Key Points
-
Urologists frequently encounter patients with multiple and complex comorbidities who are on regular antiplatelet or anticoagulation medication or who have a chronic bleeding disorder
-
Decisions regarding perioperative and postoperative thromboprophylaxis in patients undergoing urological surgery, particularly stone surgery, are frequently met with confusion
-
Systematic thromboprophylaxis with low molecular weight heparin as a subcutaneous injection once daily, until complete mobilization, is recommended in high-risk patients and when lithotripsy is not day case surgery
-
Patients undergoing stone surgery should be stratified into groups according to the risk of bleeding and the risk of thromboembolic events for the respective intervention (high, intermediate and low risk)
-
Bridging therapy should be directed by the inherent risk of bleeding in individual patients, according to American College of Chest Physicians guidelines, as should perioperative treatment with antiplatelet agents
-
A decision algorithm for each lithotripsy modality according to antithrombotic medication used should help the operating surgeon achieve the fine balance required between patient safety and treatment effectiveness
Abstract
With populations ageing and active treatment of urinary stones increasingly in demand, more patients with stones are presenting with an underlying bleeding disorder or need for regular thromboprophylaxis, by means of antiplatelet and other medication. A practical guide to thromboprophylaxis in the treatment of urinary tract lithiasis has not yet been established. Patients can be stratified according to levels of risk of arterial and venous thromboembolism, which influence the requirements for antiplatelet and anticoagulant medications, respectively. Patients should also be stratified according to their risk of bleeding. Consideration of the combined risks of bleeding and thromboembolism should determine the perioperative thromboprophylactic strategy. The choice of shockwave lithotripsy, percutaneous nephrolithotomy or ureteroscopy with laser lithotripsy for treatment of lithiasis should be determined with regard to these risks. Although ureteroscopy is the preferred method in high-risk patients, shockwave lithotripsy and percutaneous nephrolithotomy can be chosen when indicated, if appropriate guidelines are strictly followed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Trinchieri, A. Epidemiology of urolithiasis: an update. Clin. Cases Miner. Bone Metab. 5, 101–106 (2008).
Bartoletti, R. et al. Epidemiology and risk factors in urolithiasis. Urol. Int. 79 (Suppl. 1), 3–7 (2007).
Douketis, J. D. et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141 (Suppl.), e326S–e3250S (2012).
Douketis, J. D. Perioperative anticoagulation management in patients who are receiving oral anticoagulant therapy: a practical guide for clinicians. Thromb. Res. 1081, 3–13 (2002).
Larson, B. J., Zumberg, M. S. & Kitchens, C. S. A feasibility study of continuing dose-reduced warfarin for invasive procedures in patients with high thromboembolic risk. Chest 127, 922–927 (2005).
Siegal, D. et al. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation 126, 1630–1639 (2012).
Schmidt, R. F. & Thews, G. in Human Physiology 2nd edn Ch. 18 (ed. Schmidt, R. F.) 418–425 (Springer, 1989).
Nielsen, J. D., Gram, J., Holm-Nielsen, A., Fabrin, K. & Jespersen, J. Post-operative blood loss after transurethral prostatectomy is dependent on in situ fibrinolysis. Br. J. Urol. 80, 889–893 (1997).
Watson, C. J., Deane, A. M., Doyle, P. T. & Bullock, K. N. Identifiable factors in post-prostatectomy haemorrhage: the role of aspirin. Br. J. Urol. 66, 85–87 (1990).
Ihezue, C. U., Smart, J., Dewbury, K. C., Mehta, R. & Burgess, L. Biopsy of the prostate guided by transrectal ultrasound: relation between warfarin use and incidence of bleeding complications. Clin. Radiol. 60, 459–463 (2005).
Daniels, P. R. Therapy Insight: management of urology patients taking long-term warfarin anticoagulation therapy. Nat. Clin. Pract. Urol. 2, 343–350 (2005).
Turk, C. et al. Guidelines on urolithiasis. Uroweb [online], (2013).
Kovacs, M. J. et al. Single-arm study of bridging therapy with low-molecular-weight heparin for patients at risk of arterial embolism who require temporary interruption of warfarin. Circulation 110, 1658–1663 (2004).
