Abstract
Background
Hypertension occurs in up to 3% of neonates admitted to the Neonatal Intensive Care Unit (NICU), and is a potentially under-recognized condition. The aim of this study was to examine the incidence of documented and undiagnosed hypertension from the 24-center Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN) database, and to assess risk factors for hypertension according to gestational age.
Methods
Diagnosed hypertension was documented if an infant had a discharge diagnosis of hypertension and/or discharged on antihypertensive medications. Undiagnosed hypertension was defined when infants did not have a diagnosis of hypertension, but >50% of the lowest mean, diastolic and systolic blood pressure recordings were >95th percentile for gestational age.
Results
Of the 2162 neonates enrolled in the study, hypertension was documented in 1.8%. An additional 3.7% were defined as having undiagnosed hypertension. There was a significant correlation with neonatal hypertension and acute kidney injury (AKI). Additional risk factors for neonatal hypertension were hyperbilirubinaemia, Caucasian race, outborn, vaginal delivery, and congenital heart disease. Protective factors were small for gestational age, multiple gestations, and steroids for fetal maturation.
Conclusions
Neonatal hypertension may be an under-recognized condition. AKI and other risk factors predispose infants to hypertension.
Similar content being viewed by others
Introduction
Adelman first reported neonatal hypertension in the 1970s and since then advances in medicine and the practice of Neonatology have led to an increased awareness of neonatal hypertension in Neonatal Intensive Care Unit (NICU) graduates.1,2,3 The diagnosis of hypertension is considered if the systolic blood pressure (BP) is above the 95th percentile on three separate occasions for newborn infants of similar gestational or postconceptional age and size.1,2,4,5 Although relatively uncommon in healthy term infants, hypertension in the term or pre-term neonate may be seen in up to 0.2–3% of all neonates admitted to the NICU.2,3,6,7,8,9
The definition of neonatal hypertension is not standardized, and defining what is considered normative BP in newborns is a complex task, as studies in both term and pre-term infants indicate that BP increases with both gestational and postconceptional age, as well as with birthweight and length.1,2,4,10,11 Most studies to date investigating the incidence of neonatal hypertension have been single center studies, whereby the incidence varies with the population studied. Additionally, the measurement of BP in infancy is infrequently and inadequately performed, which may affect the results achieved and lead to the under-diagnosis of neonatal hypertension.12,13
To date there have been no large, multicenter studies defining neonatal hypertension and determining the incidence in NICU graduates. Previous cut-offs for BP were defined in the 1970s and 1990s by Adelman et.al and Zubrow et.al, providing guidelines that have been potentially outdated by technology and an increased awareness of hypertension in neonates.14,15 The aims of this study were to: (1) examine the incidence of documented neonatal hypertension according to gestational age; (2) assess the antenatal and postnatal risk factors (specifically acute kidney injury (AKI)) for neonatal hypertension according to gestational age; and (3) determine the incidence of potentially undiagnosed neonatal hypertension according to gestational age from a large, multicenter cohort. The primary hypotheses of this study were to test whether a proportion of neonates may have undiagnosed hypertension and whether infants with the risk factor of AKI developed hypertension after controlling for multiple confounders.
Method
Data for this study was extracted from the Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN) database, which is a multicenter, international, retrospective cohort study.16 Twenty-four level 2–4 NICUs in the United States (n = 20), Canada (n = 2), India (n = 1), and Australia (n = 1) participated in AWAKEN. A full description of the AWAKEN cohort16 and the incidence and outcome of AKI in the AWAKEN cohort17 have been recently published. Each center involved in the study had received approval from their Institutional Review Board or Human Research Ethics Committee.
Subjects
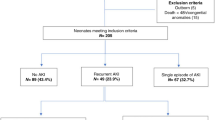
All infants who met the inclusion and exclusion criteria at each of the 24 participating centers from 1 January 2014 until 31 March 2014 were enrolled. The endpoints of the study were: discharge to home, transfer to another facility, or out of the NICU for escalating or convalescent care, death, or survival at 120 days of age. The exclusion criteria of the AWAKEN study included; not admitted to NICU, no intravenous fluids (IVFs) for at least 48 h, age > 14 days at NICU admission, lethal chromosomal anomaly, congenital heart disease with surgery at <7 days of life, and mortality at <48 h. Neonates diagnosed with severe congenital anomalies of the kidney and urinary tract were also excluded. Figure 1 outlines the inclusion and exclusion criteria.16
BP was captured from all infants during the first week of life, and the highest and lowest BP for each of the three metrics (systolic, diastolic, and mean) were recorded. During subsequent weeks of enrollment, data were captured from a given day of the week, and the highest and lowest BP for each of the three metrics were recorded. The AWAKEN study captured data from the medical record and did not dictate the methods for measurement, thus, we can assume that there were variations in BP measurement from center to center and from infant to infant, and from day to day.
