Abstract
Cognitive stimulation has been proposed as a non-pharmacological intervention to be used in primary, secondary and tertiary prevention approaches for Alzheimer’s disease. A common familial Alzheimer’s disease transgenic model showed heightened levels of the stress hormone, corticosterone. When exposed to periodic enhanced cognitive stimulation, these animals demonstrated further heightened levels of corticosterone as well as increased Aβ pathology. Hence, Alzheimer’s disease may be associated with hypothalamic-pituitary-adrenal (HPA) axis dysfunction, causing stimulatory environments to become stress-inducing, leading to a glucocorticoid-pathology cycle contributing to further Aβ release and plaque formation. This finding suggests that stimulation-based interventions and local environments for people with Alzheimer’s disease need to be designed to minimise a stress response that may exacerbate brain pathology.
Similar content being viewed by others
Introduction
The ageing of the global population is accompanied by an increasing substantial social and financial impact of ageing-related diseases that cause dementia. Among elderly populations, Alzheimer’s disease (AD) is the most common cause of dementia1. Research has consistently demonstrated that the environment influences the brain both structurally and functionally over the lifetime2. In this respect, among modifiable factors that are associated with a reduced risk of developing dementia, is living a cognitively engaged life. Indeed, those who engage in high levels of cognitive activity have approximately half the risk of developing dementia than those who engage in low levels3. The cognitive reserve theory (CR) posits that a high-level of intellectual engagement over the life promotes strong and efficient neuronal connections that enables the neural system capacity to withstand a greater degree of pathological insult before clinical expression of the disease process emerges4.
In animal models, the building of cognitive reserve can be modelled experimentally through an environmental enrichment (EE) paradigm. EE describes the manipulation of an animals’ environment in order to generate novelty and complexity, and heighten cognitive, sensory, and physical stimulation5. EE applied in early-life has been found to boost cognitive performance in familial AD (FAD) transgenic mouse models to the level of healthy wildtypes (Wt). However, EE is reported to have a variable effect on Aβ pathological burden in transgenic mice expressing human FAD-related gene mutations, with reported decrease6,7,8, no change9,10,11, or increase12, 13 in Aβ load. Alternatively, it is possible that more complex, and novel stimulation may be required to buffer AD-related neuropathology3. Further, individuals are more likely to take up interventions to delay dementia onset in mid- to late-life, or even after the onset of early symptoms of dementia. In a previous investigation, we demonstrated some beneficial effects of mid-life EE on cognitive function, with no changes to Aβ neuropathological burden in FAD model mice14. Therefore, we sought to examine whether added periodic augmentation of more novel stimulation (EE+) in FAD animals from mid-life (6 months of age), would produce findings consistent with previous reports of reduced Aβ burden following EE6,7,8. In order to examine EE in mid to later-life, mice were raised in standard housing (minimal stimulation; SH) conditions until 6 months of age, and then randomly assigned to SH, environmental enrichment (EE) or enhanced environmental enrichment (EE+) conditions, where the animals remained until 12 months of age. Mice in EE lived in a larger cage to that of SH, and enrichment objects were present in the cage (wooden and plastic blocks of differing shapes and sizes, platforms, a ball, running wheel, and a mouse hut). Mice in the EE+ condition lived in EE, but were also exposed to a novel, larger cage three times per week that contained novel enrichment objects (e.g. steps, ladders, large running wheel, mazes, toys of different textures; changed weekly).
Results
Mid-life EE+ was associated with increased Aβ plaque pathology in the hippocampus
Following the 6-month intervention, when mice were 12 months of age, we hypothesised exposure to the EE+ intervention would potentially be associated with a reduction in Aβ plaque burden. We analysed fibrillar plaque load by Thioflavin-s (Fig. 1E) staining and by immunostaining of human unagreggated, oligomeric, and fibrillar forms of Aβ1-42 with the MOAB-2 antibody (Fig. 1F), in the neocortex and hippocampus of APP/PS1 mice. No significant alterations to Aβ load in the neocortex as a function of housing condition was detected for either Thioflavin-s or MOAB-2 labelled Aβ plaques (Fig. 1A,C). In contrast, there was a large (d = 1.08) and significant increase in hippocampal fibrillar Aβ plaque load in APP/PS1 mice exposed to the EE+ condition (Fig. 1B), and this effect was also detected for Aβ1-42 immunolabelling (Fig. 1D; d = 1.83).
