Abstract
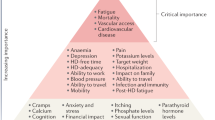
Elderly patients with end-stage renal disease (ESRD) are at increased risk of developing aging-related problems, such as frailty, impaired physical function, falls, poor nutrition and cognitive impairment. These factors affect dialysis outcomes, which can be very poor in frail, elderly patients who often experience a decline in overall health and physical function and have short survival. The default treatment option for these patients is hospital-based hemodialysis, often with little consideration of how this modality will affect the survival or quality of life of individual patients. A comparison of quality of life of elderly patients on hemodialysis versus peritoneal dialysis shows that those on peritoneal dialysis have less illness intrusion. Assisted peritoneal dialysis enables a greater number of frail, elderly patients to have dialysis in their own homes. Dialysis may not extend survival for those with multiple comorbidities, so conservative care (nondialysis treatment) should be considered. To improve the outcomes of elderly patients with ESRD, it is necessary to develop a realistic approach to overall prognosis, quality of life and how the patient copes with the disabilities associated with aging. This approach includes having discussions regarding choice of treatment and end-of-life goals with patients and families.
Key Points
-
Elderly patients with end-stage renal disease have more disabilities associated with old age than do the general population
-
Starting on hemodialysis is associated with a decline in the physical function of frail, elderly patients
-
Elderly patients on peritoneal dialysis have less illness intrusion than elderly patients on hemodialysis
-
Assisted peritoneal dialysis enables a greater number of elderly patients to have their dialysis treatment at home
-
Transplantation can be successful in elderly patients and age is not a contraindication
-
Delaying dialysis and discussing the option of conservative care will improve the quality of the end-of-life phase for elderly patients with multiple comorbidities
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Rowe, J. W. & Kahn, R. L. Successful aging. Gerontologist 37, 433–440 (1997).
Phelan, E. A., Anderson, L. A., LaCroix, A. Z. & Larson, E. B. Older adults' views of “successful aging”—how do they compare with researchers' definitions? J. Am. Geriatr. Soc. 52, 211–216 (2004).
Campbell, A. J. & Buchner, D. M. Unstable disability and the fluctuations of frailty. Age Ageing 26, 315–318 (1997).
Fried, L. P. et al. for the Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, M146–M156 (2001).
Johansen, K. L., Chertow, G. M., Jin, C. & Kutner, N. G. Significance of frailty among dialysis patients. J. Am. Soc. Nephrol. 18, 2960–2967 (2007).
Ansell, D. et al. The Ninth Annual Report. UK Renal Registry [online], (2006).
Ansell, D. et al. The Twelfth Annual Report. UK Renal Registry [online], (2009).
US Renal Data System. USRDS 2010 Annual Data Report: Atlas of End-Stage Renal Disease in the United States [online], (2010).
Challah, S., Wing, A. J., Bauer, R., Morris, R. W. & Schroeder, S. A. Negative selection of patients for dialysis and transplantation in the United Kingdom. Br. Med. J. (Clin. Res. Ed.) 288, 1119–1122 (1984).
Joly, D. et al. Octogenarians reaching end-stage renal disease: cohort study of decision-making and clinical outcomes. J. Am. Soc. Nephrol. 14, 1012–1021 (2003).
Roderick, P. et al. Late referral for end-stage renal disease: a region-wide survey in the south west of England. Nephrol. Dial. Transplant. 17, 1252–1259 (2002).
Kurella, M. et al. Chronic kidney disease and cognitive impairment in the elderly: the Health, Aging, and Body Composition study. J. Am. Soc. Nephrol. 16, 2127–2133 (2005).
Chiu, E., Markowitz, S. N., Cook, W. L. & Jassal, S. V. Visual impairment in elderly patients receiving long-term hemodialysis. Am. J. Kidney Dis. 52, 1131–1138 (2008).
Ifudu, O. et al. Dismal rehabilitation in geriatric inner-city hemodialysis patients. JAMA 271, 29–33 (1994).
Cook, W. L. & Jassal, S. V. Functional dependencies among the elderly on hemodialysis. Kidney Int. 73, 1289–1295 (2008).
Jassal, S. V., Chiu, E. & Hladunewich, M. Loss of independence in patients starting dialysis at 80 years of age or older. N. Engl. J. Med. 361, 1612–1613 (2009).
Kurella Tamura, M. et al. Functional status of elderly adults before and after initiation of dialysis. N. Engl. J. Med. 361, 1539–1547 (2009).
Kurella Tamura, M. & Yaffe, K. Dementia and cognitive impairment in ESRD: diagnostic and therapeutic strategies. Kidney Int. 79, 14–22 (2011).