Definition of definite hypertension
Was defined if an infant had a discharge diagnosis of hypertension and/or discharged home on antihypertensive agents.
Definition of undiagnosed hypertension
A literature review was performed and the 95th percentile systolic BP, diastolic BP, and mean BP were designated for gestational age at day 1, day 4, week 1, week 2, week 3, week 4 of life, and at discharge (Table 1).12,18,19,20,21,22,23 Undiagnosed hypertension was conservatively derived with more than 50% of all the lowest readings (systolic, diastolic and mean) throughout the admission needing to above the 95th centile for postconceptual age (Table 1)
Definition of AKI
The definition for AKI was based on the KDIGO definition for adults and children which includes: a rise in serum creatinine of ≥0.3 mg/dl from the lowest previous value, a 50% rise in serum creatinine from the lowest previous value and/or urine output of <1 cc/kg/hour.16 This definition has been used in neonatal studies and was proposed by Jetton and Askenazi in 2012.24 A recent review by neonatal and nephrology experts proposed that this definition be used as an empiric definition until further data was available to refine it.25
Statistical analyses
Data management and statistical analysis was performed at the University of Alabama in Birmingham using SAS software v9.4. Descriptive analysis was used to identify the incidence of neonatal hypertension within the AWAKEN population. Categorical variables were analyzed by proportional differences with the Chi-square or Fisher exact test (where appropriate). All continuous variables were tested for normality using the Shapiro–Wilk test. For normally distributed continuous variables, the mean and standard deviation (SD) were reported and analyzed using the Student's t-test. For non-normally distributed continuous variables, the median and interquartile range (IQR) were reported, and groups were compared using the Wilcoxon Signed Ranks test. Logistic regression was used to calculate crude odds ratio (OR) and associated 95% confidence intervals (CI) for the independent association between AKI and the likelihood of developing hypertension. Forward stepwise logistic regression model for hypertension was built using a significance level of entry of p < 0.1. Crude and adjusted odds ratios (OR) for variables that remained in the final model are reported. Variables considered for regression modeling included AKI, race, gestational age, birth weight, delivery site, admission for respiratory symptoms or failure, admission for hyperbilirubinaemia, admission for congenital heart disease, small for gestational age, multiple gestation, and maternal steroids for fetal maturation.
Results
Demographics of the entire cohort
A total of 2162 neonates were enrolled in the study. There were 1229 males (56.8%) and 933 females (43.2%). The mean gestational age was significantly higher in the hypertensive group than for the control group (34.9 ± 4.6 weeks vs 34 ± 4.5 weeks, p = 0.04). The average birthweight of the hypertensive group was significantly higher than the control group (2574.3 ± 1029.2 grams vs 2278.5 ± 989 grams, p = 0.002). Table 2 illustrates the percentage of BP recordings >95th percentile for the AWAKEN cohort. Definite hypertension was found in 38/2162 (1.8%) with 24 having a discharge diagnosis of hypertension, 10 were discharged home on antihypertensive medication and 4 had a discharge diagnosis of hypertension and were discharged home on antihypertensives. Undiagnosed hypertension was found in 81/2172 (3.7%), thus, the overall incidence of diagnosed and undiagnosed hypertension was 5.5%. The rates of hypertension by gestational age category are listed in Table 3. Being of Caucasian race, outborn, vaginal delivery, hyperbilirubinaemia, and congenital heart disease were significant risk factors for the development of hypertension for the whole AWAKEN cohort. Factors associated with reduced risk of neonatal hypertension were small for gestational age, multiple gestations, and steroids for fetal maturation (Table 4). In comparison to those without hypertension the length of stay for the entire cohort was increased for the combined grouping of hypertension and undiagnosed hypertension (30.4 ± 33.6 vs 36.8 ± 38.9; p = 0.049).
Acute kidney injury
The overall incidence of AKI in the cohort was 29.9%. The incidence of AKI was significantly higher in the hypertensive group in comparison to the control group (41.2% vs 26.2%, p < 0.0001). Even after adjusting for other variables associated with hypertension (overall AKI, Race, gestational age, birth weight, delivery site, mode of delivery, admission for Respiratory Symptoms or Failure, admission for hyperbilirubinemia, admission for congenital heart disease, small for gestational age, multiple gestation, and maternal steroids for fetal maturation), neonates with AKI were nearly twice as likely to develop hypertension (adjusted OR = 2.1 (1.4–3.1), p = 0.004), (Table 5). Table 6 depicts the relationship between presence or absence of hypertension with AKI type (urine output vs serum creatinine vs both) and stage 1–3 stratified by gestational age category.