Aβ plaque load in neocortex and hippocampus in APP/PS1 mice exposed to differential housing. (A) Thioflavin-S staining of fibrillar and dense core Aβ plaques demonstrated no significant difference in plaque load in neocortex between the housing groups, F(2, 19) = 0.78, p = 0.47. (B) A significant effect of housing was detected on Thioflavin-s plaque load in the hippocampus, F(2, 19) = 4.80, p = 0.02. Bonferroni adjusted post hoc tests revealed APP/PS1 mice housed in EE+ had higher hippocampal Aβ fibrillar plaque burden when compared to those in SH (p = 0.02). (C) MOAB-2 immunolabelling demonstrated no significant differences across housing groups in Aβ1-42 load, F(2, 18) = 0.65, p = 0.54. (D) A significant effect of housing condition was detected on hippocampal MOAB-2 load, F(2, 18) = 7.78, p = 0.005. Bonferroni adjusted post hoc tests showed EE+ mice to have a significantly higher hippocampal MOAB-2 load relative to mice in SH. SH (n = 9), EE (n = 7), EE+ (n = 6) *p < 0.05, **p < 0.01, ***p < 0.001. (E) Representative 10x Thioflavin-s staining in hippocampus of APP/PS1 mice for each housing group. (F) Representative 10x MOAB-2 staining in hippocampus of APP/PS1 mice for each housing group.
Mid-life EE+ was associated with increased Aβ 1-42 in neocortex
Next, we examined levels of soluble Aβ 1-42 in the neocortex and hippocampus, and found an overall significant effect of housing condition on Aβ 1-42 . APP/PS1 mice housed in EE+ showed a large (d = 1.89) and significant increase in Aβ 1-42 in neocortex, compared to mice from SH or EE (Fig. 2A). However, in contrast to the finding of an increase in Aβ plaque deposition in the hippocampus, this effect was not observed for Aβ 1-42 levels in the hippocampus (Fig. 2B). These data suggest that EE+ is associated with increases in Aβ levels in the neocortex, and increased deposition of Aβ in the hippocampus.
Aβ 1-42 levels in neocortex and hippocampus in APP/PS1 mice across differential housing conditions. (A) Overall, there was a significant effect of housing condition on cortical Aβ 1-42 levels, F(2, 12) = 10.41, p = 0.002. Follow-up post-hoc tests were performed with Bonferroni correction applied. The EE+ group had significantly higher cortical Aβ 1-42 compared with both SH (p = 0.003) and EE (p = 0.012). (B) No significant differences were detected in hippocampal Aβ 1-42 levels between housing conditions, F(2, 12) = 0.04, p = 0.96. SH (n = 5), EE (n = 5), EE+ (n = 5) *p < 0.05, **p < 0.01, ***p < 0.001.
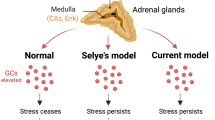
APP/PS1 mice demonstrated elevated levels of corticosterone
While our assumption had been that placing animals in an enhanced EE condition may have augmented cognitive and physical stimulation, it was also possible that this exposure had broader physiological effects that may have led to increased Aβ pathology, and that the FAD background also contributed to an unexpected reaction to the EE+ condition. Previous clinical studies have reported that people living with AD generally have higher blood-levels of the stress hormone, cortisol, when compared to healthy people15, 16. However, whether the disease process itself alters normal stress physiology, or whether stress increases vulnerability to developing AD, is unknown. It is widely accepted that stress induces activation of the hypothalamic-pituitary-adrenocortical (HPA) axis, which leads to a subsequent release of cortisol in humans, or corticosterone in rodents, from the adrenal cortex17, 18. Several studies, using experimental paradigms designed to induce stress, have demonstrated an accelerated onset, or faster rate of progression of AD, in FAD mouse models19,20,21,22,23. Such evidence led us to hypothesise that the novelty and complexity conferred by the EE+ condition, elevated stress levels, which may in turn have increased Aβ pathological burden in APP/PS1 mice in EE+ housing. We first compared levels of the stress hormone, corticosterone, between healthy control Wt and APP/PS1 mice from the SH condition, in order to determine whether the presence of the APP/PS1 transgene was associated with elevated corticosterone. Corticosterone levels in serum were significantly increased in 12-month old APP/PS1 mice compared to healthy Wt mice, which represented a large effect (d = 1.09) (Fig. 3). This finding supports the hypothesis of HPA axis dysfunction in AD.
