Abstract
The aim of this study was to investigate whether treatment with diminazene aceturate (DIZE), a putative ACE2 activator, or with angiotensin-(1–7) during pregnancy could attenuate the development of cardiovascular dysfunction in the adult offspring of spontaneously hypertensive rats (SHRs). For this, pregnant SHRs received DIZE or Ang-(1–7) throughout gestation. The systolic blood pressure (SBP) was measured in the male offspring from the 6th to16th weeks of age by tail-cuff plethysmography. Thereafter, the left ventricular contractile function and coronary reactivity were evaluated by the Langendorff technique. Samples of the left ventricles (LVs) and kidneys were collected for histology and western blot assay in another batch of adult rat offspring. Maternal treatment with DIZE or Ang-(1–7) during pregnancy attenuated the increase in SBP in adult offspring. In addition, both DIZE and Ang-(1–7) treatments reduced the cardiomyocyte diameter and fibrosis deposition in the LV, and treatment with Ang-(1–7) also reduced the fibrosis deposition in the kidneys. Maternal treatment with DIZE, as well as Ang-(1–7), improved the coronary vasodilation induced by bradykinin in isolated hearts from adult offspring. However, no difference was observed in the contractile function of the LVs of these animals. The expression levels of AT1 and Mas receptors, ACE, ACE2, SOD, and catalase in the LV were not modified by maternal treatment with Ang-(1–7), but this treatment elicited a reduction in AT2 expression. These data show that treatment with DIZE or Ang-(1–7) during gestation promoted beneficial effects of attenuating hypertension and cardiac remodeling in adult offspring.
Similar content being viewed by others
Introduction
Cardiovascular diseases (CVDs) affect many people all around the world and are the leading cause of death [1]. Hypertension, characterized by a sustained increase in blood pressure, presents an important risk factor for the development of other pathologies of the cardiovascular system, such as myocardial infarction and heart failure [2]. Some factors, such as family history, sedentary lifestyle, unbalanced diet, stress, and high sodium intake, among others, contribute to the development of CVDs, including hypertension [3].
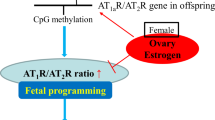
It has been proven that harmful stimuli during gestation can promote deleterious outcomes in offspring [4, 5]. Maternal exposure to a high-fat diet [6], hypoxia [7], smoking [8], dehydration [9], or protein restriction [10] led to the development of hypertension in the offspring. Furthermore, previous studies have observed that the renin-angiotensin system (RAS) can play a role in this pathological process [11,12,13,14]. A high sucrose intake during gestation promoted changes in vascular reactivity associated with increased protein expression of the AT1 receptor in the aorta and mesenteric arteries of the offspring [13]. Mothers submitted to a low-protein diet during pregnancy had offspring with an increase in blood pressure and increased urinary excretion of Ang II [10, 15]. Moreover, treatments with the angiotensin-converting enzyme (ACE) inhibitor or AT1 receptor antagonist were able to reverse the increased blood pressure in the offspring of protein-restricted rats during pregnancy [16].
Interestingly, recent studies have shown that the use of beneficial therapies during pregnancy resulted in beneficial responses in the offspring [17, 18]. Maternal supplementation with resveratrol during gestation of spontaneously hypertensive rats (SHR) mitigated the development of hypertension in the offspring [17]. Furthermore, exercise during pregnancy enhanced offspring insulin sensitivity and improved offspring glucose homeostasis [18]. Thus, these studies offer new insights supporting that intervention during pregnancy may be a beneficial strategy for the prevention of CVDs.
Angiotensin (Ang)-(1–7), an important peptide of the RAS, is mostly produced through the action of ACE2 on Ang II. Ang-(1–7), through Mas receptor activation, induces many beneficial actions in the cardiovascular system (for review, see Santos et al. [19]). Indeed, this heptapeptide induces several opposite effects to those elicited by Ang II by AT1 activation [20, 21]. Ang-(1–7) presents antihypertensive [22,23,24], vasodilation [25] and antiarrhythmogenic effects [26] and prevents cardiac remodeling [27, 28] and improves coronary perfusion and endothelial dysfunction [29,30,31].
Several studies have explored pharmacological ACE2 activators as tools for the treatment of cardiovascular dysfunction. 1-[(2-dimethylamino)ethylamino]-4-(hydroxymethyl)-7-[(4-methylphenyl)sulfonyloxy]-9H-xanthene-9-one (XNT) was able to increase ACE2 activity, promote the hypotensive response, improve cardiac function and reverse the cardiac and renal fibrosis in several animal models [32,33,34]. Similarly, protective effects have been reported with diminazene aceturate (DIZE), another putative ACE2 activator [35,36,37,38]. DIZE increased ACE2 activity in the kidneys [35], plasma and heart tissue [38, 39]. This compound reduced the cerebral infarct size and neurological deficits in a model of cerebral ischemia [39, 40], prevented monocrotaline-induced pulmonary hypertension [41], reduced cardiac hypertrophy and dysfunction [35, 37], and decreased the infarcted area and left ventricular remodeling post myocardial infarction in rats [38]. However, some studies have failed to show an effect of DIZE on increasing ACE2 activity [35, 42], noting, however, that the beneficial effects of DIZE might also depend on ACE2-independent mechanisms.
