Key Points
-
Obesity continues to be a major public health problem worldwide
-
Bariatric surgery is an effective treatment for severe obesity that results in the improvement or remission of many obesity-related comorbid conditions, as well as sustained weight loss and improvement in quality of life
-
The four most common bariatric operations performed worldwide are laparoscopic sleeve gastrectomy, laparoscopic Roux-en-Y gastric bypass, laparoscopic adjustable gastric banding and duodenal switch
-
Bariatric surgery is now safe, with mortality comparable to common elective general surgical operations
-
Level 1 evidence show that bariatric surgery provides superior short-term and long-term weight loss and improvement of type 2 diabetes mellitus compared with conventional medical therapy
-
Newly approved laparoscopic and endoscopic devices are now available for management of patients with obesity; however, the long-term efficacy of these devices is unknown
Abstract
Obesity is one of the most important public health conditions worldwide. Bariatric surgery for severe obesity is an effective treatment that results in the improvement and remission of many obesity-related comorbidities, as well as providing sustained weight loss and improvement in quality of life. Contemporary bariatric operations include Roux-en-Y gastric bypass, sleeve gastrectomy, adjustable gastric band and the duodenal switch. The vast majority of these procedures are now performed using laparoscopic technique, the main advantages of which include rapid recovery, the reduction of postoperative pain and the reduction of wound-related complications, compared with open surgery. Contemporary bariatric surgery is now safe, with a mortality of three in 1,000 patients; however, all bariatric operations are associated with their own unique short-term and long-term nutritional and procedural-related complications. Type 2 diabetes mellitus (T2DM) is the most studied metabolic disorder associated with obesity, with data demonstrating that improvement and remission of T2DM in patients with obesity is superior after bariatric surgery compared with conventional medical therapy. Bariatric surgery is now a part of some treatment algorithms for the medical management of patients with T2DM and severe obesity. New, minimally invasive and endoscopic devices for the treatment of obesity have now been approved in the USA, which will expand the treatment options for individuals with obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization. Obesity and overweight fact sheet. WHO http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed 28 December 2015).
Mingrone, G. et al. Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 386, 964–973 (2015).
Adams, T. D. et al. Long-term mortality after gastric bypass surgery. N. Engl. J. Med. 357, 753–761 (2007).
Esteban Varela, J. & Nguyen, N. T. Laparoscopic sleeve gastrectomy leads the U. S. utilization of bariatric surgery at academic medical centers. Surg. Obes. Relat. Dis. 11, 987–990 (2015).
Nguyen, N. T. et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann. Surg. 234, 279–289 (2001).
Blondet, J. J., Morton, J. M. & Nguyen, N. T. Hospital accreditation and bariatric surgery: is it important? Adv. Surg. 49, 123–129 (2015).
Chousleb, E., Rodriguez, J. A. & O'Leary, J. P. in The ASMBS Textbook of Bariatric Surgery (eds Nguyen, N. T., Blackstone, R. P., Morton, J. M., Ponce, J. & Rosenthal, R. J.) 37–46 (Springer, 2015).
Ponce, J., Nguyen, N. T., Hutter, M., Sudan, R. & Morton, J. M. American Society for Metabolic and Bariatric Surgery estimation of bariatric surgery procedures in the United States, 2011–2014. Surg. Obes. Relat. Dis. 11, 1199–2000 (2015).
Puzziferri, N., Austrheim-Smith, I. T., Wolfe, B. M., Wilson, S. E. & Nguyen, N. T. Three-year follow-up of a prospective randomized trial comparing laparoscopic versus open gastric bypass. Ann. Surg. 243, 181–188 (2006).
Dixon, J. B., Zimmet, P., Alberti, K. G., Rubino, F & International Diabetes Federation Taskforce on Epidemiology and Prevention. Bariatric surgery: an IDF statement for obese type 2 diabetes. Arq. Bras. Endocrinol. Metabol. 55, 367–382 (2011).
Jensen, M. D. et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. Circulation 129 (Suppl. 2), S102–S138 (2014).
Handelsman, Y. et al. American Association of Clinical Endocrinologists and American College of Endocrinology — clinical practice guidelines for developing a diabetes mellitus comprehensive care plan — 2015. Endocr. Pract. 21 (Suppl. 1), 1–87 (2015).
American Diabetes Association. Standards of medical care in diabetes — 2015: summary of revisions. Diabetes Care 38 (Suppl. 1), S4 (2015).
Ogden, C. L., Carroll, M. D., Kit, B. K. & Flegal, K. M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311, 806–814 (2014).
