Abstract
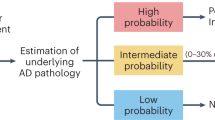
Biomarker discovery and development for clinical research, diagnostics and therapy monitoring in clinical trials have advanced rapidly in key areas of medicine — most notably, oncology and cardiovascular diseases — allowing rapid early detection and supporting the evolution of biomarker-guided, precision-medicine-based targeted therapies. In Alzheimer disease (AD), breakthroughs in biomarker identification and validation include cerebrospinal fluid and PET markers of amyloid-β and tau proteins, which are highly accurate in detecting the presence of AD-associated pathophysiological and neuropathological changes. However, the high cost, insufficient accessibility and/or invasiveness of these assays limit their use as viable first-line tools for detecting patterns of pathophysiology. Therefore, a multistage, tiered approach is needed, prioritizing development of an initial screen to exclude from these tests the high numbers of people with cognitive deficits who do not demonstrate evidence of underlying AD pathophysiology. This Review summarizes the efforts of an international working group that aimed to survey the current landscape of blood-based AD biomarkers and outlines operational steps for an effective academic–industry co-development pathway from identification and assay development to validation for clinical use.
Key points
-
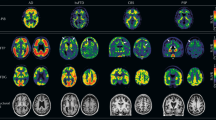
Cerebrospinal fluid (CSF) and PET markers of amyloid-β and tau proteins are accurate in detecting the neuropathological changes of Alzheimer disease (AD).
-
The use of CSF and PET biomarkers is limited by invasiveness or high costs; to address these issues, blood-based AD biomarkers are eagerly awaited.
-
An international, interdisciplinary expert working group was convened by the Alzheimer’s Precision Medicine Initiative to discuss the ideal development process for blood-based biomarkers.
-
Nineteen blood-based biomarker assays were selected by the working group for further consideration.
-
The working group outlined the pathway from biomarker identification and assay development to validation for clinical use and proposed clear steps for effective academic–industry co-development of blood-based AD biomarkers.
-
The development, standardization and validation of blood-based biomarkers will be paramount to the implementation of precision medicine in AD.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Alzheimer’s Association. 2016 Alzheimer’s disease facts and figures. Alzheimers Dement. 12, 459–509 (2016).
Scheltens, P. et al. Alzheimer’s disease. Lancet 388, 505–517 (2016).
Olsson, B. et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 15, 673–684 (2016).
Lista, S. & Hampel, H. Synaptic degeneration and neurogranin in the pathophysiology of Alzheimer’s disease. Expert Rev. Neurother 17, 47–57 (2017).
Baldacci, F., Lista, S., Cavedo, E., Bonuccelli, U. & Hampel, H. Diagnostic function of the neuroinflammatory biomarker YKL-40 in Alzheimer’s disease and other neurodegenerative diseases. Expert Rev. Proteomics 14, 285–299 (2017).
Heneka, M. T. et al. Neuroinflammation in Alzheimer’s disease. Lancet Neurol. 14, 388–405 (2015).
Iturria-Medina, Y. et al. Early role of vascular dysregulation on late-onset Alzheimer’s disease based on multifactorial data-driven analysis. Nat. Commun. 7, 11934 (2016).
de la Monte, S. M. & Tong, M. Brain metabolic dysfunction at the core of Alzheimer’s disease. Biochem. Pharmacol. 88, 548–559 (2014).
James, B. D. et al. TDP-43 stage, mixed pathologies, and clinical Alzheimer’s-type dementia. Brain 139, 2983–2993 (2016).
Kovacs, G. G. et al. Non-Alzheimer neurodegenerative pathologies and their combinations are more frequent than commonly believed in the elderly brain: a community-based autopsy series. Acta Neuropathol. 126, 365–384 (2013).
Rahimi, J. & Kovacs, G. G. Prevalence of mixed pathologies in the aging brain. Alzheimers Res. Ther. 6, 82 (2014).
Attems, J. & Jellinger, K. A. The overlap between vascular disease and Alzheimer’s disease—lessons from pathology. BMC Med. 12, 206 (2014).
Hardy, J. A. & Higgins, G. A. Alzheimer’s disease: the amyloid cascade hypothesis. Science 256, 184–185 (1992).