Thus, considering that (i) maternal exposure to adverse factors contributes to the development of cardiovascular dysfunction in the offspring, (ii) pregnant mothers exposed to beneficial stimuli can attenuate or prevent the development of injuries in the offspring, and (iii) the cardioprotective effects of the ACE2/Ang-(1–7)/Receptor Mas axis, we sought to investigate whether treatment with DIZE or Ang-(1–7) during pregnancy could attenuate the development of cardiovascular dysfunction in the adult offspring of SHRs.
Methodology
Animals
Rats were maintained in a controlled temperature (22 ± 2 °C) room with a 12 h/12 h light/dark cycle. Water and food were available ad libitum. All protocols were approved by the Animal Use Ethics Commission of Federal University of Goiás (CEUA/UFG—protocol number: 039/2017). The estrous cycle of the female SHRs (12–16 weeks old) was monitored for mating and to establish the beginning of the treatments with DIZE or Ang-(1–7). Dams were mated with male SHRs (12–16 weeks old), and vaginal smears were checked daily for the presence of spermatozoa. The presence of sperm was considered gestational day 0.
Treatment with DIZE
After confirmation of pregnancy, dams were randomly assigned to receive DIZE at a dosage of 1 mg/kg or an equal volume of filtered tap water (1 mL/kg). DIZE or saline was administered via gavage once a day throughout the gestation. On the third postnatal day, the litter was adjusted to 8 pups. After weaning, only male offspring were used for the following analyses.
Treatment with Ang-(1–7)
On the first day of Diestro II, the rats were randomly assigned to receive either saline or Ang-(1–7). For this, the female SHRs were anesthetized with tribromoethanol (0.25 g/kg, i.p.) and underwent surgery for subcutaneous implantation of an osmotic minipump containing Ang-(1–7) (delivered at a dose of 24 μg/kg/h) or saline. The infusion was kept throughout the gestation period. Two days after surgery, one SHR male and two SHR females were housed together for mating. The litter adjustment and offspring selection followed as described previously in the DIZE treatment.
Blood pressure measurement
The systolic blood pressure (SBP) was evaluated by the noninvasive method of tail-cuff plethysmography (PowerLab/400 ADInstruments). The SBP of the parents was evaluated before and during the gestational period. In the offspring, the SBP was measured from the 6th to16th weeks of age. Data were analyzed using LabChart 7 software.
Isolated heart preparation
In the 17th week of age, the male rats were euthanized by decapitation, and the left ventricular function and coronary reactivity were evaluated by isolated heart preparation according to the Langendorff technique. The hearts were excised and perfused with Krebs–Ringer solution containing NaCl 118,41 mmol/L, NaHCO3 26.24 mmol/L, KCl 4.96 mmol/L, KH2PO4 1.17 mmol/L, MgSO4·7H2O 1.17 mmol/L, CaCl2 1.25 mmol/L, and glucose 11.65 mmol/L. The solution was maintained at constant temperature (37 ± 1 °C) and oxygenation (95% O2 and 5% CO2). A water-filled balloon was inserted into the left ventricle through an incision in the left atrium to record the isovolumetric pressure. Coronary perfusion pressure was measured with a pressure transducer that was connected to the aortic cannula. In the stabilization period, the perfusion flow was adjusted to keep the perfusion pressure above 80 mmHg. Thereafter, the flow was maintained constant. After a stabilization period (30 min) and an additional 5 min to record the basal parameters, the dose-response curves for bradykinin (BK, 10−8−10−5 mol/L, bolus dose of 0.3 mL) were performed. LV pressure was recorded at a sampling rate of 1 kHz. The maximal rate of left ventricular pressure rise (dP/dt max), maximal rate of left ventricular pressure decline (dP/dt min) and heart rate were calculated from the intraventricular pressure wave. Data were analyzed using a Dataq acquisition system.
Morphometrical and stereological analyses
The hearts and kidneys were collected for morphological analyses. Left ventricles were dissected and weighed, and the ventricular mass index (VMI) was determined as the ratio of LV mass (in mg) to body weight (in g). The left ventricles were dissected out and immersed in potassium chloride solution (4 mmol/L). The medial part of the left ventricle and a half part (coronal section) of the kidneys were fixed in Metacarn solution for four hours. Thereafter, the samples were dehydrated in ethanol, clarified in xylol and embedded in paraffin. The tissue fragments were sectioned at 5 μm thickness, fixed on glass slides and stained with Picrosirius Red. The measurements of cardiomyocyte diameter were performed in the region corresponding to the nucleus and with visible cell limit. To evaluate the deposition of the interstitial and perivascular total collagen, a system coupled with a polarizing filter that facilitates the identification of the collagen fibers was used. The stereological analyses were performed on a multipoint system with 130 points to quantify the total collagen deposition. All images were obtained under a Zeiss AxioScope A1 microscope. All analyses were performed using Image Pro-Plus v6.1 software.
