Abstract
Polygenic risk scores (PRSs) have shown promise in predicting susceptibility to common diseases1,2,3. We estimated their added value in clinical risk prediction of five common diseases, using large-scale biobank data (FinnGen; n = 135,300) and the FINRISK study with clinical risk factors to test genome-wide PRSs for coronary heart disease, type 2 diabetes, atrial fibrillation, breast cancer and prostate cancer. We evaluated the lifetime risk at different PRS levels, and the impact on disease onset and on prediction together with clinical risk scores. Compared to having an average PRS, having a high PRS contributed 21% to 38% higher lifetime risk, and 4 to 9 years earlier disease onset. PRSs improved model discrimination over age and sex in type 2 diabetes, atrial fibrillation, breast cancer and prostate cancer, and over clinical risk in type 2 diabetes, breast cancer and prostate cancer. In all diseases, PRSs improved reclassification over clinical thresholds, with the largest net reclassification improvements for early-onset coronary heart disease, atrial fibrillation and prostate cancer. This study provides evidence for the additional value of PRSs in clinical disease prediction. The practical applications of polygenic risk information for stratified screening or for guiding lifestyle and medical interventions in the clinical setting remain to be defined in further studies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The FinnGen data may be accessed through Finnish Biobanks’ FinnBB portal (www.finbb.fi) and THL Biobank data may be accessed through THL Biobank (https://thl.fi/en/web/thl-biobank).
Code availability
The full genotyping and imputation protocol for FinnGen is described at https://doi.org/10.17504/protocols.io.nmndc5e.
References
Khera, A. V. et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat. Genet. 50, 1219–1224 (2018).
Mavaddat, N. et al. Polygenic risk scores for prediction of breast cancer and breast cancer subtypes. Am. J. Hum. Genet. 104, 21–34 (2019).
Seibert, T. M. et al. Polygenic hazard score to guide screening for aggressive prostate cancer: development and validation in large scale cohorts. Br. Med. J. 360, j5757 (2018).
Global Burden of Disease Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1789–1858 (2018).
Piepoli, M. F. et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 37, 2315–2381 (2016).
Lindbohm, J. V. et al. 5-year versus risk-category-specific screening intervals for cardiovascular disease prevention: a cohort study. Lancet Public Health 4, e189–e199 (2019).
Brentnall, A. R., Cuzick, J., Buist, D. S. M. & Bowles, E. J. A. Long-term accuracy of breast cancer risk assessment combining classic risk factors and breast density. JAMA Oncol. 4, e180174 (2018).
Wilson, B. J. et al. Systematic review: family history in risk assessment for common diseases. Ann. Intern. Med. 151, 878–885 (2009).
Visscher, P. M. et al. 10 years of GWAS discovery: biology, function, and translation. Am. J. Hum. Genet. 101, 5–22 (2017).
Torkamani, A., Wineinger, N. E. & Topol, E. The personal and clinical utility of polygenic risk scores. Nat. Rev. Genet. 19, 581–590 (2018).
Choudhury, P. P. et al. Comparative validation of breast cancer risk prediction models and projections for future risk stratification. J. Natl Cancer Inst. 112, 278–285 (2020).
Timpson, N. J., Greenwood, C. M. T., Soranzo, N., Lawson, D. J. & Richards, J. B. Genetic architecture: the shape of the genetic contribution to human traits and disease. Nat. Rev. Genet. 19, 110–124 (2018).
Chatterjee, N., Shi, J. & Garcia-Closas, M. Developing and evaluating polygenic risk prediction models for stratified disease prevention. Nat. Rev. Genet. 17, 392–406 (2016).
Abraham, G. et al. Genomic prediction of coronary heart disease. Eur. Heart J. 37, 3267–3278 (2016).
Goff, D. C. Jr et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129, S49–S73 (2014).
Alonso, A. et al. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J. Am. Heart Assoc. 2, e000102 (2013).
Mahajan, A. et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat. Genet. 50, 1505–1513 (2018).
Inouye, M. et al. Genomic risk prediction of coronary artery disease in 480,000 adults: implications for primary prevention. J. Am. Coll. Cardiol. 72, 1883–1893 (2018).
Lubitz, S. A. et al. Genetic risk prediction of atrial fibrillation. Circulation 135, 1311–1320 (2017).
Khera, A. V., Emdin, C. A. & Kathiresan, S. Genetic risk, lifestyle, and coronary artery disease. N. Engl. J. Med. 376, 1194–1195 (2017).
Natarajan, P. et al. Polygenic risk score identifies subgroup with higher burden of atherosclerosis and greater relative benefit from statin therapy in the primary prevention setting. Circulation 135, 2091–2101 (2017).
Mega, J. L. et al. Genetic risk, coronary heart disease events, and the clinical benefit of statin therapy: an analysis of primary and secondary prevention trials. Lancet 385, 2264–2271 (2015).
McCarthy, M. I. Painting a new picture of personalised medicine for diabetes. Diabetologia 60, 793–799 (2017).