Differential corticosterone levels according to genotype and housing condition. APP/PS1 mice in SH had significantly higher levels of corticosterone in blood serum compared to healthy Wt control mice at 12 months, t (24) = 2.34, p = 0.03. There was a significant interaction effect of genotype × housing on levels of corticosterone, F(2, 66) = 3.76, p = 0.03. In Wt mice, there was no significant effect of housing on corticosterone, F(2, 28) = 0.31, p = 0.74. Housing condition produced a significant effect on corticosterone levels in APP/PS1 mice, F(2, 38) = 4.8, p = 0.01. Bonferroni adjusted post hoc tests revealed EE+ mice had significantly higher corticosterone levels compared to SH (p = 0.02). Moreover, EE+ mice had higher corticosterone levels than mice housed in EE (p = 0.049), however, this was no longer significant when Bonferroni correction was applied (p = 0.057). SH Wt (n = 9), EE Wt (n = 12), EE+ Wt (n = 10); SH Tg (n = 17), EE Tg (n = 12), EE+ Tg (n = 12) *p < 0.05, **p < 0.01, ***p < 0.001.
Mid-life EE+ was associated with elevated corticosterone levels in APP/PS1 mice
Following the finding of elevated levels of corticosterone in APP/PS1 mice compared to Wt mice from SH, we included EE and EE+ conditions into the analysis. First, we found an overall significant interaction effect of genotype x housing on corticosterone levels. Due to the APP/PS1 mice demonstrating increased corticosterone levels, we analysed genotypes separately to investigate housing effects. In Wt mice, there was no significant housing condition effect on corticosterone levels. However, there was a significant and large effect of housing condition for APP/PS1 mice. While the APP/PS1 mice from SH exhibited increased corticosterone levels relative to Wts, APP/PS1 mice from EE+ showed further elevated corticosterone levels, being significantly higher compared to APP/PS1 mice from both the SH and EE conditions (d = 1.05) (Fig. 3).
Discussion
Our study has shown that periodic augmentation of EE conditions in APP/PS1 mice may have a deleterious effect on Aβ pathology, and this was associated with heightened levels of corticosterone, in a FAD model that already showed elevated stress hormone levels over Wt animals of a similar age. In contrast, sustained exposure to regular EE conditions did not affect corticosterone levels or amyloid pathology, indicating a potential capacity to habituate to long-term changes in the housing environment. While APP/PS1 animals housed in EE+ had increased Aβ pathology along with elevated corticosterone, no significant behavioural differences were detected on the Y maze test of spatial short-term memory, or the Barnes maze test of spatial learning and long-term memory relative to APP/PS1 mice housed in SH or EE (data not shown). The finding of increased pathological burden without cognitive dysfunction may offer support for the cognitive reserve theory4, however following up at later time points when neural resources are reduced, would be of interest.