Western blot analysis
Left ventricle tissue samples were homogenized in lysis buffer containing 1× phosphate buffered saline, 1% Nonidet, 0.5% sodium deoxycholate, 0.1% sodium dodecyl sulfate and protease inhibitors (1 µg/mL aprotinin, 1 µg/mL pepstatin, 1 µg/mL leupeptin, 100 mM PMSF and 100 mM sodium orthovanadate). Forty micrograms of protein from each sample was separated by electrophoresis on a polyacrylamide gel and transferred to nitrocellulose membranes. Nonspecific bindings were blocked by incubation with 5% milk diluted in 0.1% Tween20 in Tris-buffered saline (TBS-T). Membranes were incubated overnight with specific primary antibodies as follows: anti-ACE (1:500, Santa Cruz Biotechnology); anti-ACE2 (1:1000, Gene tex), anti-AT1 (1:200, Santa Cruz Biotechnology), anti-AT2 (1:1000, Booster), anti-MAS (1:1000, Santa Cruz Biotechnology), anti-SOD (1:1000, Santa Cruz Biotechnology), anti-Catalase (1:1000, Santa Cruz Biotechnology), and anti-GAPDH (1:2000, Santa Cruz Biotechnology). Thereafter, the membranes were incubated with secondary antibodies. Immunoreactive bands were visualized by chemiluminescence and quantified by densitometry. ImageJ software was used to quantify the bands using GAPDH as a normalization control.
Data analysis
Data are expressed as the mean ± SEM (standard error of the mean). Experimental numbers represent fetuses or offspring from different dams. Data were analyzed by the Student’s t test or two-way analysis of variance, as appropriate. All statistical analyses were considered significant at p < 0.05. The statistical analyses were performed using GraphPad Prism 6.0 software.
Results
Effects of maternal DIZE treatment during pregnancy on the cardiovascular system of adult SHR offspring
The length of gestation was 20–21 days in both pregnant nontreated dams and those treated with DIZE. The number of pups was not different between groups (SHR: 11.7 ± 0.25 vs. SHR DIZE: 10.0 ± 1.25).
Treatment with DIZE during the gestational period attenuated the increase in SBP in adult offspring of hypertensive animals (Fig. 1). Maternal treatment with DIZE did not change the VMI (3.80 ± 0.169 vs. 3.51 ± 0.063 mg/g in SHR DIZE; P = 0.076) but significantly reduced the cardiomyocyte diameter (Fig. 2a–c) and the interstitial (Fig. 2d–f) and perivascular (Fig. 2g–i) fibrosis deposition in the left ventricles of the adult offspring rats.
Morphological analyses in the left ventricle of the offspring from hypertensive rats treated with DIZE. Representative micrographs of the a, b cardiomyocyte diameter, d, e interstitial collagen content and g, h perivascular collagen content. Quantification of the c cardiomyocyte diameter, f interstitial collagen and i perivascular collagen. Dara are expressed as the mean ± SEM. The unpaired Student’s t test, *P < 0.05
To evaluate whether changes in cardiac morphology could affect cardiac function or coronary vasodilation, isolated heart preparation was performed. Left ventricular end-systolic pressure (LVESP), dP/dt max, dP/dt min, and heart rate were not different between groups (Table 1). However, the coronary vasodilation induced by BK was significantly improved in hearts from SHR DIZE rats (Fig. 3).
Changes in the perfusion pressure induced by bradykinin in isolated hearts of the offspring from hypertensive rats treated with DIZE during pregnancy. Data are expressed as the mean ± SEM. Two-way ANOVA followed by the Tukey’s post hoc test. *P < 0.05 vs. SHR at the same concentration; +P < 0.05 vs. vehicle in the respective group
Effects of maternal Ang-(1–7) treatment during pregnancy on the cardiovascular system of adult SHR offspring
The SBP of the pregnant SHRs did not change in the gestational period. However, the blood pressure of the pregnant SHRs treated with Ang-(1–7) was reduced in the first and second weeks of the gestational period (Supplementary Figure). The length of gestation was 21 days in both groups. The number of pups was not different between treated and nontreated pregnant rats (SHR: 11 ± 0.57 vs. SHR Ang-(1–7): 10 ± 0.70).
As shown in Fig. 4, maternal treatment with Ang-(1–7) during pregnancy attenuated the increase in SBP in the offspring of hypertensive animals.
Maternal treatment with Ang-(1–7) reduced the VMI (3.14 ± 0.038 vs. 2.99 ± 0.060 mg/g in SHR Ang-(1–7), P < 0.05) and the cardiomyocyte diameter of the left ventricles from adult offspring (Fig. 5a–c). Furthermore, the interstitial (Fig. 5d–f) and perivascular (Fig. 5g–i) fibrosis deposition was significantly reduced in the left ventricles of the SHR Ang-(1–7) offspring rats.
Morphological analyses in the left ventricle of the offspring from hypertensive rats treated with Ang-(1–7). Representative micrographs of the a, b cardiomyocyte diameter, d, e interstitial collagen content and g, h perivascular collagen content. Quantification of the c cardiomyocyte diameter, f interstitial collagen and i perivascular collagen. Data are expressed as the mean ± SEM. The unpaired Student’s t test, *P < 0.05
To assess whether the effects of Ang-(1–7) treatment during gestation were also beneficial to other tissues, collagen deposition was evaluated in the kidneys of adult offspring. Similar to the hearts, this treatment significantly reduced total collagen deposition in the kidneys (Fig. 6a–c).