Jaffer, A. K. et al. Low-molecular-weight-heparins as periprocedural anticoagulation for patients on long-term warfarin therapy: a standardized bridging therapy protocol. J. Thromb. Thrombolysis 20, 11–16 (2005).
Gage, B. F. et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 285, 2864–2870 (2001).
Nicolaides, A. N. et al. Prevention and treatment of venous thromboembolism. International consensus statement (guidelines according to scientific evidence). Int. Angiol. 25, 101–161 (2006).
Srisubat, A., Potisat, S., Lojanapiwat, B., Setthawong, V. & Laopaiboon, M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD007044. http://dx.doi.org/10.1002/14651858.CD007044.pub2.
Aboumarzouk, O. M., Somani, B. K. & Monga, M. Flexible ureteroscopy and holmium:YAG laser lithotripsy for stone disease in patients with bleeding diathesis: a systematic review of the literature. Int. Braz. J. Urol. 38, 298–305 (2012).
CMG49: Support for commissioning: anticoagulation therapy. National Institute for Health and Care Excellence (NICE) [online], (2013).
Schnyder-Joris, C., Bonhomme, F., Bonvini, R. & Fontana, P. Perioperative management of new antiplatelet drugs. Rev. Med. Suisse 9, 326–330 (2013).
Gupta, A. D., Streiff, M., Resar, J. & Schoenberg, M. Coronary stent management in elective genitourinary surgery. BJU Int. 110, 480–484 (2012).
Davis, N. F., Fanning, D. M., McGuire, B. B., Carroll, G. T. & Flood, H. D. Perioperative management of chronic anticoagulation therapy in urological patients: a cross-sectional survey of practice. Ir. J. Med. Sci. 180, 823–828 (2011).
Fischer, C., Wöhrle, J., Pastor, J., Morgenroth, K. & Senge, T. Extracorporeal shock-wave lithotripsy induced ultrastructural changes to the renal parenchyma under aspirin use. Electron microscopic findings in the rat kidney. Urologe A 46, 150–155 (2007).
Becopoulos, T., Karayannis, A., Mandalaki, T., Karafoulidou, A. & Markakis, C. Extracorporeal lithotripsy in patients with hemophilia. Eur. Urol. 14, 343–345 (1988).
Ruiz Marcellán, F. J. et al. Extracorporeal shockwave lithotripsy in patients with coagulation disorders. Arch. Esp. Urol. 45, 135–137 (1992).
Ishikawa, J., Okamoto, M., Higashi, Y. & Harada, M. Extracorporeal shock wave lithotripsy in von Willebrand's disease. Int. J. Urol. 3, 58–60 (1996).
Dhar, N. B., Thornton, J., Karafa, M. T. & Streem, S. B. A multivariate analysis of risk factors associated with subcapsular hematoma formation following electromagnetic shock wave lithotripsy. J. Urol. 172, 2271–2274 (2004).
Alivizatos, G. & Skolarikos, A. Is there still a role for open surgery in the management of renal stones? Curr. Opin. Urol. 16, 106–111 (2006).
Skolarikos, A., Alivizatos, G. & de la Rosette, J. Extracorporeal shock wave lithotripsy 25 years later: complications and their prevention. Eur. Urol. 50, 981–990 (2006).
Momose, A., Funyu, T., Takahashi, N. & Suzuki, T. Effect of pressure distribution of shockwave on renal hemorrhage after extracorporeal shockwave lithotripsy: comparison of EDAP LT-01 and Siemens Lithostar. J. Endourol. 13, 165–171 (1999).
Graber, S. F., Danuser, H., Hochreiter, W. W. & Studer, U. E. A prospective randomized trial comparing 2 lithotriptors for stone disintegration and induced renal trauma. J. Urol. 169, 54–57 (2003).
Evan, A. P., McAteer, J. A., Connors, B. A., Blomgren, P. M. & Lingeman, J. E. Renal injury during shock wave lithotripsy is significantly reduced by slowing the rate of shock wave delivery. BJU Int. 100, 624–627 (2007).