Demographics for infants ≤29 weeks gestation
Over 5% (15/276) of neonates born ≤29 weeks gestation had hypertension. Of these 15, 11 were diagnosed with definite hypertension and 4 were defined as having undiagnosed hypertension. The incidence of definite hypertension and undiagnosed hypertension in this gestational age group was 4.0% and 1.4%, respectively (Table 3). Definite intrapartum bacterial infection was a significant risk factor for hypertension in this gestational age group (Table 4). In the hypertensive and control groups the rate of AKI was 40% and 42.9% (Table 4). There was no relationship between stage of AKI and a diagnosis of hypertension (Table 6). There was no difference length of stay between those without and those with hypertension (79.7 ± 44.5 vs 101 ± 29.5; p = 0.07).
Demographics for infants 30–35 weeks gestation
Nearly 4% (37/958) of neonates born between 30 and 35 weeks gestation were diagnosed with hypertension. Of these 37, 6 were diagnosed with definite hypertension and 31 were defined as having undiagnosed hypertension. The incidence of definite hypertension and undiagnosed hypertension in this gestational age group was 0.6% and 3.2%, respectively (Table 3). Being of Caucasian race, heavier birthweight, outborn, vaginal delivery and hyperbilirubinaemia were all significant risk factors for the development of hypertension in this gestational age group (Table 4). In the hypertensive and control groups the rate of AKI was 29.7% and 16.4% (Table 4). There was an increased risk of hypertension with Stage 1 AKI (Table 6). There was no difference in length of stay between those without and those with hypertension (29.2 ± 27.6 vs 31.9 ± 23.7; p = 0.55).
Demographics for infants ≥36 weeks gestation
Over 7% (67/928) of neonates born ≥36 weeks gestation were diagnosed with hypertension. Of these 67, 21 were diagnosed with definite hypertension and 46 were defined as having undiagnosed hypertension. The incidence of definite hypertension and undiagnosed hypertension in this gestational age group was 2.3% and 5.0%, respectively (Table 3). Oligohydramnios, outborn, vaginal delivery, and hyperbilirubinaemia were all significant risk factors for the development of hypertension in this gestational age group (Table 4). In the hypertensive and control groups the rate of AKI was 47.8% and 31.7% (Table 4). There was an increased risk of hypertension with Stage 2 and 3 AKI (Table 6). In comparison to those without hypertension the length of stay was increased for the combined grouping of hypertension and undiagnosed hypertension (16.9 ± 18.7 vs 25.0 ± 33.6; p = 0.001).
For neonates that were classified as having undiagnosed hypertension, all three measurements (systolic, diastolic and mean) were significantly higher than those without hypertension or those that had been diagnosed with hypertension (Fig. 2a–c and Table 7). It is likely that there was no difference in the measurements between those without hypertension and those diagnosed with hypertension due to treatment.
Analyses showing differences between all three BP measurements on each day recorded between those with no hypertension, hypertension and undiagnosed (calculated) hypertension. a Systolic blood pressure measurements for each day recorded for each of the three groups—no hypertension, hypertension, and undiagnosed (calculated) hypertension. b Diastolic blood pressure measurements for each day recorded for each of the three groups—no hypertension, hypertension, and undiagnosed (calculated) hypertension. c Mean blood pressure measurements for each day recorded for each of the three groups—no hypertension, hypertension, and undiagnosed (calculated) hypertension
Discussion
This study is the first to evaluate the incidence of neonatal hypertension and that of undiagnosed hypertension in a large, multicenter setting. The incidence of hypertension in previous studies has been reported in up to 3% of all neonates admitted to the NICU.2,3,6,7,8,9 In the AWAKEN cohort 1.8% of neonates were diagnosed with definite hypertension, however, an additional 3.7% of neonates were defined as having undiagnosed hypertension. The incidence of definite hypertension was greatest in the ≤29 week gestational age group, which may be accounted for by the closer monitoring that occurs in the most premature infants. The incidence of undiagnosed hypertension increased with gestational age, indicating a potential lack of monitoring in older pre-term and term infants. Thus, this data supports our first hypothesis that many neonates with hypertension remain undiagnosed.