Table 2 presents the basal values of the isolated hearts from SHR and SHR Ang-(1–7) offspring rats. The LVESP, dP/dt max, dP/dt min, and HR were not different between groups. However, maternal treatment with Ang-(1–7) was able to improve BK-induced vasodilation in the hearts of adult offspring rats (Fig. 7).
Changes in the perfusion pressure induced by bradykinin in isolated hearts of the offspring from hypertensive rats treated with Ang-(1–7) during pregnancy. Data are expressed as the mean ± SEM. Two-way ANOVA followed by the Tukey’s post hoc test. *P < 0.05 vs. SHRs at the same concentration; + P < 0.05 vs. vehicle in the respective group
Some studies have demonstrated alterations in the expression of components of the RAS stimulated by fetal programming [43, 44]. Thus, we evaluated the protein expression of RAS components in the offspring from mothers treated with Ang-(1–7). As shown in Fig. 8, this treatment did not change the expression of the AT1 (Fig. 8a) and Mas receptors (Fig. 8c), ACE (Fig. 8d) and ACE2 (Fig. 8e) but evoked a slight reduction in the expression of the AT2 receptor (Fig. 8b) in the left ventricles of the offspring.
Furthermore, oxidative stress is an important mechanism involved in the development of cardiac remodeling. Thus, the expression of SOD and catalase in the offspring was also investigated. Maternal treatment with Ang-(1–7) did not alter the expression of these proteins (Fig. 9a, b).
Discussion
The major findings of this study were that maternal treatment of SHRs with DIZE, as well as Ang-(1–7), attenuated the increase in blood pressure, improved coronary vasodilation, and reduced cardiomyocyte hypertrophy and fibrosis deposition in the left ventricle of adult offspring.
Fetal programming has been widely studied, especially its relationship with cardiovascular dysfunction in offspring [4, 10, 13, 45]. In addition, it has been proposed that RAS is involved in this process [13, 43, 44].
In this study, maternal treatment with DIZE attenuated the increase in blood pressure in the offspring. The effect of DIZE on blood pressure has previously been demonstrated [36]. DIZE reduced the blood pressure of normotensive and hypertensive rats possibly by a mechanism involving the Mas receptor and NO [36]. In addition, this compound reduced the right ventricular systolic pressure in a monocrotaline-induced pulmonary hypertension animal model, indicating a reduction in the pulmonary arterial resistance [34].
Previous studies have demonstrated the effectiveness of DIZE in activating ACE2 [35, 36, 38, 39], which could increase Ang-(1–7) formation. In addition, the antihypertensive action of Ang-(1–7) has been widely described [23, 46]. Therefore, the effect of maternal treatment with Ang-(1–7) was evaluated to determine whether this peptide could also promote beneficial effects in the cardiovascular system of offspring. Interestingly, this treatment also attenuated the increase in blood pressure in adult male offspring. Although several studies have demonstrated that DIZE was able to increase ACE2 activity [35, 36, 38, 39], others have failed to demonstrate this effect [35, 42]. Thus, we cannot rule out the possibility that DIZE, in our study, has promoted its beneficial effects independently of ACE2.
Pregnancy promotes several alterations in the RAS, even in hypertensive states [47,48,49,50,51,52]. Reduced AT1 and increased AT2 expression were observed in the kidneys of pregnant SHRs [47]. In addition, the expression of ACE and AT1 receptor was lower in mesenteric arteries in these animals [48]. Pregnant women present significantly higher plasma angiotensin II [49]. Furthermore, plasma levels of Ang-(1–7) are reduced in preeclampsia subjects [50, 51]. Similarly, the Ang-(1–7) concentration was significantly decreased in an animal model of preeclampsia [52]. Thus, it is possible that the treatment with DIZE or Ang-(1–7) could shift the RAS balance by increasing the activity of the ACE2/Ang-(1–7)/Mas axis, which in turn could lead to an improvement in the uterine blood flow and therefore in beneficial effects in the offspring. Indeed, numerous studies have shown that Ang-(1–7) elicits vasodilation by an endothelium-dependent release of nitric oxide [30, 53,54,55]. However, one cannot rule out the possibility that the reduction in the blood pressure in offspring is due to the effect of Ang-(1–7) of reducing the blood pressure in pregnant rats.
The reduced blood pressure in offspring from mothers treated with DIZE or Ang-(1–7) was accompanied by an improvement in the coronary dilation induced by bradykinin, an endothelium-dependent vasodilator. Our group has previously demonstrated that treatment with DIZE improved coronary flow in isolated hearts from pressure-overloaded rats. Likewise, XNT, an ACE2 activator, improved endothelial function in both SHRs and diabetic Wistar rats [32]. Several studies have reported that Ang-(1–7) is also able to improve endothelium function [56, 57]. Hence, these data suggest that both treatments performed in this study improved endothelial function in the coronary bed of the male offspring. However, since elevated blood pressure itself can trigger damage to endothelial function [58], we cannot assert whether the improvement in coronary endothelial function was due to the direct effect of Ang-(1–7) or indirectly from the reduction in blood pressure in the pregnant rats.