Klingler, H. C. et al. Stone treatment and coagulopathy. Eur. Urol. 43, 75–79 (2003).
Zanetti, G. et al. Extracorporeal shockwave lithotripsy in patients treated with antithrombotic agents. J. Endourol. 15, 237–241 (2001).
Sare, G. M., Lloyd, F. R. & Stower, M. J. Life-threatening haemorrhage after extracorporeal shockwave lithotripsy in a patient taking clopidogrel. BJU Int. 90, 469 (2002).
Katz, R., Admon, D. & Pode, D. Life-threatening retroperitoneal hematoma caused by anticoagulant therapy for myocardial infarction after SWL. J. Endourol. 11, 23–25 (1997).
Kukreja, R., Desai, M., Patel, S., Bapat, S. & Desai, M. Factors affecting blood loss during percutaneous nephrolithotomy: prospective study. J. Endourol. 18, 715–722 (2004).
Preminger, G. M. et al. Chapter 1: AUA guideline on management of staghorn calculi: diagnosis and treatment recommendations. J. Urol. 173, 1991–2000 (2005).
Kefer, J. C., Turna, B., Stein, R. J. & Desai, M. M. Safety and efficacy of percutaneous nephrostolithotomy in patients on anticoagulant therapy. J. Urol. 181, 144–148 (2009).
Nerli, R. B., Reddy, M. N., Devaraju, S. & Hiremath, M. B. Percutaneous nephrolithotomy in patients on chronic anticoagulant/antiplatelet therapy. Chonnam Med. J. 48, 103–107 (2012).
Gross, A. J. & Bach, T. Preoperative percutaneous stone surgery in patients receiving anticoagulant therapy. J. Endourol. 23, 1563–1565 (2009).
Van Cangh, P. et al. Management of difficult kidney stones. J. Endourol. 21, 478–489 (2007).
Eberli, D. et al. Urological surgery and antiplatelet drugs after cardiac and cerebrovascular accidents. J. Urol. 183, 2128–2136 (2010).
Kuo, R. L., Aslan, P., Fitzgerald, K. B. & Preminger, G. M. Use of ureteroscopy and holmium:YAG laser in patients with bleeding diatheses. Urology 52, 609–613 (1998).
Watterson, J. D. et al. Safety and efficacy of holmium: YAG laser lithotripsy in patients with bleeding diatheses. J. Urol. 168, 442–445 (2002).
Turna, B. et al. Safety and efficacy of flexible ureterorenoscopy and holmium:YAG lithotripsy for intrarenal stones in anticoagulated cases. J. Urol. 179, 1415–1419 (2008).
Joint Formulary Committee. British National Formulary 65 140–162 (Pharmaceutical Press, 2013).
Author information
Authors and Affiliations
Contributions
A. Bourdoumis, T. Stasinou and S. Kachrilas researched the data for the article. A. Bourdoumis and T. Stasinou provided a substantial contribution to discussions of the content. A. Bourdoumis wrote the article. A. Bourdoumis, S. Kachrilas, A. G. Papatsoris, N. Buchholz and J. Masood contributed to review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Bourdoumis, A., Stasinou, T., Kachrilas, S. et al. Thromboprophylaxis and bleeding diathesis in minimally invasive stone surgery. Nat Rev Urol 11, 51–58 (2014). https://doi.org/10.1038/nrurol.2013.278
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2013.278
This article is cited by
-
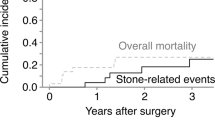
Incidence and risk factors of venous thromboembolism after percutaneous nephrolithotomy: a single-center experience
World Journal of Urology (2021)
-
How can and should we optimize extracorporeal shockwave lithotripsy?
Urolithiasis (2018)
-
Update of the ICUD-SIU consultation on stone technology behind ureteroscopy
World Journal of Urology (2017)
-
S2k-Leitlinie zur Diagnostik, Therapie und Metaphylaxe der Urolithiasis (AWMF 043/025)
Der Urologe (2016)
-
Sky is no limit for ureteroscopy: extending the indications and special circumstances
World Journal of Urology (2015)