Clinical studies have included reports of people living with AD to generally have higher levels of blood cortisol when compared to healthy people15, 16. Moreover, elevated levels of corticosterone has been reported previously in a FAD mouse model24, and Aβ accumulation has been associated with increased sensitivity of the HPA axis23. The present study confirms HPA axis dysfunction in an animal model of early AD. Several studies have demonstrated using experimental paradigms designed to induce acute stress (e.g. by restraint, loud noise, and bright light) an accelerated onset, or faster rate of progression of AD, in FAD mouse models19,20,21,22,23. However, in the current report, we found an association between the periodic stimulation condition and increased corticosterone. APP/PS1 mice display Aβ pathology from 4-5 months of age25, in the hippocampus and neocortex, and associated damage to synapses26, and the hippocampus directly regulates the HPA axis27,28,29. Green and colleagues30 speculated that, in AD, glucocorticoid feedback to the hippocampus may be lost, leading to an increased stress response. The increasing levels of glucocorticoid may further accelerate pathological processes, acting as a cycle of disease process progression. Notably, Wt mice did not show increased corticosterone levels after exposure to EE+, and, thus, were not stressed by the periodic stimulation of the EE+ condition. In contrast, FAD gene-linked deposition of Aβ in the hippocampus and synaptic damage in transgenic animals may lead to initial dysregulation of the HPA-axis, which contributed to a heightened stress response following periodic stimulation in the EE+ condition. Whereby, this periodic stimulation in EE+ may stimulate a harmful cascade, with subsequent increases in Aβ leading into an increased stress response to EE+, further increasing circulating corticosterone, and further Aβ deposition within the hippocampus.
The finding that elderly who enter a nursing home demonstrate more rapid cognitive decline compared to those who remain in the community31, together with the findings of this study, raise questions into the effect of novel environments for people with AD on disease progression. Moreover, the findings presented here bring into question cognitive interventions for the elderly, and for people living with AD in particular. An intervention aimed at delaying the progression of the clinical syndrome, dementia, is urgently needed given the rapidly increasing ageing population. As there are no current efficacious pharmacological treatments available, non-pharmacological interventions such as cognitive stimulation, training, and rehabilitation are of current interest. Such interventions have demonstrated various levels of efficacy, although modest sized effects are typically reported32. To our knowledge, the effects of cognitive intervention on stress in people living with AD has not been examined. Moving forward, this will be an important point of investigation, as cognitive interventions for people living with AD may have limited beneficial effect, and may potentially induce stress leading to an increased progression of disease processes. Likewise, given that Aβ pathology may be present in the brain many years before overt dementia symptomology33, it will be important to examine the role that stress may have in facilitating further pathology, and that primary and secondary prevention strategies that involve cognitive stimulation are designed to minimise elevated stress.
Methods
Animals and EE protocol
In the current study, we used a transgenic mouse model of AD that most closely resembles early-stage AD26. Male mice expressing chimeric mouse/human amyloid precursor protein (APP) and mutant human presenilin 1(PS1) on C57BL/6 background [B6.Cg-Tg (APPswe, PSEN1dE9) 85Dbo/J] (APP/PS1; Jankowsky et al.25 and littermate wildtype (Wt) control mice were housed in standard housing (SH) conditions (4-5 mice per 30 × 30 × 14 cm cage, ad libitum access to food and water, an igloo, one small wooden stick and one tissue) until 6 months of age. At 6 months, mice were randomly assigned to SH, EE, or EE+ conditions for the following 6 months. Mice assigned to the EE and EE+ housing conditions lived in a larger 60 × 30 × 14 cm cage with the contents of the SH cage and the addition of enrichment objects (wooden and plastic blocks of differing shapes and sizes, platforms, a ball, running wheel, and a mouse hut). The EE+ condition involved the mice being exposed to a larger (36 × 49 × 22 cm) cage three times per week that contained novel enrichment objects (changed weekly). Housing conditions were maintained until the 12-month end-point. All experimental procedures presented here were performed in accordance with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes, and approved by the University of Tasmania Animal Ethics Committee (A13253).