The diagnosis of neonatal hypertension is important to ensure adequate treatment, to prevent the possible complications of cardiac and renal compromise, and to identify the risk of cardiovascular disease later in life.4 The concept of early life physiological programming hypothesizes an association between prenatal environmental events, altered fetal growth and development, and later cardiovascular complications.26 Therefore, elevated hypertension during the neonatal period may affect the development and organization of specific tissues, thus producing effects that persist into adulthood. Neonates that have undiagnosed hypertension may be more vulnerable to these complications later in life. Due to the limited data regarding follow-up of infants with neonatal hypertension more information is required regarding the potential cardiovascular and renal risk in adolescence and adulthood.
Relationship between AKI and neonatal hypertension
The second hypothesis was confirmed by the results achieved in this study, whereby AKI was found to be a risk factor for the development of hypertension for the whole AWAKEN cohort. For those neonates diagnosed with an AKI, they were nearly two times more likely to develop neonatal hypertension, even after adjusting for other risk factors for hypertension. This result highlights the requirement for regular BP monitoring of those neonates with a diagnosis of AKI in the NICU.
Although there have not been any large, multicenter studies in neonates investigating the relationship between AKI and neonatal hypertension, Hsu et.al found that in an adult population AKI was independently associated with a 22% increase in the odds of developing elevated BP, with higher adjusted odds with more severe AKI.27 Their results extend previous findings in children regarding the risk of hypertension after various forms of acute renal disease.28,29
AKI results in parenchymal renal damage and the formation of inflammatory mediators that abolish the renal autoregulation mechanisms; myogenic and tubuloglomerular feedback. Renin is secreted in response to a decrease in arterial BP, detected by baroreceptors and reduced renal blood flow. Secretion of renin results in the production of angiotensin II, which constricts the small arterioles throughout the body therefore increasing BP and activating aldosterone. Aldosterone acts on distal tubules and collecting ducts of the nephron resulting in the conservation of sodium, thereby indirectly influencing water retention, blood volume and BP.30 These effects are seen in neonates with AKI with reduced urine output which can result in fluid overload and potentially subsequent hypertension. The long-term effects of AKI in neonates in respect to ongoing hypertension and risk of chronic disease in adulthood is unknown.
Comparison of risk factors between gestational age groups
During the intrauterine period, the cardiovascular system undergoes both structural and functional maturation and, therefore, gestational age is expected to play a role in determining BP.18 Furthermore, the risk factors that may contribute to an elevation in BP may vary between gestational age groups.
This is the first study to identify hyperbilirubinaemia as a risk factor for neonatal hypertension. It is unclear whether increased bilirubin levels elevate BP independently or are a marker of activation of the heme oxygenase-1 enzyme.
Heme oxygenase (HO) enzymes catabolise heme released from the breakdown of red blood cells to carbon monoxide and biliverdin, which is subsequently converted to bilirubin by biliverdin reductase.31 Two major isoforms of heme oxygenase have been identified, an inducible enzyme (HO-1) and a constitutive isoform (HO-2). HO-1 is a microsomal enzyme whose benefits are mediated by its by-products, which exert potent anti-inflammatory, anti-oxidant, and anti-proliferative effects. The induction of HO-1 is an adaptive and beneficial response following ischemia-hypoperfusion, rhabdomyolysis, and nephron-toxin-induced models of AKI. Although bilirubin is a part of this pathway, it is unclear whether it has protective effects or is a by-product.
A rodent model of severe hyperbilirubinaemia due to loss of hepatic UGT1A1, is resistant to vascular remodeling following a challenge with angiotensin II.31 Moderate hyperbilirubinaemia has also been found to preserve renal blood flow and normalize renal vascular resistance in angiotensin II treated mice. Ren et.al and Wang et.al have demonstrated an important role for bilirubin in protecting against excessive TGF-mediated constriction of the afferent arteriole; however, the exact mechanism by which this occurs is unknown.31 Elevated bilirubin levels also result in the quenching of reactive oxygen species, such as superoxide, thereby protecting renal vasculature.31 The results from this study support the above theory, and may suggest that heme oxygenase has a role in BP control. Further studies are required to investigate the underlying mechanisms and confirm the influence of bilirubin on BP.