Maternal exposure to DIZE or Ang-(1–7) promoted a significant reduction in cardiomyocyte diameter and fibrosis deposition in the male offspring. These effects may be caused by the reduced blood pressure observed in the offspring. However, a previous study has shown that adult offspring of mice exposed to small pollutant particles during the gestational period presented hypertrophy with increased mRNA of hypertrophic genes through a mechanism involving histone acetylation modification [59]. In addition, an increase in the molecular markers for cardiac dysfunction was reported in the prehypertensive stage of SHRs [60], suggesting that the cardiac remodeling in SHRs is, at least in part, independent of blood pressure. Therefore, it is possible that treatment with DIZE and Ang-(1–7) promoted molecular effects in the fetus, i.e., through epigenetic modifications.
Similar to the results observed in hearts, treatment with Ang-(1–7) significantly reduced total collagen deposition in the kidneys. These data suggest that the treatment during gestation was not restricted to the heart. The protective effects of Ang-(1–7) in kidneys have been shown in previous studies [61,62,63]. Ang-(1–7) prevented kidney injury in hypertensive [62] and diabetic [61] animal models. Moreover, genetic deletion of the Mas receptor leads to renal fibrosis [63].
Some studies have shown that alterations in the expression of components of the RAS induced by fetal programming (with high sucrose intake [13], hyperthyroidism induction [43] or renovascular hypertension [44] during gestation) are associated with cardiovascular dysfunction in the offspring. Furthermore, Lee et al. [64] showed that ACE is upregulated in several tissues in SHRs via histone code modifications [64]. In our study, treatment with Ang-(1–7) did not change the expression of the AT1, Mas receptor, ACE or ACE2 but reduced the expression of the AT2 receptor. Although some studies support a cardioprotective role of the AT2 receptor [65], there is accumulating evidence suggesting that the contribution of the AT2 receptor to the development of cardiac hypertrophy is very complex and its role in cardiac remodeling remains controversial [65]. For instance, gene overexpression or pharmacological stimulation of the AT2 receptor promoted an antihypertrophic effect [66, 67]. On the other hand, chronic loss of AT2 abolished cardiac hypertrophy and fibrosis [68]. Thus, we cannot assert that the cardioprotection observed in the male offspring is associated with reduced AT2 expression in the hearts. Further experiments are needed to better understand these data.
Oxidative stress has been identified as one of the key contributing factors in the development of hypertension and cardiac hypertrophy [69]. Therefore, we evaluated the expression of antioxidant enzymes in the left ventricles of male offspring. We did not observe any difference in the expression of SOD or catalase between groups, suggesting that the protective effects found in the offspring from dams treated with Ang-(1–7) can be mediated by an oxidative stress-independent mechanism.
In summary, we found that treatment with DIZE or Ang-(1–7) during gestation promoted substantial effects in attenuating hypertension and cardiac remodeling in male adult offspring. Although the mechanisms underlying this improvement require further investigation, the degree of the beneficial effects was notable. It should be emphasized that Ang-(1–7) is an endogenous peptide, thus resulting in a very low risk of adverse effects for mothers or fetuses. Thus, these data indicate that the pharmacological management toward increasing the activity of the ACE2-Ang-(1–7)-Mas receptor axis during pregnancy may be a beneficial strategy to attenuate or prevent CVDs in descendants.
References
WHO. Global status report on noncommunicable diseases 2014. World Health Organization; 2014. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
Stevens B, Pezzullo L, Verdian L, Tomlinson J, George A, Bacal F. The economic burden of heart conditions in Brazil. Arq Bras Cardiol. 2018;111:29–36.
Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015;386:801–12.
Wise I, Charchar F. Epigenetic modifications in essential hypertension. Int J Mol Sci. 2016;17:451.
Stoll S, Wang C, Qiu H. DNA methylation and histone modification in hypertension. Int J Mol Sci. 2018;19:1174.
Ciccarone F, Castelli S, Ioannilli L, Ciriolo MR. High dietary fat intake affects DNA methylation/ hydroxymethylation in mouse heart: epigenetic hints for obesity-related cardiac dysfunction. Mol Nutr Food Res. 2019;63:1–14.
Itani N, Salinas CE, Villena M, Skeffington KL, Beck C, Villamor E, et al. The highs and lows of programmed cardiovascular disease by developmental hypoxia: studies in the chicken embryo. J Physiol. 2018;596:2991–3006.
Nguyen T, Li GE, Chen H, Cranfield CG, McGrath KC, Gorrie CA. Maternal e-cigarette exposure results in cognitive and epigenetic alterations in offspring in a mouse model. Chem Res Toxicol. 2018;31:601–11.
Guan J, Mao C, Xu F, Geng C, Zhu L, Wang A, et al. Prenatal dehydration alters renin–angiotensin system associated with angiotensin-increased blood pressure in young offspring. Hypertens Res. 2010;14:384–99.
Bogdarina I, Welham S, King PJ, Burns SP, Clark AJL. Epigenetic modification of the renin-angiotensin system in the fetal programming of hypertension. Circ Res. 2007;100:520–6.