Blennow, K., Hampel, H., Weiner, M. & Zetterberg, H. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat. Rev. Neurol. 6, 131–144 (2010). This comprehensive review summarizes the role of both CSF and plasma biomarkers in the diagnosis of AD as well as in drug discovery and clinical trials.
Hampel, H. & Lista, S. Alzheimer disease: from inherited to sporadic AD-crossing the biomarker bridge. Nat. Rev. Neurol. 8, 598–600 (2012).
Kim, D., Kim, Y. S., Shin, D. W., Park, C. S. & Kang, J. H. Harnessing cerebrospinal fluid biomarkers in clinical trials for treating Alzheimer’s and Parkinson’s diseases: potential and challenges. J. Clin. Neurol. 12, 381–392 (2016).
Frisoni, G. B. et al. Strategic roadmap for an early diagnosis of Alzheimer’s disease based on biomarkers. Lancet Neurol. 16, 661–676 (2017).
Patterson, V., Humphreys, J. & Chua, R. Email triage of new neurological outpatient referrals from general practice. J. Neurol. Neurosurg. Psychiatry 75, 617–620 (2004).
The Gerontological Society of America. The Gerontological Society of America Workgroup on cognitive impairment detection and earlier diagnosis: report and recommendations. https://changeagents365.org/resources/ways-to-stay-engaged/the-gerontological-society-of-america/Cognitive%20Impairment%20Recommendations%20Report_GSA.pdf (2015).
Chen, L. M., Farwell, W. R. & Jha, A. K. Primary care visit duration and quality: does good care take longer? Arch. Intern. Med. 169, 1866–1872 (2009).
Cannon, P. & Larner, A. J. Errors in the scoring and reporting of cognitive screening instruments administered in primary care. Neurodegener. Dis. Manag. 6, 271–276 (2016).
Wojtowicz, A. & Larner, A. J. General practitioner assessment of cognition: use in primary care prior to memory clinic referral. Neurodegener. Dis. Manag. 5, 505–510 (2015).
Garcia-Ptacek, S. et al. Differences in diagnostic process, treatment and social support for Alzheimer’s dementia between primary and specialist care: results from the Swedish dementia registry. Age Ageing 46, 314–319 (2017).
Hampel, H. et al. A precision medicine initiative for Alzheimer’s disease: the road ahead to biomarker-guided integrative disease modeling. Climacteric 20, 107–118 (2017). This landmark paper describes the initiation and development of the APMI.
O’Bryant, S. E. et al. Blood-based biomarkers in Alzheimer disease: current state of the science and a novel collaborative paradigm for advancing from discovery to clinic. Alzheimers Dement. 13, 45–58 (2017). This article provides a comprehensive review of the recent literature on blood-based biomarkers in AD and proposes a novel collaborative paradigm for advancing the field from discovery to the clinic.
Lista, S. et al. CSF Aβ1-42 combined with neuroimaging biomarkers in the early detection, diagnosis and prediction of Alzheimer’s disease. Alzheimers Dement. 10, 381–392 (2014).
Lista, S. et al. Biomarkers in sporadic and familial Alzheimer’s disease. J. Alzheimers Dis. 47, 291–317 (2015).
Dubois, B. et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 13, 614–629 (2014).
McKhann, G. M. et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7, 263–269 (2011).
Inekci, D., Jonesco, D. S., Kennard, S., Karsdal, M. A. & Henriksen, K. The potential of pathological protein fragmentation in blood-based biomarker development for dementia - with emphasis on Alzheimer’s disease. Front. Neurol. 6, 90 (2015).
Vandenberghe, R., Adamczuk, K., Dupont, P., Laere, K. V. & Chetelat, G. Amyloid PET in clinical practice: its place in the multidimensional space of Alzheimer’s disease. Neuroimage Clin. 2, 497–511 (2013).
Hampel, H. et al. Perspective on future role of biological markers in clinical therapy trials of Alzheimer’s disease: a long-range point of view beyond 2020. Biochem. Pharmacol. 88, 426–449 (2014).
Hampel, H. et al. Biomarkers for Alzheimer’s disease: academic, industry and regulatory perspectives. Nat. Rev. Drug Discov. 9, 560–574 (2010). This article provides an in-depth and critical description of the role of biomarkers for AD from academic, industry and regulatory viewpoints.