In the 30–35 week and ≥36 week gestational age groups, vaginal delivery was found to be a risk factor for neonatal hypertension. A study by Sullivan et.al found that those delivered by cesarean section had lower BP.32 However, these findings have not been supported by Uhari, making the role of mode of delivery in neonatal hypertension unclear.33 The data on mode of delivery and BP in the first day of life and subsequent neonatal hypertension is very limited. There are many factors that have not been investigated in these studies including epidurals, types of anesthesia etc and how long this influence persists. The definition of hypertension is also rarely made in the first few days of life, where the influence of delivery has been noted to influence BP in normal neonates. The definition of hypertension must take into account gestation at birth and current postmenstrual age, but mode of delivery would not be a major factor to be considered in the diagnosis unless further information becomes available. Being of Caucasian race was also found to be a risk factor for the development of hypertension, contrary to a study by Vohr et.al.34 These differences may be explained by the sample studied and although our study sampled from multiple countries, the majority of neonates enrolled were classified as Caucasian.
Protective factors identified for the whole AWAKEN cohort were small for gestational age, multiple gestation, and antenatal steroids. Studies investigating the impact of birthweight on BP in early life have suggested a direct relationship, and Launer et.al showed that the direction of this relation between BP and birthweight reverses at 3 months of age.35 Our findings were similar to the study by Pejovic et.al, which showed that BP was higher in neonates with higher birth weights.36 Antenatal corticosteroids have become a mainstay of treatment in women at risk of pre-term delivery. Although our study found corticosteroids to be a protective factor, there is no clear consensus in the literature surrounding this topic.18,37 Multiple gestation neonates are often delivered electively at earlier gestations due to chorionicity and discrepant growth but are otherwise well, which may be protective against the other complications of prematurity.
Similar to our study, a previous study by Kent et.al included maternal and pregnancy-associated disease states allowing the investigation of their effects on neonatal hypertension.38 Exclusion of neonates with congenital and chromosomal abnormalities prevents the analysis of neonatal hypertension in this high-risk population, potentially reducing the incidence.11,19 Unique to previous studies, we examined the incidence of definite and undiagnosed neonatal hypertension and risk factors for neonatal hypertension according to gestational age group. Previous studies have examined the incidence of neonatal hypertension according to birthweight categories, and it is not clear whether this is a better predictor for risk of developing hypertension.34,39
Despite the strengths of the study which include: large cohort size and contribution from twenty-four NICUs across the globe, we acknowledge the following limitations: (1) the small cohort for the ≤29 week gestational group, which may have had an influence on the significance of the results noted in comparison to the other gestational age groups. (2) The AWAKEN study did not document BP measurement technique, the extremity used, or level of activity during BP measurement in the twenty-four centers involved in the study, thus certainty of measurement is not definite. BP measurement in neonates requires careful attention to how and under what circumstances the measurements are taken. Invasive BP measurements are considered the gold standard; however, it can be affected by arterial spasm and incorrect placement of the transducer above or below the level of the heart. Non-invasive BP measurement is more commonly performed as invasive methods are time limited. Three BP measurements should be taken using an appropriate sized cuff, on an upper limb, with the neonate in a resting awake state. The type of measurement along with whether neonates were sedated, on inotropes or fluid overloaded was not collected in this study and is required for future prospective studies evaluating neonatal BP and hypertension. (3) We used an arbitrary, yet conservative cut-off point of the 95th percentile and the infant had to have more than 50% of the lowest BP measurements obtained on the particular day to define undiagnosed hypertension. A cut-off point of the 95th percentile is similar to previous studies examining the incidence of neonatal hypertension; therefore, these results are potentially comparable. Whether this is the most accurate way of defining hypertension in neonates is still uncertain. We acknowledge potential bias in the ascertainment of AKI, as many infants may not have had serum creatinine and/or urine output quantified during a potential AKI event, thus the true incidence of AKI may have been higher.
The results from this study suggest that neonatal hypertension is a potentially under-recognized condition seen in NICU graduates, who have required some degree of intervention for a heterogeneous group of illnesses. A clear definition and up-to-date normotensive data is required for future appropriate diagnosis and understanding of neonatal hypertension.10 Emphasis should also be placed on closer monitoring of BP in neonates, especially those with AKI and other risk factors. Furthermore, the results from this study may suggest that heme oxygenase has a role in BP control, however further studies are required to investigate the underlying mechanisms and confirm the role of bilirubin in neonatal hypertension. More studies are also required to identify which risk factors are of concern in the diagnosis of neonatal hypertension according to gestational age.
Conclusion
This is the first large, multicenter study to determine the incidence of neonatal hypertension and potentially undiagnosed hypertension following admission to a neonatal intensive care unit. The incidence of definite hypertension in the AWAKEN cohort is similar to previous studies, however the incidence of undiagnosed neonatal hypertension highlights the need for up-to-date normative data and guidelines and regular BP monitoring in neonates. Considering this is the first study to examine the incidence of undiagnosed hypertension further studies are required to validate these findings. This is also the first study to identify AKI and hyperbilirubinaemia as risk factors for neonatal hypertension. Further studies are required to identify the significance of these risk factors and long-term outcomes in adulthood.
