Abstract
Background:
We analyzed the potential of abiraterone acetate (henceforth abiraterone) to reduce androgen levels below lower limits of quantification (LLOQ) and explored the association with changes in PSA decline in metastatic castration-resistant prostate cancer (mCRPC) patients.
Methods:
COU-AA-301 is a 2:1 randomized, double-blind, placebo-controlled study comparing abiraterone (1000 mg q.d.) plus low-dose prednisone (5 mg b.i.d.) with placebo plus prednisone in mCRPC patients post docetaxel. Serum testosterone, androstenedione and dehydroepiandrosterone sulfate from baseline to week 12 were measured by novel ultrasensitive two-dimensional liquid chromatography coupled to tandem mass spectrometry assays in a subset of subjects in each arm (abiraterone plus prednisone, n=80; prednisone, n=38). The association between PSA response (⩽50% baseline) and undetectable androgens (week 12 androgen level below LLOQ) was analyzed using logistic regression.
Results:
A significantly greater reduction in serum androgens was observed with abiraterone plus prednisone versus prednisone (all P⩽0.0003), reaching undetectable levels for testosterone (47.2% versus 0%, respectively). A positive association was observed between achieving undetectable serum androgens and PSA decline (testosterone: odds ratio=1.54; 95% confidence interval: 0.546–4.347). Reduction of androgens to undetectable levels did not occur in all patients achieving a PSA response, and a PSA response did not occur in all patients achieving undetectable androgen levels.
Conclusions:
Abiraterone plus prednisone significantly reduced serum androgens, as measured by ultrasensitive assays and was generally associated with PSA response. However, androgen decline did not uniformly predict PSA decline suggesting ligand-independent or other mechanisms for mCRPC progression.
Similar content being viewed by others
Introduction
Sources of androgens that contribute to progressive metastatic castration-resistant prostate cancer (mCRPC) despite medical castration with gonadotropin-releasing hormone agonists/antagonists include the tumor itself, due to upregulation of the androgen biosynthetic machinery, as well as the adrenal glands,1, 2 which are not affected by gonadotropin-releasing hormone agonist/antagonist therapies.3 Abiraterone acetate is metabolized to abiraterone, a selective, orally active inhibitor of 17α-hydroxylase/17,20-lyase (CYP17), a key enzyme in androgen biosynthesis that blocks testicular, adrenal and intratumoral androgen production.4, 5, 6, 7, 8 In the phase III multinational, randomized, double-blind placebo-controlled COU-AA-301 study, abiraterone acetate plus prednisone significantly improved overall survival (OS) by 4.6 months compared with prednisone (hazard ratio=0.74; P<0.0001) in men with mCRPC progressing after docetaxel.9 The results of COU-AA-301 led to regulatory approval of abiraterone acetate plus prednisone for use in mCRPC patients previously treated with docetaxel. This approval was recently expanded to include mCRPC patients who have not received prior chemotherapy, based on results of a subsequent phase III trial (COU-AA-302).10
In a retrospective analysis of COU-AA-301, pretreatment serum androgen levels, measured using a novel ultrasensitive assay based on liquid chromatography and tandem mass spectroscopy, were prognostic of OS in mCRPC patients independent of whether they received abiraterone acetate plus prednisone or prednisone alone.11 In the analysis, the median OS increased in a stepwise manner with increasing quartiles of serum testosterone. Given these findings, an investigation of the post-treatment changes in androgens in patients with available baseline and week-12 data is warranted to explore the extent to which serum androgen suppression and clinical outcome are associated. In the current study we further evaluate the effect of abiraterone acetate and prednisone on serum testosterone, androstenedione and dehydroepiandrosterone sulfate (DHEAS) levels in a subset of patients from the COU-AA-301 study using novel assays and explore the relationship between changes in androgen levels and PSA over time.
Materials and methods
Subjects
The eligibility criteria and study design for the COU-AA-301 study (ClinicalTrials.gov identifier NCT00638690) have been described previously;9, 12 details are provided in the Supplementary Information.
