Abstract
Background:
Active surveillance (AS) is commonly based on standard 10–12-core prostate biopsies, which misclassify ~50% of cases compared with radical prostatectomy. We assessed the value of multiparametric magnetic resonance imaging (mpMRI)-targeted transperineal fusion-biopsies in men under AS.
Methods:
In all, 149 low-risk prostate cancer (PC) patients were included in AS between 2010 and 2015. Forty-five patients were initially diagnosed by combined 24-core systematic transperineal saturation biopsy (SB) and MRI/transurethral ultrasound (TRUS)-fusion targeted lesion biopsy (TB). A total of 104 patients first underwent 12-core TRUS-biopsy. All patients were followed-up by combined SB and TB for restratification after 1 and 2 years. All mpMRI examinations were analyzed using PIRADS. AS was performed according to PRIAS-criteria and a NIH-nomogram for AS-disqualification was investigated. AS-disqualification rates for men initially diagnosed by standard or fusion biopsy were compared using Kaplan–Meier estimates and log-rank tests. Differences in detection rates of the SB and TB components were evaluated with a paired-sample analysis. Regression analyses were performed to predict AS-disqualification.
Results:
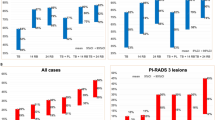
A total of, 48.1% of patients diagnosed by 12-core TRUS-biopsy were disqualified from AS based on the MRI/TRUS-fusion biopsy results. In the initial fusion-biopsy cohort, upgrading occurred significantly less frequently during 2-year follow-up (20%, P<0.001). TBs alone were significantly superior compared with SBs alone to detect Gleason-score-upgrading. NPV for Gleason-upgrading was 93.5% for PIRADS⩽2. PSA level, PSA density, NIH-nomogram, initial PIRADS score (P<0.001 each) and PIRADS-progression on consecutive MRI (P=0.007) were significant predictors of AS-disqualification.
Conclusions:
Standard TRUS-biopsies lead to significant underestimation of PC under AS. MRI/TRUS-fusion biopsies, and especially the TB component allow more reliable risk classification, leading to a significantly decreased chance of subsequent AS-disqualification. Cancer detection with mpMRI alone is not yet sensitive enough to omit SB on follow-up after initial 12-core TRUS-biopsy. After MRI/TRUS-fusion biopsy confirmed AS, it may be appropriate to biopsy only those men with suspected progression on MRI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Rider JR, Sandin F, Andrén O, Wiklund P, Hugosson J, Stattin P . Long-term outcomes among noncuratively treated men according to prostate cancer risk category in a nationwide, population-based study. Eur Urol 2013; 63: 88–96.
Choo R, Klotz L, Danjoux C, Morton GC, DeBoer G, Szumacher E et al. Feasibility study: watchful waiting for localized low to intermediate grade prostate carcinoma with selective delayed intervention based on prostate specific antigen, histological and/or clinical progression. J Urol 2002; 167: 1664–1669.
Klotz L, Vesprini D, Sethukavalan P, Jethava V, Zhang L, Jain S et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol 2014; 33: 272–277.
Ploussard G, Epstein JI, Montironi R, Carroll PR, Wirth M, Grimm M-O et al. The contemporary concept of significant versus insignificant prostate cancer. Eur Urol 2011; 60: 291–303.
Shaw GL, Thomas BC, Dawson SN, Srivastava G, Vowler SL, Gnanapragasam VJ et al. Identification of pathologically insignificant prostate cancer is not accurate in unscreened men. Br J Cancer 2014; 110: 2405–2411.
Turkbey B, Mani H, Shah V, Rastinehad AR, Bernardo M, Pohida T et al. Multiparametric 3 T prostate magnetic resonance imaging to detect cancer: histopathological correlation using prostatectomy specimens processed in customized magnetic resonance imaging based molds. J Urol 2011; 186: 1818–1824.
Moore CM, Kasivisvanathan V, Eggener S, Emberton M, Futterer JJ, Gill IS et al. Standards of reporting for MRI-targeted biopsy studies (START) of the prostate: recommendations from an International Working Group. Eur Urol 2013; 64: 544–552.