Tissue collection
Mice were terminally anaesthetized first with gas anaesthesia (isoflurane) followed by sodium pentobarbitone (100 mg/kg delivered intraperitoneally). For histological analysis, animals were perfused transcardially with 4% paraformaldehyde (PFA) in 0.1 M phosphate buffered saline (PBS pH 7.4). Post-mortem brains were transferred to 18% then 30% sucrose solutions overnight. Brains were cut on a cryostat (Leica CM 1850) in 40 μm coronal sections. APP/PS1 mice used for the quantification of human soluble Aβ 42 , were terminally anaesthetized as above, and perfused transcardially with PBS (0.1 M). Post-mortem brains were removed and the cortex and hippocampus were dissected and immediately frozen in liquid nitrogen. Cortex and hippocampal samples were stored at −80 °C for later analysis.
Aβ fibrillar plaque deposition
Thioflavin-S (Sigma-Aldrich) staining was performed in order to visualise fibrillar and dense-core Aβ plaques34, ten serial sections evenly spaced throughout the rostrocaudal axis of the brain from bregma 2.0–3.0 mm according to the stereotaxic mouse brain atlas35 were incubated in the solution (0.125% Thioflavine-S diluted in 60% absolute ethanol with 40% 0.01 M PBS) for 3 minutes at room temperature, and washed for 2 × 1 minute in 50% absolute ethanol and 50% 0.01 M PBS solution, followed by 3 × 10 minute washes in 0.01 M PBS. MOAB-2 immunostaining was performed in order to visualize human fibrillar, as well as unaggregated and oligomeric forms of Aβ42 14, 36. Ten serial sections evenly spaced throughout the rostrocaudal axis of the brain from bregma 2.0–3.0 mm were immunolabelled with the MOAB-2 antibody (1:2000; Novus Biologicals), and the labelling was visualized by inclubation in Alexa-fluorophore conjugated secondary antibody (1:1000; Molecular Probes, goat anti-mouse IgG2b-546). Sections were mounted using Dako fluorescent mounting medium.
Image acquisition
In order to determine Aβ plaque load in the neocortex and hippocampus, images were taken on a Leica DM fluorescence microscope on a 10x objective with NIS Elements imaging software. The left side of the cortex was imaged from the midline to the rhinal fissure from bregma 2.0–3.0 mm of 10 sections per animal. Images of the whole hippocampal formation were taken between bregma position −1.22 and −2.46 mm of 3–5 sections per animal. Aβ plaque load (percentage area Thioflavin-S positive) was calculated by random forest segmentation for one hemisphere of the neocortex and the whole hippocampal formation. Whereby, a custom plugin for ImageJ was applied to the images, which automatically segmented images as plaques or background pixels by random forest classification37. The percent area stained by Thioflavin-S in the neocortex and hippocampus was calculated by dividing the labelled area by the total area analysed.
Aβ42 ELISA
For the quantitation of human Aβ 1-42 , a sandwich antibody ELISA was performed according to the manufacturer’s instructions (KHB3441, Invitrogen). The right side of the neocortex and hippocampus were homogenized in RIPA buffer (Sigma) containing a protease (Roche diagnostics) and phosphatase inhibitor cocktail (AG Scientific). The samples were centrifuged for 15 minutes at 13000 RPM, rotated for a further 30 minutes, and centrifuged again at 4 °C for 15 minutes at 13000 RPM. The resulting supernatant was removed and stored at −80 °C for protein analysis. The protein concentrations of samples were determined using the Bradford assay. Duplicate neocortex and hippocampus samples from APP/PS1 mice (n = 5/group) were diluted in the buffer provided (1:50). Soluble human Aβ 1-42 levels were normalized to total protein levels and expressed as picogram of Aβ 1-42 content per milligram of total protein (pg/mg). Optical densities were read at 450 nm on a microplate reader (SpectraMax, Molecular Devices), and concentrations of Aβ 1-42 were determined by comparison to the standard curve using a 4-parameter algorithm.
Corticosterone ELISA
In order to determine if there were differences in levels of stress between the housing conditions and genotypes, blood was collected at time of perfusion by cardiac puncture, performed at the start of the dark period (3 p.m.). Duplicate serum samples were diluted at 1:100 in the buffer provided, and levels of serum corticosterone were measured by a commercial ELISA kit (ab108821; Abcam) according to manufacturer instructions. Optical densities were read at 450 nm on a microplate reader (SpectraMax, Molecular Devices), and concentrations of corticosterone were determined by comparison to the standard curve using a 4-parameter algorithm.