Xiao D, Dasgupta C, Li Y, Huang X, Zhang L. Perinatal nicotine exposure increases angiotensin II receptor-mediated vascular contractility in adult offspring. PLoS ONE. 2014;9:e108161.
Xiao D, Xu Z, Huang X, Longo LD, Yang S, Zhang L. Prenatal gender-related nicotine exposure increases blood pressure response to angiotensin II in adult offspring. Hypertension. 2008;51:1239–47.
Wu L, Shi A, Zhu D, Bo L, Zhong Y, Wang J, et al. High sucrose intake during gestation increases angiotensin II type 1 receptor-mediated vascular contractility associated with epigenetic alterations in aged offspring rats. Peptides. 2016;86:133–44.
Guan J, Mao C, Xu F, Geng C, Zhu L, Wang A, et al. Prenatal dehydration alters renin-angiotensin system associated with angiotensin-increased blood pressure in young offspring. Hypertens Res. 2009;32:1104–11.
Saito T, Musha Y, Miyakawa M, Itoh S, Ohtsuji M, Hanson MA, et al. Angiotensin II receptor antagonist reduces subsequent uterine arterial dysfunction in pregnant offspring of protein-restricted rat dams. J Obstet Gynaecol Res. 2012;38:483–9.
MohanKumar SMJ, King A, Shin AC, Sirivelu MP, MohanKumar PS, Fink GD. Developmental programming of cardiovascular disorders: focus on hypertension. Rev Endocr Metab Disord. 2007;8:115–25.
Care AS, Sung MM, Panahi S, Gragasin FS, Dyck JRB, Davidge ST, et al. Perinatal resveratrol supplementation to spontaneously hypertensive rat dams mitigates the development of hypertension in adult offspring. Hypertension. 2016;67:1038–44.
Carter LG, NR QI, Cabo R, Pearson KJ. Maternal exercise improves insulin sensitivity in mature rat offspring. Med Sci Sport Exerc. 2013;45:832–40.
Santos RAS, Sampaio WO, Alzamora AC, Motta-Santos D, Alenina N, Bader M, et al. The ACE2/angiotensin-(1–7)/MAS axis of the renin-angiotensin system: focus on angiotensin-(1–7). Physiol Rev. 2018;98:505–53.
Ferreira AJ, Murca TM, Fraga-Silva RA, Castro CH, Raizada MK, Santos RA. New cardiovascular and pulmonary therapeutic strategies based on the angiotensin-converting enzyme 2/angiotensin-(1–7)/mas receptor axis. Int J Hypertension. 2012;2012:147825.
Santos RA. Angiotensin-(1–7). Hypertension. 2014;63:1138–47.
Campagnole-Santos MJ, Heringer SB, Batista EN, Khosla MC, Santos RA. Differential baroreceptor reflex modulation by centrally infused angiotensin peptides. Am J Physiol. 1992;263:89–94.
Benter IF, Ferrario CM, Morris M, Diz DI. Antihypertensive actions of angiotensin-(1–7) in spontaneously hypertensive rats. Am J Physiol. 1995;269:313–9.
Ferrario CM, Chappell MC, Tallant EA, Brosnihan KB, Diz DI. Counterregulatory actions of angiotensin-(1–7). Hypertension. 1997;30:535–41.
Oliveira MA, Fortes ZB, Santos RAS, Kosla MC, De Carvalho MHC. Synergistic effect of angiotensin-(1–7) on bradykinin arteriolar dilation in vivo. Peptides. 1999;20:1195–201.
Ferreira AJ, Santos RAS, Almeida AP. Angiotensin-(1–7): cardioprotective effect in myocardial ischemia/reperfusion. Hypertension. 2001;38:665–8.
McCollum LT, Gallagher PE, Ann Tallant E. Angiotensin-(1–7) attenuates angiotensin II-induced cardiac remodeling associated with upregulation of dual-specificity phosphatase 1. Am J Physiol Heart Circ Physiol. 2012;302:801–10.
Mercure C, Yogi A, Callera GE, Aranha AB, Bader M, Ferreira AJ, et al. Angiotensin(1–7) blunts hypertensive cardiac remodeling by a direct effect on the heart. Circ Res. 2008;103:1319–26.
Moraes PL, Kangussu LM, Castro CH, Almeida AP, Santos RASFA. Vasodilator effect of angiotensin-(1–7) on vascular coronary bed of rats: role of Mas, ACE and ACE2. Protein Pept Lett. 2017;24:869–75.
Souza APS, Sobrinho DBS, Almeida JFQ, Alves GMM, Macedo LM, Porto JE, et al. Angiotensin II type 1 receptor blockade restores angiotensin-(1–7)-induced coronary vasodilation in hypertrophic rat hearts. Clin Sci. 2013;125:449–59.
Almeida AP, Frabregas BC, Madureira MM, Santos RJA, Campagnole-Santos MJ, Santos RJA. Angiotensin-(1–7) potentiates the coronary vasodilatatory effect of bradykinin in the isolated rat heart. Braz J Med Biol Res. 2000;33:709–13.
Fraga-Silva RA, Costa-Fraga FP, Murça TM, Moraes PL, Lima AM, Lautner RQ, et al. Angiotensin-converting enzyme 2 activation improves endothelial function. Hypertension. 2013;61:1233–8.