Finklestein, E. A., Trogdon, J. G., Cohen, J. W. & Dietz, W. Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Aff. (Millwood) 28, w822–w831 (2009).
Hammond, R. A. & Levine, R. The economic impact of obesity in the United States. Diabetes Metab. Syndr. Obes. 3, 285–295 (2010).
Angrisani, L. et al. Bariatric surgery worldwide 2013. Obes. Surg. 25, 1822–1832 (2015).
Mason, E. E. & Ito, C. Gastric bypass in obesity. Surg. Clin. North Am. 47, 1345–1351 (1967).
Hocking, M. P., Duerson, M. C., O'Leary, J. P. & Woodward, E. R. Jejunoileal bypass for morbid obesity — late follow-up in 100 cases. N. Engl. J. Med. 308, 995–999 (1983).
Maclean, L. D., Rhode, B. M. & Forse, R. A. Late results of vertical banded gastroplasty for morbid and super obesity. Surgery 107, 20–27 (1990).
Scopinaro, N. et al. Surgical revision of biliopancreatic diversion. Gastroenterol. Clin. North Am. 16, 529–531 (1987).
Hess, D. S. & Hess, D. W. Biliopancreatic diversion with a duodenal switch. Obes. Surg. 8, 267–282 (1998).
Marceau, P. et al. Biliopancreatic diversion with duodenal switch. World J. Surg. 22, 947–954 (1998).
Regan, J. P., Inabnet, W. B., Gagner, M. & Pomp, A. Early experience with two-stage laparoscopic Roux-en-Y gastric bypass as an alternative in the super-super obese patient. Obes. Surg. 13, 861–864 (2003).
ASMBS Clinical Issues Committee. Updated position statement on sleeve gastrectomy as a bariatric procedure. Surg. Obes. Relat. Dis. 8, e21–e26 (2012).
Wittgrove, A. C., Clark, G. W. & Tremblay, L. G. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes. Surg. 4, 353–357 (1994).
Nguyen, N. T., Ho, H. S., Palmer, L. S. & Wolfe, B. M. A comparison study of laparoscopic versus open gastric bypass for morbid obesity. J. Am. Coll. Surg. 191, 149–155 (2000).
Nguyen, N. T., Hinojosa, M., Fayad, C., Varela, E. & Wilson, S. E. Use and outcomes of laparoscopic versus open gastric bypass at academic medical centers. J. Am. Coll. Surg. 205, 248–255 (2007).
Nguyen, N. T., Vu, S., Kim, E., Bodunova, N. & Phelan, M. J. Trends in utilization of bariatric surgery, 2009–2012. Surg. Endosc. 30, 2723–2727 (2016).
NIH Conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann. Intern. Med. 115, 956–961 (1991).
Rubino, F. et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann. Surg. 244, 741–749 (2006).
Kashyap, S. R., Bhatt, D. L., Schauer, P. R. & STAMPEDE Investigators. Bariatric surgery versus advanced practice medical management in the treatment of type 2 diabetes mellitus: rationale and design of the Surgical Therapy And Medications Potentially Eradicate Diabetes Efficiently trial (STAMPEDE). Diabetes Obes. Metab. 12, 452–454 (2010).
Dixon, J. B. et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 299, 316–323 (2008).
ASMBS Clinical Issues Committee. Bariatric surgery in class I obesity (body mass index 30–35 kg/m2). Surg. Obes. Relat. Dis. 9, e1–e10 (2013).
O'Brien, P. E. et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann. Intern. Med. 144, 625–633 (2006).
Kumar, R. et al. Fat malabsorption and increased intestinal oxalate absorption are common after Roux-en-Y gastric bypass surgery. Surgery 149, 654–661 (2011).
Cohen, R. V., Rubino, F., Schiavon, C. & Cummings, D. E. Diabetes remission without weight loss after duodenal bypass surgery. Surg. Obes. Relat. Dis. 8, e66–e68 (2012).
Buchwald, H. et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 292, 1724–1737 (2004).
Wang, Y. & Liu, J. Plasma ghrelin modulation in gastric band operation and sleeve gastrectomy. Obes. Surg. 19, 357–362 (2009).
Bradley, D. et al. Matched weight loss induced by sleeve gastrectomy or gastric bypass similarly improves metabolic function in obese subjects. Obesity (Silver Spring) 22, 2026–2031 (2014).
Chang, S. H. et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 149, 275–287 (2014).
Hutter, M. M. et al. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann. Surg. 254, 410–420 (2011).
Himpens, J. et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch. Surg. 146, 802–807 (2011).