Statistical analysis
Statistical analyses were performed using independent t-test and two-way ANOVA using IBM SPSS (Version 20). A statistically significant two-way ANOVA was followed up by post hoc tests. Variables considered were genotype (Wt or Tg) and housing condition (SH, EE, or EE+). Values of p < 0.05 for differences between group means were classified as statistically significant. The magnitude of differences between the means were reported as Cohen’s d.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Barnes, D. & Yaffe, K. The Projected Impact of Risk Factor Reduction on Alzheimer’s Disease Prevalence. Lancet Neurol. 10, 819–828, doi:10.1016/S1474-4422 (2013).
Sale, A., Berardi, N. & Maffei, L. Enrich the environment to empower the brain. Trends in Neurosciences 32, 233–239, doi:10.1016/j.tins.2008.12.004 (2009).
Valenzuela, M. J. & Sachdev, P. Brain reserve and dementia: a systematic review. Psychol. Med. 36, 441–54, doi:10.1017/S0033291705006264 (2006).
Stern, Y. Cognitive reserve in ageing and Alzheimer’s disease. The Lancet Neurology 11, 1006–1012, doi:10.1016/S1474-4422(12)70191-6 (2012).
Nithianantharajah, J. & Hannan, A. J. Enriched environments, experience-dependent plasticity and disorders of the nervous system. Nat. Rev. Neurosci. 7, 697–709, doi:10.1038/nrn1970 (2006).
Lazarov, O. et al. Environmental enrichment reduces Aβ levels and amyloid deposition in transgenic mice. Cell 120, 701–713, doi:10.1016/j.cell.2005.01.015 (2005).
Costa, D. A. et al. Enrichment improves cognition in AD mice by amyloid-related and unrelated mechanisms. Neurobiol. Aging 28, 831–844, doi:10.1016/j.neurobiolaging.2006.04.009 (2007).
Herring, A. et al. Preventive and therapeutic types of environmental enrichment counteract beta amyloid pathology by different molecular mechanisms. Neurobiol. Dis. 42, 530–8, doi:10.1016/j.nbd.2011.03.007 (2011).
Arendash, G. W. et al. Environmental enrichment improves cognition in aged Alzheimer’s transgenic mice despite stable beta-amyloid deposition. Neuroreport 15, 1751–1754, doi:10.1097/01.wnr.0000137183.68847 (2004).
Wolf, S. A. et al. Cognitive and Physical Activity Differently Modulate Disease Progression in the Amyloid Precursor Protein (APP)-23 Model of Alzheimer’s Disease. Biol. Psychiatry 60, 1314–1323, doi:10.1016/j.biopsych.2006.04.004 (2006).
Cotel, M.-C., Jawhar, S., Christensen, D. Z., Bayer, T. A. & Wirths, O. Environmental enrichment fails to rescue working memory deficits, neuron loss, and neurogenesis in APP/PS1KI mice. Neurobiol. Aging 33, 96–107, doi:10.1016/j.neurobiolaging.2010.02.012 (2012).
Jankowsky, J. L. et al. Environmental enrichment mitigates cognitive deficits in a mouse model of Alzheimer’s disease. J. Neurosci. 25, 5217–24, doi:10.1523/JNEUROSCI.5080-04.2005 (2005).
Jankowsky, J. L., Xu, G., Fromholt, D., Gonzales, V. & Borchelt, D. R. Environmental enrichment exacerbates amyloid plaque formation in a transgenic mouse model of Alzheimer disease. J. Neuropathol. Exp. Neurol. 62, 1220–1227, doi:10.1093/jnen/62.12.1220 (2003).
Stuart, K. E. et al. Mid-life environmental enrichment increases synaptic density in CA1 in a mouse model of Abeta-associated pathology and positively influences synaptic and cognitive health in healthy ageing. J. Comp. Neurol., doi:10.1002/cne.24156 (2016).