Hampel, H., Lista, S. & Khachaturian, Z. S. Development of biomarkers to chart all Alzheimer’s disease stages: the royal road to cutting the therapeutic gordian knot. Alzheimers Dement. 8, 312–336 (2012). This article is a milestone in the discovery, development, validation and qualification processes of biological markers for AD.
Cavedo, E. et al. The road ahead to cure Alzheimer’s disease: development of biological markers and neuroimaging methods for prevention trials across all stages and target populations. J. Prev. Alzheimers Dis. 1, 181–202 (2014).
Hampel, H. & Lista, S. Use of biomarkers and imaging to assess pathophysiology, mechanisms of action and target engagement. J. Nutr. Health Aging 17, 54–63 (2013).
Lista, S. et al. Evolving evidence for the value of neuroimaging methods and biological markers in subjects categorized with subjective cognitive decline. J. Alzheimers Dis. 48 (Suppl. 1), S171–S191 (2015).
Trojanowski, J. Q. & Hampel, H. Neurodegenerative disease biomarkers: guideposts for disease prevention through early diagnosis and intervention. Prog. Neurobiol. 95, 491–495 (2011).
Hampel, H. et al. Precision medicine — the golden gate for detection, treatment and prevention of Alzheimer’s disease. J. Prev. Alzheimers Dis. 3, 243–259 (2016). This pivotal article introduces the concept of precision medicine in AD.
Hampel, H. et al. Precision pharmacology for Alzheimer’s disease. Pharmacol. Res. 130, 331–365 (2018). This landmark article focuses on the paradigm of precision pharmacology, an exploratory and integrative strategy to complex diseases — including AD — aimed at identifying aberrant molecular pathways and predicting their temporal impact at the systems level.
Hampel, H. et al. Revolution of Alzheimer precision neurology. Passageway of systems biology and neurophysiology. J. Alzheimers Dis. 64, S47–S105 (2018). This paper highlights the development of the precision neurology paradigm in AD and the growing importance of the APMI movement.
Ferretti, M. et al. Sex differences in Alzheimer disease — the gateway to precision neurology. Nat. Rev. Neurol. 14, 457–469 (2018).
Lyman, G. H. & Moses, H. L. Biomarker tests for molecularly targeted therapies — the key to unlocking precision medicine. N. Engl. J. Med. 375, 4–6 (2016).
Lista, S. et al. Application of systems theory in longitudinal studies on the origin and progression of Alzheimer’s disease. Methods Mol. Biol. 1303, 49–67 (2016).
Noorbakhsh, F., Overall, C. M. & Power, C. Deciphering complex mechanisms in neurodegenerative diseases: the advent of systems biology. Trends Neurosci. 32, 88–100 (2009).
Deyati, A., Younesi, E., Hofmann-Apitius, M. & Novac, N. Challenges and opportunities for oncology biomarker discovery. Drug Discov. Today 18, 614–624 (2013).
Krutovskikh, V. A. & Herceg, Z. Oncogenic microRNAs (oncomiRs) as a new class of cancer biomarkers. Bioessays 32, 894–904 (2010).
Schröder, H., Grösche, M., Adler, M., Spengler, M. & Niemeyer, C. M. Immuno-PCR with digital readout. Biochem. Biophys. Res. Commun. 488, 311–315 (2017).
Niemeyer, C. M., Adler, M. & Wacker, R. Immuno-PCR: high sensitivity detection of proteins by nucleic acid amplification. Trends Biotechnol. 23, 208–216 (2005).
Castrillo, J. I. & Oliver, S. G. Alzheimer’s as a systems-level disease involving the interplay of multiple cellular networks. Methods Mol. Biol. 1303, 3–48 (2016).
Nakamura, A. et al. High performance plasma amyloid-beta biomarkers for Alzheimer’s disease. Nature 554, 249–254 (2018).
Ovod, V. et al. Amyloid β concentrations and stable isotope labeling kinetics of human plasma specific to central nervous system amyloidosis. Alzheimers Dement. 13, 841–849 (2017).
Janelidze, S. et al. Plasma β-amyloid in Alzheimer’s disease and vascular disease. Sci. Rep. 6, 26801 (2016).
Weston, P. S. et al. Serum neurofilament light in familial Alzheimer disease: a marker of early neurodegeneration. Neurology 89, 2167–2175 (2017).