Murray, A. M. et al. Cognitive impairment in hemodialysis patients is common. Neurology 67, 216–223 (2006).
Plassman, B. L. et al. Prevalence of cognitive impairment without dementia in the United States. Ann. Intern. Med. 148, 427–434 (2008).
Weiner, D. E. The cognition-kidney disease connection: lessons from population-based studies in the United States. Am. J. Kidney Dis. 52, 201–204 (2008).
Madero, M., Gul, A. & Sarnak, M. J. Cognitive function in chronic kidney disease. Semin. Dial. 21, 29–37 (2008).
Pereira, A. A., Weiner, D. E., Scott, T. & Sarnak, M. J. Cognitive function in dialysis patients. Am. J. Kidney Dis. 45, 448–462 (2005).
Kurella, M., Mapes, D. L., Port, F. K. & Chertow, G. M. Correlates and outcomes of dementia among dialysis patients: the Dialysis Outcomes and Practice Patterns Study. Nephrol. Dial. Transplant. 21, 2543–2548 (2006).
Cohen, L. M., Ruthazer, R., Moss, A. H. & Germain, M. J. Predicting six-month mortality for patients who are on maintenance hemodialysis. Clin. J. Am. Soc. Nephrol. 5, 72–79 (2010).
Petersen, R. C. et al. Current concepts in mild cognitive impairment. Arch. Neurol. 58, 1985–1992 (2001).
Sánchez-Perales, C. et al. Ischaemic stroke in incident dialysis patients. Nephrol. Dial. Transplant. 25, 3343–3348 (2010).
Cook, W. L. et al. Falls and fall-related injuries in older dialysis patients. Clin. J. Am. Soc. Nephrol. 1, 1197–1204 (2006).
Tinetti, M. E., Speechley, M. & Ginter, S. F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 319, 1701–1707 (1988).
Power, A. et al. High but stable incidence of subdural haematoma in haemodialysis—a single-centre study. Nephrol. Dial. Transplant. 25, 2272–2275 (2010).
Graham, J. E. et al. Prevalence and severity of cognitive impairment with and without dementia in an elderly population. Lancet 349, 1793–1796 (1997).
Watnick, S., Kirwin, P., Mahnensmith, R. & Concato, J. The prevalence and treatment of depression among patients starting dialysis. Am. J. Kidney Dis. 41, 105–110 (2003).
Charney, D. S. et al. for the Depression and Bipolar Support Alliance. Depression and Bipolar Support Alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch. Gen. Psychiatry 60, 664–672 (2003).
Goodpaster, B. H. et al. The loss of skeletal muscle strength, mass, and quality in older adults: the Health, Aging and Body Composition study. J. Gerontol. A Biol. Sci. Med. Sci. 61, 1059–1064 (2006).
Hughes, V. A., Frontera, W. R., Roubenoff, R., Evans, W. J. & Singh, M. A. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am. J. Clin. Nutr. 76, 473–481 (2002).
Cornoni-Huntley, J. C. et al. An overview of body weight of older persons, including the impact on mortality. The National Health and Nutrition Examination Survey I—Epidemiologic Follow-Up Study. J. Clin. Epidemiol. 44, 743–753 (1991).
Newman, A. B. et al. for the Cardiovascular Study Research Group. Weight change in old age and its association with mortality. J. Am. Geriatr. Soc. 49, 1309–1318 (2001).
Garibotto, G. et al. Skeletal muscle protein synthesis and degradation in patients with chronic renal failure. Kidney Int. 45, 1432–1439 (1994).
Carrero, J. J. et al. Comparison of nutritional and inflammatory markers in dialysis patients with reduced appetite. Am. J. Clin. Nutr. 85, 695–701 (2007).
Ikizler, T. A. Protein and energy: recommended intake and nutrient supplementation in chronic dialysis patients. Semin. Dial. 17, 471–478 (2004).
Aparicio, M. et al. Nutritional status of haemodialysis patients: a French national cooperative study. French Study Group for Nutrition in Dialysis. Nephrol. Dial. Transplant. 14, 1679–1686 (1999).
Cianciaruso, B. et al. Nutritional status in the elderly patient with uraemia. Nephrol. Dial. Transplant. 10 (Suppl. 6), 65–68 (1995).
Marcén, R., Teruel, J. L., de la Cal, M. A. & Gámez, C. The impact of malnutrition in morbidity and mortality in stable haemodialysis patients. Spanish Cooperative Study of Nutrition in Hemodialysis. Nephrol. Dial. Transplant. 12, 2324–2331 (1997).
Qureshi, A. R. et al. Factors predicting malnutrition in hemodialysis patients: a cross-sectional study. Kidney Int. 53, 773–782 (1998).
