clin. Oncol. 19, 3836–3847 (2001).
Dakappagari, N. K. et al. A chimeric multi-human epidermal growth factor receptor-2b cell epitope peptide vaccine mediates superior antitumor responses. J. Immunol. 170, 4242–4253 (2003).
Chianese-Bullock, K. A. et al. MAGE-A1-, MAGE-A10-, and gp100-derived peptides are immunogenic when combined with granulocyte-macrophage colony-stimulating factor and montanide ISA-51 adjuvant and administered as part of a multipeptide vaccine for melanoma. J. Immunol. 174, 3080–3086 (2005).
Liang, M. T., Davies, N. M., Blanchfield, J. T. & Toth, I. Particulate systems as adjuvants and carriers for peptide and protein antigens. Curr. Drug Deliv. 3, 379–388 (2006).
Sanders, M. T., Brown, L. E., Deliyannis, G. & Pearse, M. J. ISCOM-based vaccines: the second decade. Immunol. Cell Biol. 83, 119–128 (2005).
Skene, C. D. & Sutton, P. Saponin-adjuvanted particulate vaccines for clinical use. Methods 40, 53–59 (2006).
Kersten, G. F. & Crommelin, D. J. Liposomes and ISCOMs. Vaccine 21, 915–920 (2003).
Taieb, J., Chaput, N. & Zitvogel, L. Dendritic cell-derived exosomes as cell-free peptide-based vaccines. Crit. Rev. Immunol. 25, 215–223 (2005).
Westerfeld, N. & Zurbriggen, R. Peptides delivered by immunostimulating reconstituted influenza virosomes. J. Pept. Sci. 11, 707–712 (2005).
Petrovsky, N. Novel human polysaccharide adjuvants with dual Th1 and Th2 potentiating activity. Vaccine 24 (Suppl. 2), 26–29 (2006).
Luft, T. et al. Exogenous peptides presented by transporter associated with antigen processing (TAP)-deficient and TAP-competent cells: intracellular loading and kinetics of presentation. J. Immunol. 167, 2529–2537 (2001). This paper highlights the different paths exogenous peptides take during vaccination compared with endogenous peptides traversing the MHC class I processing pathway.
Carbone, F. R., Kurts, C., Bennett, S. R., Miller, J. F. & Heath, W. R. Cross-presentation: a general mechanism for CTL immunity and tolerance. Immunol. Today 19, 368–373 (1998).
West, M. A. et al. Membrane ruffling, macropinocytosis and antigen presentation in the absence of gelsolin in murine dendritic cells. Eur. J. Immunol. 29, 3450–3455 (1999).
Sallusto, F., Cella, M., Danieli, C. & Lanzavecchia, A. Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: downregulation by cytokines and bacterial products. J. Exp. Med. 182, 389–400 (1995).
Rock, K. L. & Shen, L. Cross-presentation: underlying mechanisms and role in immune surveillance. Immunol. Rev. 207, 166–183 (2005).
Li, Z., Menoret, A. & Srivastava, P. Roles of heat-shock proteins in antigen presentation and cross-presentation. Curr. Opin. Immunol. 14, 45–51 (2002).
Singh-Jasuja, H. et al. Cross-presentation of glycoprotein 96-associated antigens on major histocompatibility complex class I molecules requires receptor-mediated endocytosis. J. Exp. Med. 191, 1965–1974 (1999).
Williamson, N. A. & Purcell, A. W. Use of proteomics to define targets of T-cell immunity. Expert Rev. Proteomics 2, 367–380 (2005).
Yewdell, J. W., Anton, L. C. & Bennink, J. R. Defective ribosomal products (DRiPs). A major source of antigenic peptides for MHC class I molecules? J. Immunol. 157, 1823–1826 (1996).
Schubert, U. et al. Rapid degradation of a large fraction of newly synthesized proteins by proteasomes. Nature 404, 770–774 (2000). This paper demonstrates that the majority of endogenous peptides presented by MHC class I molecules are derived from premature translation products.