Study design and treatment
COU-AA-301 was a phase III, multinational, 2:1 randomized, double-blind placebo-controlled study of abiraterone acetate (1000 mg q.d. plus prednisone 5 mg orally b.i.d.) versus placebo plus prednisone in men with mCRPC progressing post docetaxel (subjects and study design are described in detail in the Supplementary Information and shown schematically in Supplementary Figure 1).9, 12 The review boards at all participating institutions approved the study, which was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonisation and Good Clinical Practice guidelines. All patients provided written informed consent before participating in the study.
Androgen assays
Serum androgen levels were measured at baseline and at week 12 using liquid–liquid extraction or protein precipitation and two-dimensional liquid chromatography coupled to tandem mass spectrometry ([LC]-LC-MS/MS) by Endocrine Sciences, a Laboratory Corporation of America Company (Calabasas Hills, CA, USA), as described,11 with details provided in the Supplementary Information.
Statistical analysis
The reduction in androgen levels from baseline to week 12 was compared between treatment arms using the Satterthwaite t-test, with statistical significance achieved at P⩽0.05. Adjusted mean androgen levels at baseline and week 12 were also compared between the two arms using a mixed effects model, as androgen level (after log transformation) regressed on treatment, visit of sample collected and the interaction between treatment and time. The association between PSA response and undetectable androgen levels with adjustment for treatment was measured as an odds ratio (OR) using logistic regression, with an OR >1.0 favoring the group with undetectable androgens. No adjustment for multiple testing was used for this exploratory analysis. Association between androgen change (%) and PSA change (%) at week 12 was measured by Spearman’s rank correlation coefficient.
Results
Subjects
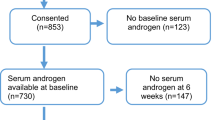
The COU-AA-301 study randomly assigned 1195 patients to study treatment: 797 to abiraterone acetate plus prednisone and 398 to prednisone. Baseline serum androgen levels were obtained in most patients11 and in ∼10% of patients at week 12, a time point frequently used in mCRPC studies as a landmark for measuring response to therapy.13 In this exploratory analysis, 118 patients with available serum androgen data at both baseline and week 12 from 48 trial sites located in the United States and Europe were evaluated, 80 (10.0%) in the abiraterone acetate plus prednisone arm and 38 (9.5%) in the prednisone arm. Patients with only baseline or week 12 androgen data were excluded from analysis. These patients were consecutively accrued and do not represent a selected population with characteristics different from those without 12-week androgens. As previously reported for the entire study cohort, baseline characteristics of the 118 patients were well balanced between treatment arms and were representative of the overall population (Supplementary Table 1). Of this subset of 118 patients, 71.1% had radiographic evidence of disease progression, 45.8% had significant pain present as evidenced by a score ⩾4 on the 0–10 scale of the Brief Pain Inventory-Short Form and 32.2% had received two prior chemotherapies (including docetaxel) before study enrollment.
Baseline values
The mean serum androgen values in each group are presented in Table 1. These values are similar to the baseline values used in a previous analysis of the relationship of baseline androgens to outcome from a data set of nearly all of the 1185 patients enrolled in the study.11
Reduction in serum androgen
The mean androgen levels declined in both treatment arms, and treatment with abiraterone acetate plus prednisone significantly reduced the mean serum androgen levels from baseline to week 12 compared with prednisone alone (Table 1 and Figure 1). The mean serum testosterone was reduced by 90% in the abiraterone acetate plus prednisone arm compared with 49% in the prednisone arm (P<0.0001; Figure 1a); serum androstenedione was reduced by 92% versus 20%, respectively (P=0.0003; Figure 1b); and serum DHEAS was reduced by 86% versus 48%, respectively (P=0.0007; Figure 1c). Comparable results were observed with back-transformed adjusted means in serum androgens estimated in a mixed-effects model (Figure 2).
Box plots of serum androgen levels at baseline and at week 12. The horizontal line within the box indicates the median value and the open circle represents the mean value; the ends of the box show the 25 and 75% quartiles, and the whiskers show the minimum and maximum values. P-values for (a) testosterone, (b) androstenedione and (c) dehydroepiandrosterone sulfate (DHEAS) comparing treatment arms are <0.0001, 0.0003 and 0.0007, respectively.