Change history
08 August 2018
Text for Correction
References
Chaudhari, T. et al. Neonatal hypertension—a long-term pilot follow-up study. Res. Rep. Neonatol. 3, 37–43 (2013).
Flynn, J. T. Neonatal hypertension: diagnosis and management. Pediatr. Nephrol. 14, 332–341 (2000).
Flynn, J. T. Hypertension in the neonatal period. Curr. Opin. Pediatr. 24, 197–204 (2012).
Seliem, W. A., Falk, M. C., Shadbolt, B. & Kent, A. L. Antenatal and postnatal risk factors for neonatal hypertension and infant follow-up. Pediatr. Nephrol. 22, 2081–2087 (2007).
Carey, B. E. Neonatal systemic hypertension. Newborn. Infant. Nurs. Rev. 2, 105–110 (2002).
Batisky, D. L. Neonatal hypertension. Clin. Perinatol. 41, 529–542 (2014).
Dionne, J. M., Abitbol, C. L. & Flynn, J. T. Hypertension in infancy: diagnosis, management and outcome. Pediatr. Nephrol. 27, 17–32 (2012).
Watkinson, M. Hypertension in the newborn baby. Arch. Dis. Child Fetal Neonatal Ed. 86, F78–F88 (2002).
Sahu, R. et al. Systemic hypertension requiring treatment in the neonatal intensive care unit. J. Pediatr. 163, 84–88 (2013).
Sharma, D., Pandita, A. & Shastri, S. Neonatal hypertension: an undiagnosed condition, a review article. Curr. Hypertens. Rev. 10, 1–8 (2014).
Georgieff, M. K., Mills, M. M., Gomez-Marin, O. & Sinaiko, A. R. Rate of change of blood pressure in premature and full term infants from birth to 4 months. Pediatr. Nephrol. 10, 152–155 (1996).
Kent, A. L., Kecskes, Z., Shadbolt, B. & Falk, M. C. Blood pressure in the first year of life in healthy infants born at term. Pediatr. Nephrol. 22, 1743–1749 (2007).
Blowey, D. L., Duda, P. J., Stokes, P. & Hall, M. Incidence and treatment of hypertension in the neonatal intensive care unit. J. Am. Soc. Hypertens. 5, 478–483 (2011).
Zubrow, A. B. et al. Determinants of blood pressure in infants admitted to neonatal intensive care units: a prospective multicentre study. J. Perinatol. 15, 470–479 (1995).
Adelman, R. D. Neonatal hypertension. Pediatr. Clin. North. Am. 25, 99–110 (1978).
Jetton, J. G. et al. Assessment of worldwide acute kidney injury epidemiology in neonates: design of a retrospective cohort study. Front. Pediatr. 4, 1–11 (2016).
Jetton J. G., et al. Neonatal acute kidney injury incidence and outcomes: Findings from the multi-center, multi-national Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates (AWAKEN) observational cohort study. Lancet Child Adoles. Health 1, 184–194 (2017).
Kent, A. L. & Chaudhari, T. Determinants of neonatal blood pressure. Curr. Hypertens. Rep. 15, 426–432 (2013).
Engle, W. D. Blood pressure in the very low birth weight neonate. Early Hum. Dev. 62, 97–130 (2001).
Cantinotti, M. et al. Strengths and limitations of current pediatric blood pressure nomograms: a global overview with a special emphasis on regional differences in neonates and infants. Hypertens. Res. 38, 577–587 (2015).
Kent, A. L., Kecskes, Z., Shadbolt, B. & Falk, M. C. Normative blood pressure data in the early neonatal period. Pediatr. Nephrol. 22, 1335–1341 (2007).
Task Force on Blood Pressure Control in Children. Report of the second task force on blood pressure control in children—1987. Pediatrics 79, 1–25 (1987).
Fanaroff, J. M. & Fanaroff, A. A. Blood pressure disorders in the neonate: hypotension and hypertension. Semin. Fetal Neonatal Med. 11, 174–181 (2006).
Jetton, J. G. & Askenazi, D. J. Update on acute kidney injury in the neonate. Curr. Opin. Pediatr. 24, 191–196 (2012).
Zappitelli, M. et al. Developing a neonatal acute kidney injury research definition: a report from the NIDDK neonatal AKI workshop. Pediatr. Res. 82, 569–573 (2017).