Falk, K. et al. Ligand exchange of major histocompatibility complex class II proteins is triggered by H-bond donor groups of small molecules. J. Biol. Chem. 277, 2709–2715 (2002).
Jensen, P. E., Weber, D. A., Thayer, W. P., Westerman, L. E. & Dao, C. T. Peptide exchange in MHC molecules. Immunol. Rev. 172, 229–238 (1999).
Reid, P. A. & Watts, C. Cycling of cell-surface MHC glycoproteins through primaquine-sensitive intracellular compartments. Nature 346, 655–657 (1990).
Webb, A. I., Aguilar, M. I. & Purcell, A. W. Optimisation of peptide-based cytotoxic T-cell determinants using non-natural amino acids. Lett. Pept. Sci. 10, 561–569 (2003).
Acknowledgements
A.W.P. is the Grimwade Senior Research Fellow in the Department of Biochemistry and Molecular Biology, University of Melbourne. J.R. is an Australian Research Council Federation Fellow. The financial support of the Australian Research Council, National Health and Medical Research Council of Australia and National Institutes of Health is gratefully acknowledged. We acknowledge I. Smith for providing the material regarding peptide-based vaccine development in industry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary information S1 (table)
Human leukocyte antigen supertypes and their peptide-binding specificities‡ (PDF 137 kb)
Supplementary information S2 (figure)
Different length epitopes bound within the antigen-binding cleft of MHC I. (PDF 363 kb)
Related links
Glossary
- Major histocompatibility complex
-
(MHC). A cluster of genes on human chromosome 6 or on mouse chromosome 17 that encode for MHC molecules. These molecules are the most polymorphic in the genome, and are the ones recognized by T lymphocytes during transplant rejection. They encode for a family of cellular antigens that help the immune system to recognize self from non-self.
- Dendritic cells
-
Antigen-presenting cells found in T-cell areas of lymphoid tissues, but also as minor cellular components in most tissues. They have a branched or dendritic morphology and are the most potent stimulators of T-cell responses.
- Macrophages
-
One of the main types of professional phagocytes. Macrophages are long-lived and detrimental for many microbial pathogens. Intracellular bacteria, including Mycobacterium tuberculosis, can survive within the macrophages.
- Human leukocyte antigen
-
(HLA). Genetic designation for the human major histocompatibility complex.
- Immunoproteasome
-
The proteasome is a multisubunit structure found in the cytoplasm, and is responsible for protein degradation. During inflammation some of the constitutive catalytic subunits are replaced by interferon-γ-inducible subunits. This inflammation-induced proteasome is known as the immunoproteasome.
- HLA-DM and HLA-DO
-
These are chaperones encoded by the human major histocompatibility complex, and are responsible for facilitating the peptide loading of human leukocyte antigen (HLA) class II molecules in human antigen-presenting cells such as dendritic cells and B cells.
- Pegylation
-
This is the process of attaching one or more chains of polyethylene glycol (also known as PEG) to a peptide molecule, resulting in increased bioavailability and stability.
Rights and permissions
About this article
Cite this article
Purcell, A., McCluskey, J. & Rossjohn, J. More than one reason to rethink the use of peptides in vaccine design. Nat Rev Drug Discov 6, 404–414 (2007). https://doi.org/10.1038/nrd2224
Issue Date:
DOI: https://doi.org/10.1038/nrd2224
This article is cited by
-
Enhancing explainable SARS-CoV-2 vaccine development leveraging bee colony optimised Bi-LSTM, Bi-GRU models and bioinformatic analysis
Scientific Reports (2024)
-
Evaluation of immunogenicity and protective efficacy of bacteriophage conjugated haemagglutinin based subunit vaccine against equine influenza virus in a murine model
Veterinary Research Communications (2024)
-
Quantum dots-based “chemical tongue” for the discrimination of short-length Aβ peptides
Microchimica Acta (2024)
-
Radiotherapy combined with nano-biomaterials for cancer radio-immunotherapy
Journal of Nanobiotechnology (2023)
-
In silico Approach for B Cell Epitopes Prediction of Respiratory Syncytial Virus
International Journal of Peptide Research and Therapeutics (2023)