Mattsson, N., Andreasson, U., Zetterberg, H. & Blennow, K. Alzheimer’s Disease Neuroimaging Initiative. Association of plasma neurofilament light with neurodegeneration in patients with Alzheimer disease. JAMA Neurol. 74, 557–566 (2017).
O’Brien, J. T. & Herholz, K. Amyloid imaging for dementia in clinical practice. BMC Med. 13, 163 (2015).
Henriksen, K. et al. The future of blood-based biomarkers for Alzheimer’s disease. Alzheimers Dement. 10, 115–131 (2014).
de Almeida, S. M. et al. Incidence of post-dural puncture headache in research volunteers. Headache 51, 1503–1510 (2011).
Schneider, P., Hampel, H. & Buerger, K. Biological marker candidates of Alzheimer’s disease in blood, plasma, and serum. CNS Neurosci. Ther. 15, 358–374 (2009).
Thambisetty, M. & Lovestone, S. Blood-based biomarkers of Alzheimer’s disease: challenging but feasible. Biomark. Med. 4, 65–79 (2010).
O’Bryant, S. E. et al. A blood screening test for Alzheimer’s disease. Alzheimers Dement. (Amst.) 3, 83–90 (2016).
van Gool, A. J. et al. Bridging the translational innovation gap through good biomarker practice. Nat. Rev. Drug Discov. 16, 587–588 (2017).
Lista, S., Faltraco, F., Prvulovic, D. & Hampel, H. Blood and plasma-based proteomic biomarker research in Alzheimer’s disease. Prog. Neurobiol. 101–102, 1–17 (2013).
Naj, A. C. & Schellenberg, G. D. Alzheimer’s Disease Genetics Consortium (ADGC). Genomic variants, genes, and pathways of Alzheimer’s disease: an overview. Am. J. Med. Genet. B Neuropsychiatr. Genet. 174, 5–26 (2017).
Bertram, L. & Hampel, H. The role of genetics for biomarker development in neurodegeneration. Prog. Neurobiol. 95, 501–504 (2011).
Pimenova, A. A., Raj, T. & Goate, A. M. Untangling genetic risk for Alzheimer’s disease. Biol. Psychiatry 83, 300–310 (2018).
Genomes Project, C. et al. A map of human genome variation from population-scale sequencing. Nature 467, 1061–1073 (2010).
Genomes Project, C. et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Snyder, H. M. et al. Developing novel blood-based biomarkers for Alzheimer’s disease. Alzheimers Dement. 10, 109–114 (2014).
Galasko, D. & Golde, T. E. Biomarkers for Alzheimer’s disease in plasma, serum and blood — conceptual and practical problems. Alzheimers Res. Ther. 5, 10 (2013).
Zipser, B. D. et al. Microvascular injury and blood–brain barrier leakage in Alzheimer’s disease. Neurobiol. Aging 28, 977–986 (2007).
Montagne, A. et al. Blood-brain barrier breakdown in the aging human hippocampus. Neuron 85, 296–302 (2015).
Lewczuk, P. et al. Electrophoretic separation of amyloid β peptides in plasma. Electrophoresis 25, 3336–3343 (2004).
Arvanitakis, Z., Lucas, J. A., Younkin, L. H., Younkin, S. G. & Graff-Radford, N. R. Serum creatinine levels correlate with plasma amyloid beta protein. Alzheimer Dis. Assoc. Disord. 16, 187–190 (2002).
Fukumoto, H. et al. Age but not diagnosis is the main predictor of plasma amyloid β-protein levels. Arch. Neurol. 60, 958–964 (2003).
Fagan, A. M. et al. Cerebrospinal fluid tau/β-amyloid42 ratio as a prediction of cognitive decline in nondemented older adults. Arch. Neurol. 64, 343–349 (2007).
Pannee, J. et al. The amyloid-β degradation pattern in plasma — a possible tool for clinical trials in Alzheimer’s disease. Neurosci. Lett. 573, 7–12 (2014).
Lewczuk, P. et al. Amyloid beta peptides in plasma in early diagnosis of Alzheimer’s disease: a multicenter study with multiplexing. Exp. Neurol. 223, 366–370 (2010).