Murca TM, Almeida TC, Raizada MK, Ferreira AJ. Chronic activation of endogenous angiotensin-converting enzyme 2 protects diabetic rats from cardiovascular autonomic dysfunction. Exp Physiol. 2012;97:699–709.
Ferreira AJ, Shenoy V, Qi Y, Fraga-Silva RA, Santos RAS, Katovich MJ, et al. Angiotensin-converting enzyme 2 activation protects against hypertension-induced cardiac fibrosis involving extracellular signal-regulated kinases. Exp Physiol. 2011;96:287–94.
Velkoska E, Patel SK, Griggs K, Pickering RJ, Tikellis C, Burrell LM. Short-term treatment with diminazene aceturate ameliorates the reduction in kidney ACE2 activity in rats with subtotal nephrectomy. PLoS ONE. 2015;10:e0118758.
De Maria MLA, Araújo LD, Fraga-Silva RA, Pereira LAS, Ribeiro HJ, Menezes GB, et al. Anti-hypertensive effects of diminazene aceturate: an angiotensin- converting enzyme 2 activator in rats. Protein Pept Lett. 2016;23:9–16.
Macedo LM, Souza APS, De Maria MLA, Borges CL, Soares CMA, Pedrino GR, et al. Cardioprotective effects of diminazene aceturate in pressure-overloaded rat hearts. Life Sci. 2016;155:63–9.
Qi Y, Zhang J, Cole-Jeffrey CT, Shenoy V, Espejo A, Hanna M, et al. Diminazene aceturate enhances angiotensin-converting enzyme 2 activity and attenuates ischemia-induced cardiac pathophysiology. Hypertension. 2013;62:746–52.
Bennion DM, Haltigan EA, Irwin AJ, Donnangelo LL, Regenhardt RW, Pioquinto DJ, et al. Activation of the neuroprotective angiotensin-converting enzyme 2 in rat ischemic stroke. Hypertension. 2015;66:141–8.
Mecca AP, Regenhardt RW, Connor TEO, Joseph JP, Raizada MK, Katovich MJ, et al. Cerebroprotection by angiotensin-(1–7) in endothelin-1-induced ischaemic stroke. Exp Physiol. 2011;96:1084–96.
Shenoy V, Gjymishka A, Jarajapu YP, Qi Y, Afzal A, Rigatto K, et al. Diminazene attenuates pulmonary hypertension and improves angiogenic progenitor cell functions in experimental models. Am J Respir Crit Care Med. 2013;187:648–57.
Haber PK, Ye M, Wysocki J, Maier C, Haque SK, Batlle D. Angiotensin-converting enzyme 2–independent action of presumed angiotensin-converting enzyme 2. Hypertension. 2014;63:774–82.
Lino CA, da Silva IB, Shibata CER, Monteiro P, de S, Barreto-Chaves MLM. Maternal hyperthyroidism increases the susceptibility of rat adult offspring to cardiovascular disorders. Mol Cell Endocrinol. 2015;416:1–8.
Guo Q, Feng X, Xue H, Teng X, Jin S, Duan X, et al. Maternal renovascular hypertensive rats treatment with hydrogen sulfide increased the methylation of AT1b gene in offspring. Am J Hypertens. 2017;30:1220–7.
Mukerjee S, Zhu Y, Zsombok A, Mauvais-Jarvis F, Zhao J, Lazartigues E. Perinatal exposure to western diet programs autonomic dysfunction in the male offspring. Cell Mol Neurobiol. 2018;38:233–42.
Costa MA, Verrilli MAL, Gomez KA, Nakagawa P, Peña C, Arranz C, et al. Angiotensin- (1–7) upregulates cardiac nitric oxide synthase in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol. 2010;299:1205–11.
Iacono A, Bianco G, Raso GM, Esposito E, Bianca REV, Sorrentino R, et al. Maternal adaptation in pregnant hypertensive rats: improvement of vascular and inflammatory variables and oxidative damage in the kidney. Am J Hypertens. 2009;22:777–83.
Ognibene DT, Carvalho LCRM, Costa CA, Rocha APM, Moura RS, Resende ÂC. Role of renin-angiotensin system and oxidative status on the maternal cardiovascular regulation in spontaneously hypertensive rats. Am J Hypertens. 2012;25:498–504.
Hanssens MS, KEIRSE MJ, Spitz B, Van Assche FA. Measurement of individual plasma angiotensins in normal pregnancy and pregnancy-induced hypertension. J Clin Endocrinol Metab. 1991;73:489–94.
Brosnihan KB, Neves LAA, Anton L, Joyner J, Valdes G, Merrill DC. Enhanced expression of Ang- (1–7) during pregnancy. Braz J Med Biol Res. 2004;37:1255–62.
Merrill DC, Karoly M, Chen K, Ferrario CM, Brosnihan KB. Angiotensin-(1–7) in normal and preeclamptic pregnancy. Endocrine. 2002;18:239–45.
Joyner J, Neves LAA, Granger JP, Alexander BT, Merrill DC, Chappell MC, et al. Temporal-spatial expression of ANG- (1–7) and angiotensin-converting enzyme 2 in the kidney of normal and hypertensive pregnant rats. Am J Physiol Regul Integr Physiol. 2007;293:169–77.