De Rooij M, Hamoen EHJ, Fütterer JJ, Barentsz JO, Rovers MM . Accuracy of multiparametric MRI for prostate cancer detection: a meta-analysis. Am J Roentgenol 2014; 202: 343–351.
Turkbey B, Pinto PA, Mani H, Bernardo M, Pang Y, McKinney YL et al. Prostate cancer: value of multiparametric MR imaging at 3 T for detection–histopathologic correlation. Radiology 2010; 255: 89–99.
Rosenkrantz AB, Deng FM, Kim S, Lim RP, Hindman N, Mussi TC et al. Prostate cancer: multiparametric MRI for index lesion localization—a multiple-reader study. Am J Roentgenol 2012; 199: 830–837.
Le JD, Tan N, Shkolyar E, Lu DY, Kwan L, Marks LS et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol 2014; 67: 569–576.
Baco E, Ukimura O, Rud E, Vlatkovic L, Svindland A, Aron M et al. Magnetic resonance imaging-transectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol 2014; 67: 787–794.
Delongchamps NB, Lefèvre A, Bouazza N, Beuvon F, Legman P, Cornud F . Detection of significant prostate cancer with magnetic resonance targeted biopsies—should transrectal ultrasound-magnetic resonance imaging fusion guided biopsies alone be a standard of care? J Urol 2014; 193: 1198–1204.
Vargas HA, Akin O, Afaq A, Goldman D, Zheng J, Moskowitz CS et al. Magnetic resonance imaging for predicting prostate biopsy findings in patients considered for active surveillance of clinically low risk prostate cancer. J Urol 2012; 188: 1732–1738.
Hu JC, Chang E, Natarajan S, Margolis DJ, Macairan M, Lieu P et al. Targeted prostate biopsy in select men for active surveillance: do the Epstein criteria still apply? J Urol 2014; 192: 385–390.
Schoots IG, Petrides N, Giganti F, Bokhorst LP, Rannikko A, Klotz L et al. Magnetic resonance imaging in active surveillance of prostate cancer: a systematic review. Eur Urol 2014; 67: 67–73.
Van den Bergh RCN, Roemeling S, Roobol MJ, Roobol W, Schröder FH, Bangma CH . Prospective validation of active surveillance in prostate cancer: the PRIAS study. Eur Urol 2007; 52: 1560–1563.
Stamatakis L, Siddiqui MM, Nix JW, Logan J, Rais-Bahrami S, Walton-Diaz A et al. Accuracy of multiparametric magnetic resonance imaging in confirming eligibility for active surveillance for men with prostate cancer. Cancer 2013; 119: 3359–3366.
Siddiqui MM, Truong H, Rais-Bahrami S, Stamatakis L, Logan J, Walton-Diaz A et al. Clinical implications of a multiparametric MRI based nomogram applied to prostate cancer active surveillance. J Urol 2015; 193: 1943–1949.
Kuru TH, Roethke MC, Seidenader J, Simpfendorfer T, Boxler S, Alammar K et al. Critical evaluation of magnetic resonance imaging targeted, transrectal ultrasound guided transperineal fusion biopsy for detection of prostate cancer. J Urol 2013; 190: 1380–1386.
Radtke JP, Kuru TH, Boxler S, Alt CD, Popeneciu IV, Huettenbrink C et al. Comparative analysis of transperineal template saturation prostate biopsy versus magnetic resonance imaging targeted biopsy with magnetic resonance imaging-ultrasound fusion guidance. J Urol 2015; 193: 87–94.
Barentsz JO, Richenberg J, Clements R, Choyke P, Verma S, Villeirs G et al. ESUR prostate MR guidelines 2012. Eur Radiol 2012 22: 746–757.
Van der Kwast TH, Amin MB, Billis A, Epstein JI, Griffiths DF, Humphrey PA et al. International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. working group 1: specimen handling. Mod Pathol 2011; 24: 16–25.