Roeben, B. et al. Association of plasma Abeta40 peptides, but not Abeta42, with coronary artery disease and diabetes mellitus. J. Alzheimers Dis. 52, 161–169 (2016).
Hilal, S. et al. Plasma amyloid-beta levels, cerebral small vessel disease, and cognition: the Rotterdam study. J. Alzheimers Dis. 60, 977–987 (2017).
Lopez, O. L. et al. Plasma amyloid levels and the risk of AD in normal subjects in the cardiovascular health study. Neurology 70, 1664–1671 (2008).
Lewczuk, P. et al. Cerebrospinal fluid and blood biomarkers for neurodegenerative dementias: an update of the consensus of the task force on biological markers in psychiatry of the world federation of societies of biological psychiatry. World J. Biol. Psychiatry 19, 244–328 (2018).
Tzen, K. Y. et al. Plasma Aβ but not tau is related to brain PiB retention in early Alzheimer’s disease. ACS Chem. Neurosci. 5, 830–836 (2014).
Zetterberg, H. et al. Plasma tau levels in Alzheimer’s disease. Alzheimers Res. Ther. 5, 9 (2013).
Mattsson, N. et al. Plasma tau in Alzheimer disease. Neurology 87, 1827–1835 (2016).
Mielke, M. M. et al. Association of plasma total tau level with cognitive decline and risk of mild cognitive impairment or dementia in the mayo clinic study on aging. JAMA Neurol. 74, 1073–1080 (2017).
Gisslén, M. et al. Plasma concentration of the neurofilament light protein (NFL) is a biomarker of CNS injury in HIV infection: a cross-sectional study. EBioMedicine 3, 135–140 (2016).
Kuhle, J. et al. Comparison of three analytical platforms for quantification of the neurofilament light chain in blood samples: ELISA, electrochemiluminescence immunoassay and Simoa. Clin. Chem. Lab. Med. 54, 1655–1661 (2016).
Rojas, J. C. et al. Plasma neurofilament light chain predicts progression in progressive supranuclear palsy. Ann. Clin. Transl Neurol. 3, 216–225 (2016).
Rohrer, J. D. et al. Serum neurofilament light chain protein is a measure of disease intensity in frontotemporal dementia. Neurology 87, 1329–1336 (2016).
Hansson, O. et al. Blood-based NfL: a biomarker for differential diagnosis of parkinsonian disorder. Neurology 88, 930–937 (2017).
Vassar, R. et al. Beta-secretase cleavage of Alzheimer’s amyloid precursor protein by the transmembrane aspartic protease BACE. Science 286, 735–741 (1999).
Wu, G. et al. Characterization of plasma β-secretase (BACE1) activity and soluble amyloid precursor proteins as potential biomarkers for Alzheimer’s disease. J. Neurosci. Res. 90, 2247–2258 (2012).
Shen, Y. et al. Increased plasma beta-secretase 1 may predict conversion to Alzheimer’s disease dementia in individuals with mild cognitive impairment. Biol. Psychiatry 83, 447–455 (2018).
Hye, A. et al. Plasma proteins predict conversion to dementia from prodromal disease. Alzheimers Dement. 10, 799–807.e2 (2014).
O’Bryant, S. E. et al. Validation of a serum screen for Alzheimer’s disease across assay platforms, species, and tissues. J. Alzheimers Dis. 42, 1325–1335 (2014).
Yu, S. et al. Serum protein-based profiles as novel biomarkers for the diagnosis of Alzheimer’s disease. Mol. Neurobiol. 55, 3999–4008 (2018).
Corso, G. et al. Serum amino acid profiles in normal subjects and in patients with or at risk of Alzheimer dementia. Dement Geriatr. Cogn. Dis. Extra 7, 143–159 (2017).
Keller, A. et al. Validating Alzheimer’s disease micro RNAs using next-generation sequencing. Alzheimers Dement. 12, 565–576 (2016).
Guo, R. et al. A 9-microRNA signature in serum serves as a noninvasive biomarker in early diagnosis of Alzheimer’s disease. J. Alzheimers Dis. 60, 1365–1377 (2017).
Anand, S. et al. Discovery and confirmation of diagnostic serum lipid biomarkers for Alzheimer’s disease using direct infusion mass spectrometry. J. Alzheimers Dis. 59, 277–290 (2017).