Adjusted mean values (back-transformed) of serum androgens at baseline and week 12 in mixed-effect model, with the androgen level (after log transformation) regressed on treatment, visit and interaction between treatment and visit. Bars represent 95% confidence intervals. P-values for the adjusted mean difference for testosterone, androstenedione and dehydroepiandrosterone sulfate (DHEAS) were 0.7322, 0.8432 and 0.3904 at baseline and <0.0001 for all androgens at week 12.
The proportions of patients with 30, 50 and 90% reductions in androgen levels at week 12, and the proportions achieving undetectable androgen levels (that is, below lower limits of quantification (LLOQ)), were substantially greater in the abiraterone acetate plus prednisone arm compared with the prednisone arm (Table 2). More than 80% of patients in the abiraterone acetate plus prednisone arm had 90% reductions from baseline to week 12 in serum testosterone, androstenedione and DHEAS, whereas in the prednisone arm only one patient for either testosterone or androstenedione and two for DHEAS had this magnitude of serum androgen decrease. Furthermore, in the abiraterone acetate plus prednisone arm, 47, 30 and 58% of patients achieved undetectable serum testosterone, androstenedione and DHEAS levels at week 12, respectively. In comparison, none of the patients in the prednisone arm achieved undetectable serum testosterone or androstenedione levels, and only one patient (5.3%) had undetectable serum DHEAS.
Association of undetectable androgens with PSA response
PSA response rates were substantially higher in the abiraterone acetate plus prednisone arm compared with the prednisone arm in this subset of patients (Table 3). A decline in PSA was associated with development of undetectable serum androgen levels. Among patients who had a ⩾50% decline in PSA at week 12, an undetectable serum testosterone was observed in 11 of 20 (55.0%); nine of 19 patients (47.4%) had undetectable serum androstenedione, and 13 of 22 patients (59.1%) had undetectable DHEAS. No patients in the prednisone arm developed undetectable serum androgen levels, and there were very few declines in PSA of ⩾50% (testosterone, 2/37 (5.4%); androstenedione, 1/31 (3.2%); DHEAS, 2/38 (5.3%)).
Logistic regression analysis demonstrates that the reduction of androgens to undetectable levels increases the odds of achieving a ⩾50% PSA decline (Table 4). The strongest association was observed for androstenedione, for which patients who achieved undetectable serum levels had a threefold greater likelihood of PSA response compared with those who did not (adjusted OR=3.06; 95% confidence interval: 0.975–9.604). The OR relating undetectable serum testosterone with PSA response was 1.54 (95% confidence interval: 0.546–4.347). However, achieving undetectable serum testosterone was not required for a PSA response with abiraterone acetate (Figure 3), as 15 of 109 patients (14%) experienced a ⩾50% decline in PSA without achieving undetectable testosterone. Similar trends were observed for serum androstenedione and DHEAS (data not shown).
Waterfall plots for maximal PSA change in patients who did and did not achieve undetectable serum testosterone levels. If patient had decreased PSA value on at least one post-baseline visit, maximal PSA change=maximal PSA decrease. If patient had no decreased PSA value on any post-baseline visits, maximal PSA change=maximal PSA increase. *Truncated values.
The Spearman correlations between androgen change and PSA change at week 12 for abiraterone acetate plus prednisone versus prednisone-treated subjects are shown in Table 5. Androgen change and PSA change were positively correlated with Spearman correlations ranging from 0.18 to 0.48. All correlations were significant except from that observed with testosterone or androstenedione in the prednisone arm.
In the prednisone arm, serum androgen levels were variably suppressed, with greatest reductions in serum androgens generally associated with greatest reductions in PSA. Of the 10 patients in the prednisone group with PSA decline, nine showed testosterone decline. However, similar findings were observed in the 26 patients in the prednisone arm without any PSA decline, of whom 25 had testosterone decline. These trends were observed in the abiraterone acetate plus prednisone arm and were consistent for both arms in both the androstenedione and DHEAS groups (Supplementary Table 2).