Tango T . Equivalence test and confidence interval for the difference in proportions for the paired-sample design. Stat Med 1998; 17: 891–908.
R Development Core Team R. R: a language and environment for statistical computing. R Found Stat Comput 2014; 1: 409.
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis Ca, Glasziou PP, Irwig LM et al. Towards complete and,accurate reporting of studies of diagnostic accuracy: the STARD initiative. Radiology 2003; 226: 24–28.
Ouzzane A, Renard-Penna R, Marliere F, Mozer P, Olivier J, Barkatz J et al. MRI-targeted biopsy improves selection of patients considered for active surveillance for clinically low-risk prostate cancer based on systematic biopsies. J Urol 2015; 194: 350–356.
Barzell WE, Melamed MR, Cathcart P, Moore CM, Ahmed HU, Emberton M . Identifying candidates for active surveillance: an evaluation of the repeat biopsy strategy for men with favorable risk prostate cancer. J Urol 2012; 188: 762–767.
Turkbey B, Mani H, Aras O, Ho J, Hoang A, Rastinehad AR et al. Prostate cancer: can multiparametric MR imaging help identify patients who are candidates for active surveillance? Radiology 2013; 268: 144–152.
Villa L, Salonia A, Capitanio U, Scattoni V, Abdollah F, Suardi N et al. The Number of cores at first biopsy may suggest the need for a con fi rmatory decision making in the real-life setting. Urology 2014; 84: 634–641.
Ploussard G, Xylinas E, Salomon L, Allory Y, Vordos D, Hoznek A et al. The role of biopsy core number in selecting prostate cancer patients for active surveillance. Eur Urol 2009; 56: 891–898.
Mullins JK, Bonekamp D, Landis P, Begum H, Partin AW, Epstein JI et al. Multiparametric magnetic resonance imaging findings in men with low-risk prostate cancer followed using active surveillance. BJU Int 2013; 111: 1037–1045.
Dianat SS, Carter HB, Pienta KJ, Schaeffer EM, Landis PK, Epstein JI et al. Magnetic resonance e invisible versus magnetic resonance e visible prostate cancer in active surveillance: a preliminary report on disease outcomes. Urology 2015; 85: 147–154.
Park BH, Jeon HG, Choo SH, Jeong BC, Seo SI, Jeon SS et al. Role of multiparametric 3.0-Tesla magnetic resonance imaging in patients with prostate cancer eligible for active surveillance. BJU Int 2014; 113: 864–870.
Da Rosa MR, Milot L, Sugar L, Vesprini D, Chung H, Loblaw A et al. A prospective comparison of MRI-US fused targeted biopsy versus systematic ultrasound-guided biopsy for detecting clinically significant prostate cancer in patients on active surveillance. J Magn Reson Imaging 2015; 41: 220–225.
Baco E, Ukimura O, Rud E, Vlatkovic L, Svindland A, Aron M et al. Magnetic resonance imaging–transectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol 2015; 67: 787–794.
Thompson JE, Moses D, Shnier R, Brenner P, Delprado W, Ponsky L et al. Multiparametric magnetic resonance imaging guided diagnostic biopsy detects significant prostate cancer and could reduce unnecessary biopsies and over detection: a prospective study. J Urol 2014; 192: 67–74.
Walton Diaz A, Shakir NA, George AK, Rais-Bahrami S, Turkbey B, Rothwax JT et al. Use of serial multiparametric magnetic resonance imaging in the management of patients with prostate cancer on active surveillance. Urol Oncol Semin Orig Investig 2015; 33: 202.e1–202.e7.
Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MGM . Magnetic resonance imaging–targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol 2014; 68: 438–450.
Guo R, Cai L, Fan Y, Jin J, Zhou L, Zhang K . Magnetic resonance imaging on disease reclassification among active surveillance candidates with low-risk prostate cancer: a diagnostic meta-analysis. Prostate Cancer Prostatic Dis 2015; 18: 221–228.