Lista, S., Faltraco, F. & Hampel, H. Biological and methodical challenges of blood-based proteomics in the field of neurological research. Prog. Neurobiol. 101–102, 18–34 (2013).
Kiddle, S. J., Voyle, N. & Dobson, R. A blood test for Alzheimer’s disease: progress, challenges and recommendations. J. Alzheimers Dis. 64, S289–S297 (2018).
Andreasson, U., Blennow, K. & Zetterberg, H. Update on ultrasensitive technologies to facilitate research on blood biomarkers for central nervous system disorders. Alzheimers Dement. (Amst.) 3, 98–102 (2016).
O’Bryant, S. E. et al. Guidelines for the standardization of preanalytic variables for blood-based biomarker studies in Alzheimer’s disease research. Alzheimers Dement. 11, 549–560 (2015). This article provides a summary of selected pre-analytical methodologies used in several international AD cohort studies and presents advanced guidelines and protocols for pre-analytical methods.
Jack, C. R. Jr et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology 87, 539–547 (2016).
Lista, S., Dubois, B. & Hampel, H. Paths to Alzheimer’s disease prevention: from modifiable risk factors to biomarker enrichment strategies. J. Nutr. Health Aging 19, 154–163 (2015).
Gupta, V. B., Sundaram, R. & Martins, R. N. Multiplex biomarkers in blood. Alzheimers Res. Ther. 5, 31 (2013).
Lista, S., Zetterberg, H., O’Bryant, S. E., Blennow, K. & Hampel, H. Evolving relevance of neuroproteomics in Alzheimer’s disease. Methods Mol. Biol. 1598, 101–115 (2017).
Brinkmalm, A. et al. Explorative and targeted neuroproteomics in Alzheimer’s disease. Biochim. Biophys. Acta 1854, 769–778 (2015).
Blennow, K. & Zetterberg, H. Understanding biomarkers of neurodegeneration: ultrasensitive detection techniques pave the way for mechanistic understanding. Nat. Med. 21, 217–219 (2015).
Robin, X. et al. Bioinformatics for protein biomarker panel classification: what is needed to bring biomarker panels into in vitro diagnostics? Expert Rev. Proteomics 6, 675–689 (2009).
Hilario, M. & Kalousis, A. Approaches to dimensionality reduction in proteomic biomarker studies. Brief Bioinform. 9, 102–118 (2008).
Hampel, H. et al. Advances in the therapy of Alzheimer’s disease: targeting amyloid beta and tau and perspectives for the future. Expert Rev. Neurother. 15, 83–105 (2015).
Broich, K., Weiergräber, M. & Hampel, H. Biomarkers in clinical trials for neurodegenerative diseases: regulatory perspectives and requirements. Prog. Neurobiol. 95, 498–500 (2011).
Nistico, G., Broich, K. & Hampel, H. Need for new guidelines for Alzheimer’s disease clinical trials. Eur. J. Neurodegener. Dis. 2, 181–186 (2013).
Collins, F. S. & Varmus, H. A new initiative on precision medicine. N. Engl. J. Med. 372, 793–795 (2015).
Dubois, B. et al. Cognitive and neuroimaging parameters and brain amyloidosis in individuals at risk of Alzheimer’s disease (INSIGHT-preAD): a longitudinal observational study. Lancet Neurol. 17, 335–346 (2018). This landmark manuscript focuses on the INSIGHT-preAD cohort.
Doecke, J. D. et al. Blood-based protein biomarkers for diagnosis of Alzheimer disease. Arch. Neurol. 69, 1318–1325 (2012).
Mapstone, M. et al. Plasma phospholipids identify antecedent memory impairment in older adults. Nat. Med. 20, 415–418 (2014).
Burnham, S. C. et al. A blood-based predictor for neocortical Aβ burden in Alzheimer’s disease: results from the AIBL study. Mol. Psychiatry 19, 519–526 (2014).
Kerr, N. L. HARKing: hypothesizing after the results are known. Pers. Soc. Psychol. Rev. 2, 196–217 (1998).
Robinson, S. M., Canavan, M. & O’Keeffe, S. T. Preferences of older people for early diagnosis and disclosure of Alzheimer’s disease (AD) before and after considering potential risks and benefits. Arch. Gerontol. Geriatr. 59, 607–612 (2014).