Relationship of androgen kinetics with radiographic progression-free survival and time to PSA progression
We further examined the relationship between androgen kinetics and mCRPC outcome measures of radiographic progression-free survival and time to PSA progression. In a pooled analysis of both treatment arms, comparing patients with ⩾90% decrease in androgen levels versus patients with lesser androgen declines at 12 weeks led to nonsignificant changes in both radiographic progression-free survival and time to PSA progression, lending more evidence of a potential disconnect between serum androgen levels and disease control (Supplementary Table 3).
Discussion
Abiraterone acetate inhibits the CYP17 enzyme complex, a critical mediator of the conversion of pregnenolone and progesterone to androgens.6 The present data demonstrate that treatment with abiraterone acetate achieved the desired pharmacodynamic effect resulting in reductions of testosterone and other androgens in the vast majority of patients. Reduction of serum androgens was associated with PSA decline in patients receiving abiraterone acetate with prednisone or prednisone alone. Although the reduction of androgens to undetectable levels was more highly associated with PSA declines, achieving post-treatment undetectable androgen levels was not required for a PSA decline to occur, nor was PSA decline always observed. These data support the notion that in those patients in whom reducing serum androgens generate a PSA response to abiraterone acetate, this may occur in conjunction with, or separately from, a reduction in intratumoral androgens, the measurement of which is currently not technically possible in a multicenter clinical trial setting in which tumor biopsy procedures and tissue processing are not standardized. It is apparent from this analysis that androgen decline does not uniformly predict PSA decline, supporting the hypothesis that a variety of mechanisms may lead to progression of mCRPC,14 including some that are ligand-independent.
A recent analysis of the COU-AA-301 study suggested that baseline serum androgens were prognostic of OS in patients with mCRPC, independent of treatment with abiraterone acetate or prednisone alone.11 The median OS increased in a stepwise manner per androgen quartile, ranging from 10.4 months for patients in the lowest quartile of serum testosterone to 18.9 months for those in the highest quartile (P<0.0001), regardless of treatment arm in the study. Similar trends were observed for androstenedione and DHEAS. Somewhat paradoxically, in that analysis, the relative benefit of abiraterone acetate was higher in the patients with lower androgen levels, suggesting that the dynamics of androgen change following abiraterone acetate exposure (for example, the degree of decline) may be more important than the baseline androgen milieu in which the disease had progressed, or that intratumoral androgen production is a more important driver of tumor progression in patients with low serum androgens—and that abiraterone acetate is able to suppress this process. The current analysis therefore enhances these observations by demonstrating the relationship of decline in androgen to decline in PSA in a subset of the population.
The causes for variability in androgen decline in the context of abiraterone acetate therapy merit investigation. Treatment adherence and pharmacologic variables relating to absorption, distribution, metabolism and excretion in particular may affect this. Polymorphisms of CYP17 have been shown to affect prostate cancer incidence15 and may produce some variation in serum androgen levels in mCRPC as well,16, 17 and finally, androgen levels vary according to circadian influence. Recognition of these effects and their incorporation into standard of care may prove useful in optimizing therapy with abiraterone acetate.
Given the previous finding that higher baseline androgen levels are associated with a higher likelihood of achieving a PSA decline of ⩾50% during therapy with abiraterone acetate,11 it is reasonable to hypothesize the presence of a strong positive correlation between androgen decline and PSA decline. The present data demonstrate that, although such a relationship exists, the correlation coefficients were relatively modest (Table 5). Androgen reduction thus serves to confirm that the ‘target’ (CYP17) has been hit; however, the disconnect between androgen reduction and PSA reduction in some patients precludes androgen response from being considered a ‘response measure.’ In addition, abiraterone acetate may exert antitumor activity by mechanisms other than inhibition of androgen production. Further analysis of the relationship of serum androgens to androgen receptor status is ongoing.
Conversely, the observation that lack of response to abiraterone acetate can occur despite near total androgen suppression supports the hypothesis that for many primary resistance to abiraterone acetate may be mostly tumor-mediated (that is, the treatment is hitting the target but the tumor is resistant) as opposed to pharmacodynamic (that is, the drug fails to hit the target, e.g., fails to reduce androgens). This is consistent with prior observations that demonstrated no rise in androgen levels at the time of acquired resistance to abiraterone acetate.18, 19 Further, it is possible that alternate, unmeasured androgens may activate the androgen receptor through a so-called ‘back door’ mechanism. What is not known, however, is the relationship between serum androgen reduction and intratumoral androgen reduction, which remains a key limitation on the development of serum androgens as a biomarker in mCRPC.