Cary KC, Cowan JE, Sanford M, Shinohara K, Perez N, Chan JM et al. Predictors of pathologic progression on biopsy among men on active surveillance for localized prostate cancer: the value of the pattern of surveillance biopsies. Eur Urol 2014; 66: 337–342.
Dinh KT, Mahal Ba, Ziehr DR, Muralidhar V, Chen Y-W, Viswanathan VB et al. Incidence and predictors of upgrading and upstaging among 10,000 contemporary patients with low-risk prostate cancer. J Urol 2015; 194: 343–349.
Anderson CB, Sternberg IA, Karen-Paz G, Kim PH, Sjoberg D, Vargas HA et al. Age is associated with upgrading at confirmatory biopsy among men with prostate cancer treated with active surveillance. J Urol 2015; 194: 1607–1611.
Suardi N, Gallina A, Capitanio U, Salonia A, Lughezzani G, Freschi M et al. Age-adjusted validation of the most stringent criteria for active surveillance in low-risk prostate cancer patients. Cancer 2012; 118: 973–980.
Klotz L . Nomogram for predicting survival in men with clinically localized prostate cancer who do not undergo definitive therapy. Nat Clin Pract Urol 2008; 5: 362–363.
Ankerst DP, Xia J, Thompson IM, Hoefler J, Newcomb LF, Brooks JD et al. Precision medicine in active surveillance for prostate cancer: development of the canary–early detection research network active surveillance biopsy risk calculator. Eur Urol 2015; 68: 1083–1088.
Carter HB, Kettermann A, Warlick C, Metter EJ, Landis P, Walsh PC et al. Expectant management of prostate cancer with curative intent: an update of the Johns Hopkins experience. J Urol 2007; 178: 2359–2365.
Pham KN, Porter CR, Odem-Davis K, Wolff EM, Jeldres C, Wei JT et al. Transperineal template guided prostate biopsy selects candidates for active surveillance—how many cores are enough? J Urol 2015; 194: 674–679.
Reese AC, Landis P, Han M, Epstein JI, Carter HB . Expanded criteria to identify men eligible for active surveillance of low risk prostate cancer at Johns Hopkins: a preliminary analysis. J Urol 2013; 190: 2033–2038.
Ploussard G, Isbarn H, Briganti A, Sooriakumaran P, Surcel CI, Salomon L et al. Can we expand active surveillance criteria to include biopsy Gleason 3+4 prostate cancer? A multi-institutional study of 2,323 patients. Urol Oncol Semin Orig Investig 2015; 33: 71.e1–71.e9.
Acknowledgements
We cordially thank Mrs. Diana Tichy (Division of Biostatistics, German Cancer Research Center, Heidelberg, Germany) for statistical advice and support. BAH is grateful for funding from the German Research Foundation and the European Foundation for Urology.
DISCLOSURE
None of the funding sources had any input whatsoever into this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
BAH has received research funding from MedCom and Uromed. The remaining authors declare on conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Rights and permissions
About this article
Cite this article
Radtke, J., Kuru, T., Bonekamp, D. et al. Further reduction of disqualification rates by additional MRI-targeted biopsy with transperineal saturation biopsy compared with standard 12-core systematic biopsies for the selection of prostate cancer patients for active surveillance. Prostate Cancer Prostatic Dis 19, 283–291 (2016). https://doi.org/10.1038/pcan.2016.16
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.16
This article is cited by
-
Multiparametrische MRT und alternative Methoden in der Interventions- und Behandlungsplanung beim Prostatakarzinom
Die Urologie (2023)
-
The current role of MRI for guiding active surveillance in prostate cancer
Nature Reviews Urology (2022)
-
Accuracy of the magnetic resonance imaging pathway in the detection of prostate cancer: a systematic review and meta-analysis
Prostate Cancer and Prostatic Diseases (2019)
-
MRI in active surveillance: a critical review
Prostate Cancer and Prostatic Diseases (2019)
-
Role of multiparametric magnetic resonance imaging for patients under active surveillance for prostate cancer: a systematic review with diagnostic meta-analysis
Prostate Cancer and Prostatic Diseases (2019)