Abstract
Background/Objectives
Oropharyngeal dysphagia (OD) is a common problem in elderly population that negatively affects the oral intake and body composition resulting in clinical complications as malnutrition and dehydration. The aim of this study was to design, implement, and evaluate the effect of texture-modified foods and thickened drinks diet, with nectar or pudding viscosity and controlled bolus volume in older adults with OD on body composition and oral intake.
Subjects/Methods
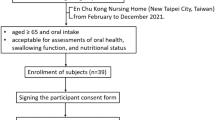
Randomized clinical trial, simple blind. Patients ≥ 65 years, admitted at a national institute, who had a confirmed diagnosis of OD were included. A texture-modified foods and thickened drinks diet, with nectar or pudding viscosity and controlled bolus volume, was compared to isocaloric standard treatment for 12 weeks. Body composition was evaluated by bioelectrical impedance, muscular functionality was evaluated by handgrip strength, and daily energy and protein intake by 24-h recall and evaluated by Food Processor Nutrition Analysis® software.
Results
Twenty participants were included per group, with mean age 76 years. After 12 weeks, the consumption of energy (29 ± 10 to 40 ± 15 kcal/kg, p = 0.009) and protein (1.3 ± 0.6 to 1.8 ± 0.7 g/kg, p = 0.03), as well as phase angle (4.4 ± 1.8 to 5.5 ± 2.5°, p = 0.05), body weight (56 ± 10 to 60 ± 10 kg, p < 0.001), and handgrip strength (18 ± 11 to 21 ± 13 kg, p = 0.004) increased in the intervention group. In control group there were no changes.
Conclusions
The dietary intervention improved oral intake, weight, handgrip strength, and phase angle, which can prevent or limit the nutritional complications associated with the OD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Clavé P, Shaker R. Dysphagia: current reality and scope of the problem. Nat Rev Gastroenterol Hepatol. 2015;49:1–12.
Roden DF, Altman KW. Causes of dysphagia among different age groups. A systematic review of the literature. Otolaryngol Clin North Am. 2013;46:965–87.
Clave P, Verdaguer A, Arreola V. Oral-pharyngeal dysphagia in the elderly. Med Clin. 2005;124:742–8.
Carrión S, Cabré M, Monteis R, Roca M, Palomera E, Serra-Prat M, et al. Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin Nutr. 2015;34:436–42.
Rofes L, Arreola V, Almirall J, Cabré M, Campins L, García-Perris P, et al. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract 2011;2011:818–979..
Loeb MB, Becker M, Eady A, Walker-Dilks C. Interventions to prevent aspiration pneumonia in older adults: a systematic review. J Am Geriatr Soc. 2003;51:1018–22.
Almirall J, Cabre M, Clave P. Aspiration pneumonia. Med Clin. 2007;129:424–32.
Germain I, Dufresne T, Gray-Donald K. A novel dysphagia diet improves the nutrient intake of institutionalized elders. J Am Diet Assoc. 2006;106:1614–23.
Higashiguchi T. Novel diet for patients with impaired mastication evaluated by consumption rate, nutrition intake, and questionnaire. Nutrition. 2013;29:858–64.
Taylor KA, Barr SI. Provision of small, frequent meal does not improve energy intake of elderly residents with dysphagia, who live in extended care facility. J Am Diet Assoc. 2006;106:1115–8.
Barrea L, Muscogiuri G, Macchia PE, Di Somma C, Falco A, Savanelli MC, et al. Mediterranean diet and phase angle in a sample of adult population: results of a pilot study. Nutrients. 2017;9:1–14.
Barrea L, Muscogiuri G, Di Somma C, Tramontano G, De Luca V, Illario M, et al. Association between Mediterranean diet and hand grip strength in older adult women. Clin Nutr 2018 Apr 3;S0261-5614(18):1-9.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919–24.
Burgos R, Sarto B, Segurola H, Romagosa A, Puiggrós C, Vázquez C, et al. Translation and validation of the Spanish version of the EAT-10 (Eating Assessment Tool-10) for the screening of dysphagia. Nutr Hosp. 2012;27:2048–54.
Clavé P, Arreola V, Romea L, Medina L, Palomera E, Serra-Prat M, et al. Accuracy of volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr. 2008;27:806–15.
Dawson B, Trapp R. Basic & clinical biostatistics. 4th ed. New York: Lange Medical Books-McGraw-Hill, Medical Pub. Division; 2004.
Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics Books Bridged Edition; 1991.
Christensson L, Unosson M, Ek AC. Evaluation of nutritional assessment techniques in elderly people newly admitted to municipal care. Eur J Clin Nutr. 2002;56:810–8.