Silva DMR, Vianna HR, Cortes SF, Campagnole-Santos MJ, Santos RAS, Lemos VS. Evidence for a new angiotensin-(1–7) receptor subtype in the aorta of Sprague-Dawley rats. Peptides. 2007;28:702–7.
Nunes ADC, Souza APS, Macedo LM, Alves PH, Pedrino GR, Colugnati DB, et al. Influence of antihypertensive drugs on aortic and coronary effects of Ang-(1–7) in pressure-overloaded rats. Braz J Med Biol Res. 2017;50:1–8.
Feterik K, Smith L, Katusic ZS. Angiotensin-(1–7) causes endothelium-dependent relaxation in canine middle cerebral artery. Brain Res. 2000;873:75–82.
Beyer AM, Guo D, Rahmouni K, City I, City I. Prolonged treatment withangiotensin1–7 improves endothelial function in diet-induced obesity. J Hypertens. 2013;31:730–8.
Faria-silva R, Duarte FV, Santos RAS. Improves endothelial function in normotensive rats. Hypertension. 2005;46:948–52.
Voorde J Van De, Vanheel B, Leusen I, et al. Depressed endothelium-dependent relaxation in hypertension: relation to increased blood pressure and reversibility. Eur J Physiol. 1988;411:500–4.
Wu X, Pan B, Liu L, Zhao W, Zhu J, Huang X, et al. In utero exposure to PM2.5 during gestation caused adult cardiac hypertrophy through histone acetylation modification. J Cell Biochem. 2019;120:4375–84.
Matsuo H, Kitamura K, Kangawa K, Minamino N, Yokota N, Eto T, et al. Alterations in circulating and cardiac tissue concentrations of brain natriuretic peptide in spontaneously hypertensive rats. Cardiovasc Res. 1993;27:1312–5.
Shi Y, Lo C-S, Padda R, Abdo S, Chenier I, Filep JG, et al. Angiotensin-(1–7) prevents systemic hypertension, attenuates oxidative stress and tubulointerstitial fibrosis, and normalizes renal angiotensin-converting enzyme 2 and Mas receptor expression in diabetic mice. Clin Sci. 2015;128:649–63.
Chen Y, Zhao W, Liu C, Meng W, Zhao T, Bhattacharya SK, et al. Molecular and cellular effect of angiotensin 1–7 on hypertensive kidney disease. Am J Hypertens. 2019;32:460–7.
Pinheiro SV, Ferreira AJ, Kitten GT, da Silveira KD, da Silva DA, Santos SH, et al. Genetic deletion of the angiotensin-(1–7) receptor Mas leads to glomerular hyperfiltration and microalbuminuria. Kidney Int. 2009;75:1184–93.
Lee HA, Cho HM, Lee DY, Kim KC, Han HS, Kim IK. Tissue-specific upregulation of angiotensin-converting enzyme 1 in spontaneously hypertensive rats through histone code modifications. Hypertension. 2012;59:621–6.
Kaschina E, Namsolleck P, Unger T. AT2 receptors in cardiovascular and renal diseases. Pharmacol Res. 2017;125:39–47.
Falcón BL, Stewart JM, Bourassa E, Katovich MJ, Walter G, Speth RC, et al. Angiotensin II type 2 receptor gene transfer elicits cardioprotective effects in an angiotensin II infusion rat model of hypertension. Physiol Genomics. 2004;19:255–61.
Dopona EPB, Rocha VF, Furukawa LNS, Oliveira IB, Heimann JC. Nutrition, metabolism & cardiovascular diseases myocardial hypertrophy induced by high salt consumption is prevented by angiotensin II AT2 receptor agonist. Nutr Metab Cardiovasc Dis. 2018;23:301–5.
Ichihara S, Senbonmatsu T, Price E, Ichiki T, Gaffney FA, Inagami T. Angiotensin II type 2 receptor is essential for left ventricular hypertrophy and cardiac fibrosis in chronic angiotensin II-induced hypertension. Circulation. 2001;104:346–51.
Takimoto E, Kass DA. Role of oxidative stress in cardiac hypertrophy and remodeling. Hypertension. 2007;49:241–8.
Acknowledgements
This work was supported by grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundação de Amparo à Pesquisa do Estado de Goiás (FAPEG), and Programa de Educação Tutorial (PET-SeSU-MEC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bessa, A.S.M., Jesus, É.F., Nunes, A.D.C. et al. Stimulation of the ACE2/Ang-(1–7)/Mas axis in hypertensive pregnant rats attenuates cardiovascular dysfunction in adult male offspring. Hypertens Res 42, 1883–1893 (2019). https://doi.org/10.1038/s41440-019-0321-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0321-8
Keywords
This article is cited by
-
Nuclear import of Mas-related G protein-coupled receptor member D induces pathological cardiac remodeling
Cell Communication and Signaling (2023)
-
Novel therapeutics for the treatment of hypertension and its associated complications: peptide- and nonpeptide-based strategies
Hypertension Research (2021)
-
Sex Differences in Association Between Anti-Hypertensive Medications and Risk of COVID-19 in Middle-Aged and Older Adults
Drugs & Aging (2021)