The reductions in serum androgens with abiraterone acetate plus prednisone were significantly greater than those observed with prednisone. Although reductions to undetectable levels (that is, less than LLOQ) were frequently observed in the abiraterone acetate plus prednisone arm, this was not required for obtaining a PSA response. Prednisone is also capable of reducing androgen levels, which may account for some of its activity in mCRPC. Prednisone reduces adrenal androgen production via a distinct mechanism from abiraterone acetate, namely inhibition of adrenocorticotropin-mediated adrenal stimulation and not direct CYP17 inhibition.20 Prednisone produced PSA responses in 24% of men with mCRPC who had not received prior chemotherapy in the COU-AA-302 study.10 It should be noted that most patients in the post-chemotherapy COU-301 setting had already been taking prednisone before study entry such that the PSA response to prednisone is expected to be lower than that in an earlier disease setting.
The present analysis of COU-AA-301 considered the impact of reductions in serum androgens as measured by an ultrasensitive assay. The ultrasensitive (LC)-LC-MS/MS assays used in this study allow for the assessment of heterogeneity of serum androgens below castrate levels, a process that was not previously possible because a large proportion of patients had levels <10 ng dl−1, which was considered ‘undetectable’ with prior radioimmunoassays. One commercially available assay (Quest Diagnostics, Madison, NJ, USA) was unable to account for changes in values <1 ng dl−1 (LLOQ=1.0 ng dl−1), whereas those obtained by the current ultrasensitive assay were more precise, showing accurate and reproducible measurement of serum testosterone to an LLOQ of 0.05 ng dl−1.
The relationship between serum androgens and intratumoral androgens, and androgen levels in the tumor microenvironment, is the subject of ongoing investigation.21 In the COU-AA-301 study, above-median baseline serum androgens were associated with better PSA response rates in bivariate and multivariate analyses that accounted for the effects of known prognostic laboratory parameters, including lactate dehydrogenase, hemoglobin, alkaline phosphatase and PSA.11 In a previous phase II study with ketoconazole, baseline serum androstenedione was predictive of PSA responses, with patients who had higher baseline levels more likely to achieve PSA responses than those with lower levels.22 The present analysis considered the change from baseline to week 12; patients achieving undetectable serum androgens appeared more likely to achieve PSA responses and the association between PSA response and undetectable androgen levels was also best observed with androstenedione. This analysis does not have sufficient statistical power to evaluate whether changes in serum androgens are associated with OS. However, the present data, along with our recently published findings showing that baseline androgens are prognostic of OS,11 support further investigation of whether post-treatment reduction of androgens below the previously defined ‘castrate’ testosterone level (that is, <50 ng dl−1)23 are associated with outcome. To address this in the current study, we did an exploratory analysis of OS and radiographic progression-free survival outcomes with undetectable versus detectable androgen levels at week 12 but did not observe a significant difference in the pooled patient population regardless of androgen (Supplementary Table 4). Additional studies will depend on the availability of assays that can detect very low serum androgen levels with accuracy and precision.24, 25, 26 The novel ultrasensitive (LC)-LC-MS/MS assays used in this study have sensitivities of 0.05 ng dl−1 for testosterone, 0.10 ng dl−1 for androstenedione and 0.10 μg dl−1 for DHEAS. These sensitive assays allow for the assessment of the heterogeneity of subcastrate serum androgen levels. Integration of these assays into standard clinical practice may be possible following validation of these results.
In summary, the present data establish an association between reduction in serum androgens and PSA change during CYP17 inhibitor therapy and further support the continued development of serum androgens, measured by ultrasensitive techniques, as pharmacodynamic biomarkers in mCRPC.
References
Bonkhoff H, Berges R . From pathogenesis to prevention of castration resistant prostate cancer. Prostate 2010; 70: 100–112.