Stenvinkel, P. et al. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 55, 1899–1911 (1999).
Burrowes, J. D. et al. Cross-sectional relationship between dietary protein and energy intake, nutritional status, functional status, and comorbidity in older versus younger hemodialysis patients. J. Ren. Nutr. 12, 87–95 (2002).
Burrowes, J. D. et al. for the Hemodialysis (HEMO) Study Group. Effects of dietary intake, appetite, and eating habits on dialysis and non-dialysis treatment days in hemodialysis patients: cross-sectional results from the HEMO study. J. Ren. Nutr. 13, 191–198 (2003).
Locher, J. L., Robinson, C. O., Roth, D. L., Ritchie, C. S. & Burgio, K. L. The effect of the presence of others on caloric intake in homebound older adults. J. Gerontol. A Biol. Sci. Med. Sci. 60, 1475–1478 (2005).
Stratton, R. J. et al. Multinutrient oral supplements and tube feeding in maintenance dialysis: a systematic review and meta-analysis. Am. J. Kidney Dis. 46, 387–405 (2005).
Schaeffner, E. S., Rose, C. & Gill, J. S. Access to kidney transplantation among the elderly in the United States: a glass half full, not half empty. Clin. J. Am. Soc. Nephrol. 5, 2109–2114 (2010).
Knoll, G. A. Is kidney transplantation for everyone? The example of the older dialysis patient. Clin. J. Am. Soc. Nephrol. 4, 2040–2044 (2009).
Rao, P. S. et al. Renal transplantation in elderly patients older than 70 years of age: results from the Scientific Registry of Transplant Recipients. Transplantation 83, 1069–1074 (2007).
Heldal, K. et al. Benefit of kidney transplantation beyond 70 years of age. Nephrol. Dial. Transplant. 25, 1680–1687 (2010).
Stevens, K. K. et al. Deceased donor transplantation in the elderly—are we creating false hope? Nephrol. Dial. Transplant. 26, 2382–2386 (2011).
Cohen, B. et al. Expanding the donor pool to increase renal transplantation. Nephrol. Dial. Transplant. 20, 34–41 (2005).
Lindsay, R. M., Heidenheim, P. A., Nesrallah, G., Garg, A. X. & Suri, R. for the Daily Hemodialysis Study Group London Health Sciences Centre. Minutes to recovery after a hemodialysis session: a simple health-related quality of life question that is reliable, valid, and sensitive to change. Clin. J. Am. Soc. Nephrol. 1, 952–959 (2006).
Pisoni, R. L. et al. Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: an instrumental variable analysis. Am. J. Kidney Dis. 53, 475–491 (2009).
Lazarides, M. K., Georgiadis, G. S., Antoniou, G. A. & Staramos, D. N. A meta-analysis of dialysis access outcome in elderly patients. J. Vasc. Surg. 45, 420–426 (2007).
ERA-EDTA. European Renal Association and European Dialysis and Transplant Association annual report 2007 [online], (2009).
Oliver, M. J. et al. Home care assistance and the utilization of peritoneal dialysis. Kidney Int. 71, 673–678 (2007).
Verger, C. et al. French Peritoneal Dialysis Registry (RDPLF): outline and main results. Kidney Int. Suppl. 103, S12–S20 (2006).
Li, P. K. & Szeto, C. C. Success of the peritoneal dialysis programme in Hong Kong. Nephrol. Dial. Transplant. 23, 1475–1478 (2008).
Couchoud, C. et al. Associations between comorbidities, treatment choice and outcome in the elderly with end-stage renal disease. Nephrol. Dial. Transplant. 22, 3246–3254 (2007).
Brown, E. A., Dratwa, M. & Povlsen, J. V. Assisted peritoneal dialysis—an evolving dialysis modality. Nephrol. Dial. Transplant. 22, 3091–3092 (2007).
Kurella, M., Covinsky, K. E., Collins, A. J. & Chertow, G. M. Octogenarians and nonagenarians starting dialysis in the United States. Ann. Intern. Med. 146, 177–183 (2007).
Castrale, C. et al. Peritoneal dialysis in elderly patients: report from the French Peritoneal Dialysis Registry (RDPLF). Nephrol. Dial. Transplant. 25, 255–262 (2010).
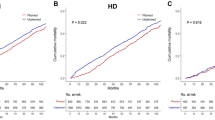
Jassal, S. V., Trpeski, L., Zhu, N., Fenton, S. & Hemmelgarn, B. Changes in survival among elderly patients initiating dialysis from 1990 to 1999. CMAJ 177, 1033–1038 (2007).
Lamping, D. L. et al. Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: a prospective cohort study. Lancet 356, 1543–1550 (2000).