Seckl, J. R. Physiologic programming of the fetus. Clin. Perinatol. 25, 939–964 (1998).
Hsu, C. Y. et al. Elevated BP after AKI. JASN 27, 914–923 (2016).
Askenazi, D. J. et al. 3–5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int. 69, 184–189 (2006).
Vivante, A. et al. Childhood history of resolved glomerular disease and risk of hypertension during adulthood. JAMA 311, 1155–1157 (2014).
Guyton, A. C. Blood pressure control—special role of the kidneys and body fluids. Science 252, 1813–1816 (1991).
Stec, D. E., Hosick, P. A. & Granger, J. P. Bilirubin, renal hemodynamics, and blood pressure. Front. Pharmacol. 3, 1–7 (2012).
O’Sullivan, M. J., Kearney, P. J. & Crowley, M. J. The influence of some perinatal variables on neonatal blood pressure. Acta Pediatr. 85, 849–853 (1996).
Uhari, M. Changes in blood pressure during the first year of life. Acta Pediatr. Scand. 69, 613–617 (1980).
Vohr, B. R. et al. Early predictors of hypertension in prematurely born adolescents. Acta Pediatr. 99, 1812–1818 (2010).
Launer, L. J., Hofman, A. & Grobbee, D. E. Relation between birth weight and blood pressure: longitudinal study of infants and children. BMJ 307, 1451–1454 (1993).
Pejkovic, B., Peco-Antic, A. & Marinkovic-Eric, J. Blood pressure in non-critically ill preterm and full-term neonates. Pediatr. Nephrol. 22, 249–257 (2007).
LeFlore, J. L., Engle, W. D. & Rosenfeld, C. R. Determinants of blood pressure in very low birth weight neonates: lack of effect of antenatal steroids. Early Hum. Dev. 59, 37–50 (2000).
Kent, A. L. et al. Do maternal- or pregnancy-associated disease states affect blood pressure in the early neonatal period? Aust. N. Z. J. Obstet. Gynaecol. 49, 364–370 (2009).
Lurbe, E. et al. First-year blood pressure increase steepest in low birthweight newborns. J. Hypertens. 25, 81–86 (2007).
Acknowledgements
The authors would also like to thank the outstanding work of the following clinical research personnel and colleagues for their involvement in AWAKEN: Ariana Aimani, Samantha Kronish, Ana Palijan, MD, Michael Pizzi—Montreal Children’s Hospital, McGill University Health Centre, Montreal, Quebec, Canada; Laila Ajour, BS, Julia Wrona, BS—University of Colorado, Children’s Hospital Colorado, Aurora, Colorado, USA; Melissa Bowman, RN—University of Rochester, Rochester, New York, USA; Teresa Cano, RN, Marta G. Galarza, MD, Wendy Glaberson, MD, Aura Arenas Morales, MD, Denisse Cristina Pareja Valarezo, MD—Holtz Children’s Hospital, University of Miami, Miami, Florida, USA; Sarah Cashman, BS, Madeleine Stead, BS—University of Iowa Children’s Hospital, Iowa City, Iowa, USA; Jonathan Davis, MD, Julie Nicoletta, MD—Floating Hospital for Children at Tufts Medical Center, Tufts University School of Medicine, Boston, Massachusetts, USA; Alanna DeMello—British Columbia Children’s Hospital, Vancouver, British Columbia, Canada; Lynn Dill, RN—University of Alabama at Birmingham, Birmingham, Alabama, USA; Emma Perez-Costas PhD—university of Alabama at Birmingham, Birmingham, Alabama, USA; Ellen Guthrie, RN—MetroHealth Medical Center, Case Western Reserve University, Cleveland, Ohio, USA, Nicholas L. Harris, BS, Susan M. Hieber, MSQM—C.S. Mott Children’s Hospital, University of Michigan, Ann Arbor, Michigan, USA; Katherine Huang, Rosa Waters—University of Virginia Children’s Hospital, Charlottesville, Virginia, USA; Judd Jacobs, Ryan Knox, BS, Hilary Pitner, MS, Tara Terrell—Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA; Nilima Jawale, MD—Maimonides Medical Center, Brooklyn, New York, USA; Emily Kane—Australian National University, Canberra, Australia; Vijay Kher, DM, Puneet Sodhi, MBBS—Medanta Kidney Institute, The Medicity Hospital, Gurgaon, Haryana, India; Grace Mele—New York College of Osteopathic Medicine, Westbury, New York, USA; Patricia Mele, DNP—Stony Brook Children’s Hospital, Stony Brook, New York, USA; Charity Njoku, Tennille Paulsen, Sadia Zubair—Texas Children’s Hospital, Baylor College of Medicine, Houston, Texas, USA; Emily Pao—University of Washington, Seattle Children’s Hospital, Seattle, Washington, USA; Becky Selman RN, Michele Spear, CCRC—University of New Mexico Health Sciences Center Albuquerque, New Mexico, USA; Melissa Vega, PA-C—The Children’s Hospital at Montefiore, Bronx, New York, USA); and Leslie Walther RN—Washington University, St. Louis, Missouri, USA.