Van Allen EM, Ryan CJ . Novel secondary hormonal therapy in advanced prostate cancer: an update. Curr Opin Urol 2009; 19: 315–321.
Hofland J, van Weerden WM, Dits NF, Steenbergen J, van Leenders GJ, Jenster G et al. Evidence of limited contributions for intratumoral steroidogenesis in prostate cancer. Cancer Res 2010; 70: 1256–1264.
Attard G, Reid AH, A'Hern R, Parker C, Oommen NB, Folkerd E et al. Selective inhibition of CYP17 with abiraterone acetate is highly active in the treatment of castration-resistant prostate cancer. J Clin Oncol 2009; 27: 3742–3748.
Danila DC, Morris MJ, de Bono JS, Ryan CJ, Denmeade SR, Smith MR et al. Phase II multicenter study of abiraterone acetate plus prednisone therapy in patients with docetaxel-treated castration-resistant prostate cancer. J Clin Oncol 2010; 28: 1496–1501.
O'Donnell A, Judson I, Dowsett M, Raynaud F, Dearnaley D, Mason M et al. Hormonal impact of the 17alpha-hydroxylase/C(17,20)-lyase inhibitor abiraterone acetate (CB7630) in patients with prostate cancer. Br J Cancer 2004; 90: 2317–2325.
Reid AH, Attard G, Danila DC, Oommen NB, Olmos D, Fong PC et al. Significant and sustained antitumor activity in post-docetaxel, castration-resistant prostate cancer with the CYP17 inhibitor abiraterone acetate. J Clin Oncol 2010; 28: 1489–1495.
Ryan CJ, Shah S, Efstathiou E, Smith MR, Taplin ME, Bubley GJ et al. Phase II study of abiraterone acetate in chemotherapy-naive metastatic castration-resistant prostate cancer displaying bone flare discordant with serologic response. Clin Cancer Res 2011; 17: 4854–4861.
Fizazi K, Scher HI, Molina A, Logothetis CJ, Chi KN, Jones RJ et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol 2012; 13: 983–992.
Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med 2013; 368: 138–148.
Ryan CJ, Molina A, Li J, Kheoh T, Small EJ, Haqq CM et al. Serum androgens as prognostic biomarkers in castration-resistant prostate cancer: results from an analysis of a randomized phase III trial. J Clin Oncol 2013; 31: 2791–2798.
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 2011; 364: 1995–2005.
Scher HI, Kelly WM, Zhang ZF, Ouyang P, Sun M, Schwartz M et al. Post-therapy serum prostate-specific antigen level and survival in patients with androgen-independent prostate cancer. J Natl Cancer Inst 1999; 91: 244–251.
Ryan CJ, Tindall DJ . Androgen receptor rediscovered: the new biology and targeting the androgen receptor therapeutically. J Clin Oncol 2011; 29: 3651–3658.
Stanford JL, Noonan EA, Iwasaki L, Kolb S, Chadwick RB, Feng Z et al. A polymorphism in the CYP17 gene and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev 2002; 11: 243–247.
Hamada A, Danesi R, Price DK, Sissung T, Chau C, Venzon D et al. Association of a CYP17 polymorphism with overall survival in Caucasian patients with androgen-independent prostate cancer. Urology 2007; 70: 217–220.
Wright JL, Kwon EM, Lin DW, Kolb S, Koopmeiners JS, Feng Z et al. CYP17 polymorphisms and prostate cancer outcomes. Prostate 2010; 70: 1094–1101.
Attard G, Reid AH, Yap TA, Raynaud F, Dowsett M, Settatree S et al. Phase I clinical trial of a selective inhibitor of CYP17, abiraterone acetate, confirms that castration-resistant prostate cancer commonly remains hormone driven. J Clin Oncol 2008; 26: 4563–4571.
Ryan CJ, Smith MR, Fong L, Rosenberg JE, Kantoff P, Raynaud F et al. Phase I clinical trial of the CYP17 inhibitor abiraterone acetate demonstrating clinical activity in patients with castration-resistant prostate cancer who received prior ketoconazole therapy. J Clin Oncol 2010; 28: 1481–1488.