Kindel, T., Martin, E., Hungness, E. & Nagle, A. High failure rate of the laparoscopic-adjustable gastric band as a primary bariatric procedure. Surg. Obes. Relat. Dis. 10, 1070–1075 (2014).
Altieri, M. S. et al. Lap band outcomes from 19,221 patients across centers and over a decade within the state of New York. Surg. Endosc. 30, 1725–1732 (2016).
Mingrone, G. et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N. Engl. J. Med. 366, 1577–1585 (2012).
Morton, J. M., Garg, T. & Nguyen, N. Does hospital accreditation impact bariatric surgery safety? Ann. Surg. 260, 504–508 (2014).
Villamere, J., Gebhart, A., Vu, S. & Nguyen, N. T. Utilization and outcome of laparoscopic versus robotic general and bariatric surgical procedures at Academic Medical Centers. Surg. Endosc. 29, 1729–1736 (2015).
Longitudinal Assessment of Bariatric Surgery (LABS) Consortium et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N. Engl. J. Med. 361, 445–454 (2009).
Buchwald, H., Estok, R., Fahrbach, K., Banel, D. & Sledge, I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery 142, 621–632 (2007).
Inge, T. H. et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N. Engl. J. Med. 374, 113–123 (2016).
Inge, T. H. et al. Perioperative outcomes of adolescents undergoing bariatric surgery: the Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study. JAMA Pediatr. 168, 47–53 (2014).
Gebhart, A., Young, M. T. & Nguyen, N. T. Bariatric surgery in the elderly: 2009–2013. Surg. Obes. Relat. Dis. 11, 393–398 (2015).
Ikramuddin, S. et al. Roux-en-Y gastric bypass versus intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 309, 2240–2249 (2013).
Courcoulas, A. P. et al. Three-year outcomes of bariatric surgery versus lifestyle intervention for type 2 diabetes mellitus treatment: a randomized clinical trial. JAMA Surg. 150, 931–940 (2015).
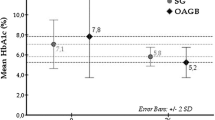
Schauer, P. R. et al. Bariatric surgery versus intensive medical therapy for diabetes — 3 year outcomes. N. Engl. J. Med. 370, 2002–2013 (2014).
Cummings, D. E. et al. Gastric bypass surgery versus intentive lifestyle and medical intervention for type 2 diabetes: the CROSSROADS randomised controlled trial. Diabetologia 59, 945–953 (2016).
Look AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring) 22, 5–13 (2014).
Buchwald, H. et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am. J. Med. 122, 248–256. e5 (2009).
Grundy, S. M. et al. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institue/American Heaty Association conference on scientific issues related to definition. Circulation 109, 433–438 (2004).
Batsis, J. A. et al. Effect of bariatric surgery on the metabolic syndrome: a population-based, long-term controlled study. Mayo Clin. Proc. 83, 897–907 (2008).
Sjostrom, L. et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N. Engl. J. Med. 357, 741–752 (2007).
Sarr, M. G. et al. The EMPOWER study: randomized, prospective, double-blind, ulticentre trial of vagal blockade to induce weight loss in morbid obesity. Obes. Surg. 22, 1771–1782 (2012).
Ponce, J. et al. The REDUCE pivotal trial: a prospective, randomized controlled pivotal trial of a dual intragastric balloon for the treatment of obesity. Surg. Obes. Relat. Dis. 11, 874–878 (2015).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to this Review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Nguyen, N., Varela, J. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol 14, 160–169 (2017). https://doi.org/10.1038/nrgastro.2016.170
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2016.170
This article is cited by
-
A nanoemulsion targeting adipose hypertrophy and hyperplasia shows anti-obesity efficiency in female mice
Nature Communications (2024)
-
Effect of Sleeve Gastrectomy Versus One Anastomosis Gastric Bypass on Postoperative Renal Function and the Urinary Monocyte Chemoattractant Protein-1 (MCP-1) Level
Obesity Surgery (2024)
-
Overview of the Last 71 Years of Metabolic and Bariatric Surgery: Content Analysis and Meta-analysis to Investigate the Topic and Scientific Evolution
Obesity Surgery (2024)
-
Body Fat Depletion: the Yin Paradigm for Treating Type 2 Diabetes
Current Atherosclerosis Reports (2024)
-
Single anastomosis duodeno-ileal bypass with sleeve gastrectomy generates sustained improvement of glycemic control compared with sleeve gastrectomy in the diet-induced obese rat model
Journal of Physiology and Biochemistry (2024)