NKC Contributors
David T. Selewski5, MD, Subrata Sarkar5, MD, Alison Kent6, MD, Jeffery Fletcher6, PhD, Carolyn L Abitbol7, MD, Marissa DeFreitas7, MD, Shahnaz Duara, MD, Jennifer R. Charlton8, MD, Jonathon Swanson8, MD, Ronnie Guillet9, MD, Carl D’Angio9, MD, Ayesa Mian9, MD, Erin Rademacher9, MD, Maroun J. Mhanna10, MD, Rupesh Raina10, MD, Deepak Kumar10, MD, Namasivayam Ambalavanan11, MD, Ayse Akcan Arikan12, MD, Christopher J. Rhee12, MD, Stuart L. Goldstein13, MD, Amy T. Nathan13, MD, Alok Bhutada14, MD, Shantanu Rastogi14, MD, Elizabeth Bonachea15, MD, Susan Ingraham15, MD, John Mahan15, MD; Arwa Nada15, MBBCH, Patrick D.16 Brophy, MD, Tarah T. Colaizy16, MD, Jonathan M. Klein16, MD, F. Sessions Cole17, MD, T. Keefe Davis17, MD, Joshua Dower18, BS, Lawrence Milner18, MD, Alexandra Smith18, MD Mamta Fuloria19, MD, Kimberly Reidy19, MD, Frederick J. Kaskel19, MD, Jason Gien20, MD, Katja M. Gist20, DO, Mina H. Hanna21, MD, Sangeeta Hingorani22, MD, Michelle Starr22, MD, Catherine Joseph23, MD, Tara DuPont23, MD, Robin Ohls23, MD, Amy Staples23, MD, Surender Khokhar24, MD, Sofia Perazzo25, MD, Patricio E. Ray25, Mary Revenis25, MD, Anne Synnes26, MDCM, Pia Wintermark27, MD, and Michael Zappitelli27, MD
Funding
Cincinnati Children’s Hospital Center for Acute Care Nephrology provided funding to create and maintain the AWAKEN Medidata Rave electronic database. The Pediatric and Infant Center for Acute Nephrology (PICAN) provided support for web meetings for the NKC steering committee annual meeting at the University of Alabama at Birmingham (UAB), as well as support for some of the AWAKEN investigators at UAB (LBJ, RJG). PICAN is part of the Department of Pediatrics at the University of Alabama at Birmingham (UAB), and is funded by Children’s of Alabama Hospital, the Department of Pediatrics, UAB School of Medicine, and UAB’s Center for Clinical and Translational Sciences (CCTS, NIH grant UL1TR001417). Finally, the AWAKEN study at the University of New Mexico was supported by the Clinical and Translational Science Center (CTSC, NIH grant UL1TR001449) and by the University of Iowa Institute for Clinical and Translational Science (U54TR001356).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The following individuals served as collaborators and site investigators for the AWAKEN study. They collaborated in protocol development and review, local IRB submission, data collection, and participated in drafting or review of the manuscript:
Rights and permissions
About this article
Cite this article
Kraut, E., Boohaker, L., Askenazi, D. et al. Incidence of neonatal hypertension from a large multicenter study [Assessment of Worldwide Acute Kidney Injury Epidemiology in Neonates—AWAKEN]. Pediatr Res 84, 279–289 (2018). https://doi.org/10.1038/s41390-018-0018-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0018-8
This article is cited by
-
A reappraisal of risk factors for hypertension after pediatric acute kidney injury
Pediatric Nephrology (2024)
-
Blood pressure in preterm infants with bronchopulmonary dysplasia in the first three months of life
Pediatric Nephrology (2024)
-
Recurrent acute kidney injury in preterm neonates is common and associated with worse outcomes and higher mortality
Pediatric Research (2022)
-
Postnatal glucocorticoid use impacts renal function in VLBW neonates
Pediatric Research (2022)
-
Antenatal and perinatal factors influencing neonatal blood pressure: a systematic review
Journal of Perinatology (2021)