Ashton, N. J. et al. Blood protein predictors of brain amyloid for enrichment in clinical trials? Alzheimers Dement. (Amst.) 1, 48–60 (2015).
Aisen, P. S., Vellas, B. & Hampel, H. Moving towards early clinical trials for amyloid-targeted therapy in Alzheimer’s disease. Nat. Rev. Drug Discov. 12, 324 (2013).
Hampel, H. et al. Biomarkers for Alzheimer’s disease therapeutic trials. Prog. Neurobiol. 95, 579–593 (2011).
Vellas, B. et al. Designing drug trials for Alzheimer’s disease: what we have learned from the release of the phase III antibody trials: a report from the EU/US/CTAD task force. Alzheimers Dement. 9, 438–444 (2013).
Hood, L. & Flores, M. A personal view on systems medicine and the emergence of proactive P4 medicine: predictive, preventive, personalized and participatory. N. Biotechnol. 29, 613–624 (2012).
Gligorijević, V., Malod-Dognin, N. & Pržulj, N. Integrative methods for analyzing big data in precision medicine. Proteomics 16, 741–758 (2016).
Younesi, E. & Hofmann-Apitius, M. From integrative disease modeling to predictive, preventive, personalized and participatory (P4) medicine. EPMA J. 4, 23 (2013).
Hampel, H. et al. The cholinergic system in the pathophysiology and treatment of Alzheimer’s disease. Brain 141, 1917–1933 (2018).
Acknowledgements
The authors acknowledge the following employees of F. Hoffmann-La Roche Ltd (Basel, Switzerland) who attended the working group meeting, the discussions from which formed the basis of this Review: Barbara Schaeuble, Bruce Jordan, Chiaki Yoda, Christian Czech, Estelle Vester-Blokland and Hai Zhang. Maryline Simon (Roche Diagnostics International, Rotkreuz, Switzerland) and Tobias Bittner (Genentech, Basel, Switzerland) also contributed to the meeting. Editorial support, in the form of minute-taking during the group meetings and formatting of the manuscript before submission, was provided by Jennifer Smith of MediTech Media Ltd (funded by Roche Diagnostics International). H.H. is supported by the AXA Research Fund, the Fondation Partenariale Sorbonne Université and the Fondation pour la Recherche sur Alzheimer, Paris, France. The research leading to these results has received funding from the programme Investissements d’Avenir ANR-10-IAIHU-06 (Agence Nationale de la Recherche-10-IA and Agence Institut Hospitalo-Universitaire-6). This research benefited from the support of the Program PHOENIX led by the Sorbonne University Foundation and sponsored by the Fondation pour la Recherche sur Alzheimer.
Reviewer information
Nature Reviews Neurology thanks T. Leyhe, P. Lewczuk and the other anonymous reviewer for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
H.H. and K.B. provided the initial idea and outline of content for the manuscript. All authors contributed content and critically reviewed and edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
H.H. received personal fees from Roche Diagnostics International during the conduct of the study. He has also received lecture fees from Biogen and Roche; research grants from Pfizer, Avid and MSD Avenir (paid to his institution); travel funding from Functional Neuromodulation, Axovant, Eli Lilly and Company, Takeda and Zinfandel, GE Healthcare and Oryzon Genomics; and consultancy fees from Jung Diagnostics, Cytox, Axovant, Anavex, Takeda and Zinfandel, GE Healthcare, Oryzon Genomics and Functional Neuromodulation. H.H. participated in scientific advisory boards of Functional Neuromodulation, Axovant, Eli Lilly and Company, Cytox, GE Healthcare, Takeda and Zinfandel, Oryzon Genomics and Roche Diagnostics International. H.H. is a co-inventor on numerous patents relating to biomarker measurement but has received no royalties from these patents. S.E.O. declares personal fees from Roche Diagnostics International and grants from the US National Institute on Aging during the conduct of the study as well as personal fees from Cx Precision Medicine outside the submitted work. In addition, S.E.O. has three patents licensed to Cx Precision Medicine. J.L.M. declares personal fees from Roche Diagnostics International during the conduct of the study and personal fees from IBL International, Raman Health and Fujirebio outside the submitted work. H.Z. is a co-founder of Brain Biomarker Solutions in Gothenburg AB, a GU Ventures-based platform company at the University of Gothenburg, Sweden, and reports personal fees from Roche Diagnostics International during the conduct of the study. C.L.M. declares personal fees from Roche Diagnostics International during