Guigoz Y, Vellas B, Garry PJ. Mini Nutritional Assessment: a practical assessment tool for grading the nutritional state of elderly patients. Facts Res Gerontol. 1994;4(Suppl 2):15–59.
Kyle UG, Bosaeus I, de Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, et al. Bioelectrical impedance analysis—part II: utilization in clinical practice. Clin Nutr. 2004;23:1430–53.
Kushner RF. Bioelectrical impedance analysis: a review of principles and applications. J Am Coll Nutr. 1992;11:199–209.
McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically Ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enter Nutr. 2016;40:159–211.
Bauer J, Biolo G, Cederholm T, Cesari M, Cruz-Jentoft AJ, Morley JE, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. 2013;14:542–59.
American Dietetic Association and National Dysphagia Diet Task Force. National dysphagia diet: standardization for optimal care. 1st ed. Chicago, IL: American Dietetic Association; 2002.
Andersen UT, Beck AM, Kjaersgaard A, Hansen T, Poulsen I. Systematic review and evidence based recommendations on texture modified foods and thickened fluids for adults with oropharyngeal dysphagia. ESPEN J. 2013;8:e127–34.
Hanson B. A review of diet standardization and bolus rheology in the management of dysphagia. Curr Opin Otolaryngol Head Neck Surg. 2016;24:183–90.
Mertz-Garcia J, Chambers E. Perspectives of registered dietitians about thickened beverages in nutrition management of dysphagia. Top Clin Nutr. 2012;27:105–13.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–23.
Barbosa-Silva MC, Barros A, Wang J, Heymsfield SB, Pierson RN Jr, et al. Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Am J Clin Nutr. 2005;82:49–52.
Kuroda Y. Relationship between swallowing function and functional and nutritional status in hospitalized elderly individuals. Int J Speech Lang Pathol Audiol. 2014;2:20–6.
Walshe M. Oropharyngeal dysphagia in neurodegenerative disease. J Gastroenterol Hepatol Res. 2014;3:1265–71.
Schiffman SS, Zervakis J. Taste and smell perception in the elderly: effect of medications and disease. Adv Food Nutr Res. 2002;44:247–346.
Shah M, Deeb J, Fernando M, Noyce A, Visentin E, Findley LJ, et al. Abnormality of taste and smell in Parkinson’s disease. Park Relat Disord. 2009;19:232–7.
Keller H, Chambers L, Niezgoda H. Issues associated with the use of modified texture foods. J Nutr Health Aging. 2012;16:195–200.
Acknowledgements
The authors thank clinical nutrition service members as well as the nursing and medical staff for providing valuable assistance.
Funding
The National Council of Science and Technology (CONACYT) provided a graduate scholarship for the principal investigator. Victus® laboratory donated the Enterex Food Thickener for the intervention in the study. The CONACYT and Victus® laboratory took no part in design, conduct of the study, collection, management, analysis, interpretation of the data, preparation, review, and approval of the manuscript.
Author contributions
AES-Z, LC-M, C-N, RR-T: study concept and design. AGR-V, RR-G, MZ-S: clinical diagnoses and data collection. LC-M and CAR-T: analysis and interpretation of data. CAR-T and AGR-V: drafting of the manuscript. AES-Z, LC-M: critical revision of the manuscript. All authors have reviewed the manuscript and approved its submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reyes-Torres, C.A., Castillo-Martínez, L., Reyes-Guerrero, R. et al. Design and implementation of modified-texture diet in older adults with oropharyngeal dysphagia: a randomized controlled trial. Eur J Clin Nutr 73, 989–996 (2019). https://doi.org/10.1038/s41430-019-0389-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-019-0389-x
This article is cited by
-
Effects of hydrolysed meat on dietary intake and nutritional status in aged care residents requiring pureed diets: a crossover randomised controlled trial
BMC Geriatrics (2022)
-
Prevalence and management of dysphagia in nursing home residents in Europe and Israel: the SHELTER Project
BMC Geriatrics (2022)
-
Association between food texture levels consumed and the prevalence of malnutrition and sarcopenia in older patients after stroke
European Journal of Clinical Nutrition (2022)
-
Impact of Multiple Texture-Modified Diets on Oral Intake and Nutritional Status in Older Patients with Pneumonia: A Retrospective Cohort Study
Dysphagia (2020)
-
Burden of Premorbid Consumption of Texture Modified Diets in Daily Life on Nutritional Status and Outcomes of Hospitalization
The Journal of nutrition, health and aging (2019)