Harris, S. A., Lamping, D. L., Brown, E. A. & Constantinovici, N. for the North Thames Dialysis Study (NTDS) Group. Clinical outcomes and quality of life in elderly patients on peritoneal dialysis versus hemodialysis. Perit. Dial. Int. 22, 463–470 (2002).
Brown, E. A. et al. Broadening Options for Long-term Dialysis in the Elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patients. Nephrol. Dial. Transplant. 25, 3755–3763 (2010).
Rosansky, S. J., Clark, W. F., Eggers, P. & Glassock, R. J. Initiation of dialysis at higher GFRs: is the apparent rising tide of early dialysis harmful or helpful? Kidney Int. 76, 257–261 (2009).
Cooper, B. A. et al. A randomized, controlled trial of early versus late initiation of dialysis. N. Engl. J. Med. 363, 609–619 (2010).
Lassalle, M. et al. Age and comorbidity may explain the paradoxical association of an early dialysis start with poor survival. Kidney Int. 77, 700–707 (2010).
Ahmed, A. K., Kamath, N. S., El Kossi, M. & El Nahas, A. M. The impact of stopping inhibitors of the renin-angiotensin system in patients with advanced chronic kidney disease. Nephrol. Dial. Transplant. 25, 3977–3982 (2010).
Knauf, F. & Aronson, P. S. ESRD as a window into America's cost crisis in health care. J. Am. Soc. Nephrol. 20, 2093–2097 (2009).
Murtagh, F. E. et al. Dialysis or not? A comparative survival study of patients over 75 years with chronic kidney disease stage 5. Nephrol. Dial. Transplant. 22, 1955–1962 (2007).
Chandna, S. M. et al. Survival of elderly patients with stage 5 CKD: comparison of conservative management and renal replacement therapy. Nephrol. Dial. Transplant. 26, 1608–1614 (2011).
Brunori, G. et al. Efficacy and safety of a very-low-protein diet when postponing dialysis in the elderly: a prospective randomized multicenter controlled study. Am. J. Kidney Dis. 49, 569–580 (2007).
Murtagh, F. E., Addington-Hall, J. M. & Higginson, I. J. End-stage renal disease: a new trajectory of functional decline in the last year of life. J. Am. Geriatr. Soc. 59, 304–308 (2011).
Carson, R. C., Juszczak, M., Davenport, A. & Burns, A. Is maximum conservative management an equivalent treatment option to dialysis for elderly patients with significant comorbid disease? Clin. J. Am. Soc. Nephrol. 4, 1611–1619 (2009).
De Vecchi, A. F., Dratwa, M. & Wiedemann, M. E. Healthcare systems and end-stage (ESRD) therapies—an international review: costs and reimbursement/funding of ESRD therapies. Nephrol. Dial. Transplant. 14 (Suppl. 6), 31–41 (1999).
Mendelssohn, D. C. et al. A prospective evaluation of renal replacement therapy modality eligibility. Nephrol. Dial. Transplant. 24, 555–561 (2009).
O'Hare, A. M., Rodriguez, R. A., Hailpern, S. M., Larson, E. B. & Kurella Tamura, M. Regional variation in health care intensity and treatment practices for end-stage renal disease in older adults. JAMA 304, 180–186 (2010).
Schell, J. O., Germain, M. J., Finkelstein, F. O., Tulsky, J. A. & Cohen, L. M. An integrative approach to advanced kidney disease in the elderly. Adv. Chronic Kidney Dis. 17, 368–377 (2010).
Author information
Authors and Affiliations
Contributions
E. A. Brown wrote the article. Both authors researched data for the article, made a substantial contribution to discussion of content and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
E. A. Brown has received speakers bureau honoraria from Baxter Healthcare. L. Johansson declares no competing interests.
Rights and permissions
About this article
Cite this article
Brown, E., Johansson, L. Epidemiology and management of end-stage renal disease in the elderly. Nat Rev Nephrol 7, 591–598 (2011). https://doi.org/10.1038/nrneph.2011.113
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2011.113
This article is cited by
-
Clinical significance of hemodialysis quality of care indicators in very elderly patients with end stage kidney disease
Journal of Nephrology (2022)
-
Assisted peritoneal dialysis: a feasible KRT modality for frail older patients with end-stage kidney disease (ESKD)
Scientific Reports (2021)
-
The effects of megestrol acetate on nutrition, inflammation and quality of life in elderly haemodialysis patients
International Urology and Nephrology (2019)
-
Fistula First Initiative: Historical Impact on Vascular Access Practice Patterns and Influence on Future Vascular Access Care
Cardiovascular Engineering and Technology (2017)
-
Quality of life of elderly patients on peritoneal dialysis versus hemodialysis: a single-center study
Clinical and Experimental Nephrology (2017)