Bapat, A., Anderson, C. D., Ellinor, P. T. & Lubitz, S. A. Genomic basis of atrial fibrillation. Heart 104, 201–206 (2018).
Average Number of New Cases Per Year and Age-Specific Incidence Rates per 100,000 Females, UK (Cancer Research UK, accessed 4 April 2019); https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer
Cancer Incidence, Mortality, Prevalence and Survival in the Nordic Countries Version 8.2 (26.03.2019) (NORDCAN, accessed 4 April 2019); http://www-dep.iarc.fr/NORDCAN/
Maas, P. et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncol. 2, 1295–1302 (2016).
Lee, A. et al. BOADICEA: a comprehensive breast cancer risk prediction model incorporating genetic and nongenetic risk factors. Genet. Med. 21, 1708–1718 (2019).
Martin, A. R. et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 51, 584–591 (2019).
Borodulin, K. et al. Cohort Profile: The National FINRISK Study. Int. J. Epidemiol. 47, 696–696i (2018).
Grundy, S. M. et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 73, 3168–3209 (2019).
American Diabetes Association 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care 42, S13–S28 (2019).
Lindstrom, J. & Tuomilehto, J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care 26, 725–731 (2003).
Terry, M. B. et al. 10-year performance of four models of breast cancer risk: a validation study. Lancet Oncol. 20, 504–517 (2019).
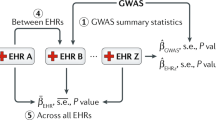
Kiiskinen, T. et al. Genomic prediction of alcohol-related morbidity and mortality. Transl. Psychiatry 10, 23 (2020).
Zhou, W. et al. Efficiently controlling for case–control imbalance and sample relatedness in large-scale genetic association studies. Nat. Genet. 50, 1335–1341 (2018).
Schumacher, F. R. et al. Association analyses of more than 140,000 men identify 63 new prostate cancer susceptibility loci. Nat. Genet. 50, 928–936 (2018).
Michailidou, K. et al. Association analysis identifies 65 new breast cancer risk loci. Nature 551, 92–94 (2017).
Nielsen, J. B. et al. Biobank-driven genomic discovery yields new insight into atrial fibrillation biology. Nat. Genet. 50, 1234–1239 (2018).
Vilhjalmsson, B. J. et al. Modeling linkage disequilibrium increases accuracy of polygenic risk scores. Am. J. Hum. Genet. 97, 576–592 (2015).
May, S. & Hosmer, D. W. A simplified method of calculating an overall goodness-of-fit test for the Cox proportional hazards model. Lifetime Data Anal. 4, 109–120 (1998).
Royston, P. & Parmar, M. K. Restricted mean survival time: an alternative to the hazard ratio for the design and analysis of randomized trials with a time-to-event outcome. BMC Med. Res. Methodol. 13, 152 (2013).
Acknowledgements
We thank S. Kivikko, H.-Y. Shen and U. Tuomainen for management assistance. The FINRISK analyses were conducted using the THL biobank permission for project BB2015_55.1. The FINRISK data used for the research were obtained from THL Biobank. For the Finnish Institute of Health and Welfare (THL)-driven FinnGen preparatory project (here called FinnGen), all patients and control subjects had provided informed consent for biobank research, based on the Finnish Biobank Act. Alternatively, older cohorts were based on study-specific consents and later transferred to the THL Biobank after approval by Valvira, the National Supervisory Authority for Welfare and Health. Recruitment protocols followed the biobank protocols approved by Valvira. The Ethics Review Board of the Hospital District of Helsinki and Uusimaa approved the FinnGen study protocol no. HUS/990/2017. The FinnGen preparatory project is approved by THL, approval number THL/2031/6.02.00/2017, amendments THL/341/6.02.00/2018, THL/2222/6.02.00/2018 and THL/283/6.02.00/2019. The following biobanks are acknowledged for collecting the FinnGen project samples: Auria Biobank (https://www.auria.fi/biopankki/en), THL Biobank (https://thl.fi/fi/web/thl-biopankki), Helsinki Biobank (https://www.terveyskyla.fi/helsinginbiopankki/en), Northern Finland Biobank Borealis (https://www.ppshp.fi/Tutkimus-ja-opetus/Biopankki), Finnish Clinical Biobank Tampere (https://www.tays.fi/en-US/Research_and_development/Finnish_Clinical_Biobank_Tampere), Biobank of Eastern Finland (https://ita-suomenbiopankki.fi/), Central Finland Biobank (https://www.ksshp.fi/fi-FI/Potilaalle/Biopankki), Finnish Red Cross Blood Service Biobank (https://www.bloodservice.fi/Research%20Projects/biobanking). We thank all study participants for their generous participation in FINRISK and FinnGen. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was supported by the Finnish Foundation for Cardiovascular Research (to S.R., V.S. and A.P.); Sigrid Jusélius Foundation (to S.R. and A.P.); University of Helsinki HiLIFE Fellow grants 2017–2020 (to S.R.); Academy of Finland Center of Excellence in Complex Disease Genetics (grant number 312062 to S.R., 312074 to A.P., 312075 to M.D.); Academy of Finland (grant number 285380 to S.R., 128650 to A.P.); The Finnish Innovation Fund Tekes (grant number 2273/31/2017 to E.W.); Horizon 2020 Research and Innovation Programme (grant number 667301 (COSYN) to A.P.); Ida Montin Foundation (to P.R.); Doctoral Programme in Population Health, University of Helsinki (to P.R.); and Emil Aaltonen Foundation (to P.R.). The FinnGen project is funded by two grants from Business Finland (HUS 4685/31/2016 and UH 4386/31/2016) and nine industry partners (AbbVie, AstraZeneca, Biogen, Celgene, Genentech, GSK, MSD, Pfizer and Sanofi). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
S.R. and N.M. conceived and designed the study. N.M. and P.R. carried out the statistical and computational analyses with advice from S.R., J.T.K., E.W., J.V.L., A.A.-O., M.D., V.S., B.M.N. and A.P. Quality control of the data was carried out by N.M., A.S.H., T.T.J.K., M.K., J.K. and P.P. The manuscript was written and revised by all of the co-authors. All co-authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.P. is a member of the Pfizer Genetics Scientific Advisory Panel. V.S. has participated in a conference trip sponsored by Novo Nordisk and received an honorarium for participating in an advisory board meeting (unrelated to the present study). V.S. also has research collaboration with Bayer Ltd (unrelated to the present study). B.M.N. is a member of the scientific advisory board at Deep Genomics and a consultant for Camp4 Therapeutics, Takeda Pharmaceutical and Biogen.