the conduct of the study. S.L. received lecture honoraria from Roche. S.J.K. reports personal fees from Roche Diagnostics International, grants from the Medical Research Council (UK) and National Institute for Health Research Biomedical Research Centre for Mental Health during the conduct of the study and grants from Eli Lilly and Company outside the submitted work. R.B. is a current employee and stockholder of Roche Diagnostics International. K.B. declares personal fees from Roche Diagnostics International during the conduct of the study and personal fees from Fujirebio Europe, IBL International, Roche Diagnostics, Eli Lilly and Company and Alzheon outside the submitted work. In addition, K.B. has a European Patent application (EP 16002379.2) pending and is co-founder of Brain Biomarker Solutions in Gothenburg AB.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
All of Us Research Program: https://allofus.nih.gov/
Annual Wellness Visit: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/AWV_Chart_ICN905706.pdf
Big Data Research and Development Initiative: https://obamawhitehouse.archives.gov/blog/2012/03/29/big-data-big-deal
Clinical Laboratory and Standards Institute: http://clsi.org/
UK Biobank: http://www.ukbiobank.ac.uk/about-biobank-uk/
Supplementary information
Glossary
- Sensitivity
-
Diagnostic sensitivity is the probability that a test result is positive when the disease is present.
- Subjective cognitive decline
-
A self-reported decline in cognition, undetected by standard neuropsychological tests.
- Receiver operating characteristic
-
(ROC). The ROC curve is a plot of sensitivity versus 1 − specificity for the different possible cut-off points of a diagnostic test. Accuracy of the diagnostic test is based on the area under the ROC curve; the closer the area under the ROC curve is to 1, the better the test.
- Positive predictive value
-
(PPV). The probability that a patient has the disease when the test result is positive.
- Negative predictive value
-
(NPV). The probability that a patient does not have the disease when the test result is negative.
- Context of use
-
(COU). A statement that describes the manner and purpose of use for the biomarker in drug development. The supporting data and analyses submitted with the biomarker qualification determine the acceptability of the qualified COU.
- A/T/N classification system
-
A classification system that uses three binary biomarker categories reflecting Alzheimer disease pathophysiology. ‘A’ refers to biomarkers of amyloid-β (Aβ) pathology (cerebrospinal fluid (CSF) Aβ1–42 or amyloid PET), ‘T’ refers to biomarkers of tau pathology (CSF hyperphosphorylated tau or tau PET) and ‘N’ refers to biomarkers of neurodegeneration or neuronal injury (CSF total tau 18F-FDG–PET or structural MRI).
- Specificity
-
Diagnostic specificity is the probability that a test result is negative when the disease is absent.
- Big data
-
A repository of many data sets generated by data-mining tools, including information obtained through systems-theory-based and knowledge-based approaches, and clinical records.
- Integrative disease modelling
-
A multidisciplinary approach to standardize, manage, integrate and interpret multiple sources of structured and unstructured quantitative and qualitative data across biological scales using computational models that assist decision-making for translation of patient-specific molecular mechanisms into tailored clinical applications.
Rights and permissions
About this article
Cite this article
Hampel, H., O’Bryant, S.E., Molinuevo, J.L. et al. Blood-based biomarkers for Alzheimer disease: mapping the road to the clinic. Nat Rev Neurol 14, 639–652 (2018). https://doi.org/10.1038/s41582-018-0079-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-018-0079-7
This article is cited by
-
Correlation analysis between smoke exposure and serum neurofilament light chain in adults: a cross-sectional study
BMC Public Health (2024)
-
Data-driven modelling of neurodegenerative disease progression: thinking outside the black box
Nature Reviews Neuroscience (2024)
-
Serum neurofilament light chain and inflammatory cytokines as biomarkers for early detection of mild cognitive impairment
Scientific Reports (2024)
-
Gold nanomaterials: important vectors in biosensing of breast cancer biomarkers
Analytical and Bioanalytical Chemistry (2024)
-
Determinants of Plasma Alzheimer’s Disease Biomarker Use by Primary Care Providers and Dementia Specialists
Journal of General Internal Medicine (2024)