Russell GM, Henley DE, Leendertz J, Douthwaite JA, Wood SA, Stevens A et al. Rapid glucocorticoid receptor-mediated inhibition of hypothalamic-pituitary-adrenal ultradian activity in healthy males. J Neurosci 2010; 30: 6106–6115.
Efstathiou E, Titus M, Tsavachidou D, Tzelepi V, Wen S, Hoang A et al. Effects of abiraterone acetate on androgen signaling in castrate-resistant prostate cancer in bone. J Clin Oncol 2012; 30: 637–643.
Ryan CJ, Halabi S, Ou SS, Vogelzang NJ, Kantoff P, Small EJ . Adrenal androgen levels as predictors of outcome in prostate cancer patients treated with ketoconazole plus antiandrogen withdrawal: results from a cancer and leukemia group B study. Clin Cancer Res 2007; 13: 2030–2037.
Scher HI, Halabi S, Tannock I, Higano C, Bubley GJ, Dreicer R et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 2008; 26: 1148–1159.
Leppert JT, Lam JS, Butch AW, Belldegrun AS . The sensitivity of testosterone immunoassays and their role in monitoring antiandrogen therapy. Urol Oncol 2006; 24: 277–278.
Matsumoto AM, Bremner WJ . Serum testosterone assays–accuracy matters. J Clin Endocrinol Metab 2004; 89: 520–524.
Vesper HW, Bhasin S, Wang C, Tai SS, Dodge LA, Singh RJ et al. Interlaboratory comparison study of serum total testosterone [corrected] measurements performed by mass spectrometry methods. Steroids 2009; 74: 498–503.
Acknowledgements
This study was funded by Ortho Biotech Oncology Research & Development unit of Cougar Biotechnology (now Janssen Research & Development). We are grateful to Russell P Grant, PhD, of Endocrine Sciences, a Laboratory Corporation of America Company (Calabasas Hills, CA, USA) for his role in the development and validation of the androgen assay that led to its inclusion in this study, and for his critical review of this manuscript. Writing assistance was provided by Ira Mills, PhD, of PAREXEL, and was funded by Janssen Global Services, LLC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
C J Ryan has received honoraria from Janssen Pharmaceuticals. W Peng is an employee of Janssen Research & Development. T Kheoh and A Molina are employees of Janssen Research & Development and own stock in Johnson & Johnson. C M Haqq owns stock in Johnson & Johnson. D W Chandler is an employee of LabCorp and owns stock in LabCorp. H I Scher has served as a consultant (uncompensated) for Aragon Pharmaceuticals, Celgene, Orion Pharmaceuticals, Johnson & Johnson Pharmaceutical Development, Medivation and Veridex (now Janssen Research & Development); is a consultant (compensated) for Enzon, Millennium and Ortho Biotech Oncology Research and Development; and has received institutional support for research funding from Aragon Pharmaceuticals, Janssen Research & Development, Medivation and Veridex (now Janssen Research & Development). E Welkowsky declares no conflict of interest.
Additional information
Presented in part at the American Association for Cancer Research Annual Meeting, 31 March 2012 to 4 April 2012, Chicago, IL, USA.
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Ryan, C., Peng, W., Kheoh, T. et al. Androgen dynamics and serum PSA in patients treated with abiraterone acetate. Prostate Cancer Prostatic Dis 17, 192–198 (2014). https://doi.org/10.1038/pcan.2014.8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2014.8
This article is cited by
-
LHRH sparing therapy in patients with chemotherapy-naïve, mCRPC treated with abiraterone acetate plus prednisone: results of the randomized phase II SPARE trial
Prostate Cancer and Prostatic Diseases (2022)
-
The role of glucocorticoid receptor in prostate cancer progression: from bench to bedside
International Urology and Nephrology (2017)
-
Modeling the Relationship Between Exposure to Abiraterone and Prostate-Specific Antigen Dynamics in Patients with Metastatic Castration-Resistant Prostate Cancer
Clinical Pharmacokinetics (2017)
-
Therapieerfolg basiert auf der Androgendeprivation
Uro-News (2016)
-
An Update on Triptorelin: Current Thinking on Androgen Deprivation Therapy for Prostate Cancer
Advances in Therapy (2016)