Additional information
Peer review information Kate Gao was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
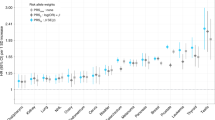
Extended Data Fig. 1 Investigating goodness-of-fit by polygenic risk score deciles in FinnGen (n = 135,300). Y-axis represents the expected and observed risks in each decile.
Goodness-of-fit test for the Cox proportional hazards model with R package survMisc, following the methodology in May & Hosmer (2004).41 Error bars for the expected counts represent the 95% confidence intervals.
Extended Data Fig. 2 With any breast cancer as the outcome in FinnGen (n = 135,300), adjusted survival curves for estrogen receptor-specific polygenic risk scores (PRS).
The PRS for any breast cancer showed high correlation with the estrogen receptor-positive PRS (Pearson correlation r = 0.93) and moderate correlation with estrogen receptor-negative PRS (r = 0.54).
Extended Data Fig. 3 Difference in age at disease onset estimates across polygenic risk score categories in FinnGen (n = 135,300).
CHD = coronary heart disease, AF = atrial fibrillation or flutter, T2D = type 2 diabetes. The estimands are restricted mean survival times (RMST) for age at onset, and the error bars represent their 95% confidence intervals. Incident and prevalent cases included. All tests were two-tailed.
Extended Data Fig. 4 Difference in age at disease onset estimates by sex, across polygenic risk score categories (FinnGen, n = 135,300).
CHD = coronary heart disease, AF = atrial fibrillation or flutter, T2D = type 2 diabetes. The estimands are restricted mean survival times (RMST) for age at onset, and the error bars represent their 95% confidence intervals. Incident and prevalent cases included. All tests were two-tailed.
Extended Data Fig. 5 Correlation between polygenic and clinical risk.
PRS = polygenic risk score, CHD = coronary heart disease, AF = atrial fibrillation or flutter, T2D = type 2 diabetes. Sample size in FINRISK (CHD, n = 20,165; AF, n = 21,030; T2D n = 10,561) and in FinnGen (breast cancer, n = 37,841; prostate cancer n = 48,851), using respective incident disease cases and controls. Correlation was assessed with Pearson correlation.
Extended Data Fig. 6 Adjusted survival curves in FINRISK, showing cumulative risk of incident disease in by polygenic risk score (PRS) categories.
The FINRISK cohorts (total n = 21,813) comprised of 2,197 incident cases of CHD, 1,431 cases of AF, 2,516 cases of T2D, 404 cases of breast cancer, and 444 cases of prostate cancer. Only incident cases included.
Supplementary information
Supplementary Information
Supplementary Tables 1–11.
Rights and permissions
About this article
Cite this article
Mars, N., Koskela, J.T., Ripatti, P. et al. Polygenic and clinical risk scores and their impact on age at onset and prediction of cardiometabolic diseases and common cancers. Nat Med 26, 549–557 (2020). https://doi.org/10.1038/s41591-020-0800-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-0800-0
This article is cited by
-
Predicting the presence of coronary plaques featuring high-risk characteristics using polygenic risk scores and targeted proteomics in patients with suspected coronary artery disease
Genome Medicine (2024)
-
The clinical relevance of a polygenic risk score for type 2 diabetes mellitus in the Korean population
Scientific Reports (2024)
-
Integration of polygenic and gut metagenomic risk prediction for common diseases
Nature Aging (2024)
-
Principles and methods for transferring polygenic risk scores across global populations
Nature Reviews Genetics (2024)
-
Integration of risk factor polygenic risk score with disease polygenic risk score for disease prediction
Communications Biology (2024)