Rasmuson, S. et al. Increased glucocorticoid production and altered cortisol metabolism in women with mild to moderate Alzheimer’s disease. Biol. Psychiatry 49, 547–552, doi:10.1016/S0006-3223(00)01015-5 (2001).
Csernansky, J. G. et al. Plasma Cortisol and Progression of Dementia in DAT Subjects. Am. J. Psychiatry 163, 2164–2169, doi:10.1176/appi.ajp.163.12.2164 (2006).
Nelson, D. H. Regulation of glucocorticoid release. Am. J. Med. 53, 590–594, doi:10.1016/0002-9343(72)90155-6 (1972).
Silverman, M. N. & Sternberg, E. M. Glucocorticoid regulation of inflammation and its functional correlates: From HPA axis to glucocorticoid receptor dysfunction. Annals of the New York Academy of Sciences 1261, 55–63, doi:10.1111/j.1749-6632.2012.06633.x (2012).
Dong, H. et al. Modulation of hippocampal cell proliferation, memory, and amyloid plaque deposition in APPsw (Tg2576) mutant mice by isolation stress. Neuroscience 127, 601–609, doi:10.1016/j.neuroscience.2004.05.040 (2004).
Jeong, Y. H. et al. Chronic stress accelerates learning and memory impairments and increases amyloid deposition in APPV717I-CT100 transgenic mice, an Alzheimer’s disease model. FASEB J. 20, 729–731, doi:10.1096/fj.05-4265fje (2006).
Rothman, S. M. et al. 3xTgAD mice exhibit altered behavior and elevated Aβ after chronic mild social stress. Neurobiol. Aging 33, 830.e1–830.e12, doi:10.1016/j.neurobiolaging.2011.07.005 (2012).
Baglietto-Vargas, D. et al. Short-term modern life-like stress exacerbates Aβ-pathology and synapse loss in 3xTg-AD mice. J. Neurochem. 134, 915–926, doi:10.1111/jnc.13195 (2015).
Carroll, J. C. et al. Chronic Stress Exacerbates Tau Pathology, Neurodegeneration, and Cognitive Performance through a Mechanism in a Transgenic Mouse Model of Tauopathy. J. Neurosci. 31, 14436–14449, doi:10.1523/JNEUROSCI.3836-11.2011 (2011).
Guo, Q., Zheng, H. & Justice, N. J. Central CRF system perturbation in an Alzheimer’s disease knockin mouse model. Neurobiol. Aging 33, 2678–2691, doi:10.1016/j.neurobiolaging.2012.01.002 (2012).
Jankowsky, J. L. et al. APP processing and amyloid deposition in mice haplo-insufficient for presenilin 1. Neurobiol. Aging 25, 885–92, doi:10.1016/j.neurobiolaging.2003.09.008 (2004).
Mitew, S., Kirkcaldie, M. T. K., Dickson, T. C. & Vickers, J. C. Altered synapses and gliotransmission in alzheimer’s disease and AD model mice. Neurobiol. Aging 34, 2341–2351, doi:10.1016/j.neurobiolaging.2013.04.010 (2013).
Herman, J. P. et al. Evidence for hippocampal regulation of neuroendocrine neurons of the hypothalamo-pituitary-adrenocortical axis. J. Neurosci. 9, 3072–82 (1989).
Jacobson, L. & Sapolsky, R. The role of the hippocampus in feedback regulation of the hypothalamic-pituitary-adrenocortical axis. Endocrine Reviews 12, 118–134, doi:10.1210/edrv-12-2-118 (1991).
Roozendaal, B. et al. Memory retrieval impairment induced by hippocampal CA3 lesions is blocked by adrenocortical suppression. Nat. Neurosci. 4, 1169–1171, doi:10.1038/nn766 (2001).
Green, K. N., Billings, L. M., Roozendaal, B., McGaugh, J. L. & LaFerla, F. M. Glucocorticoids increase amyloid-beta and tau pathology in a mouse model of Alzheimer’s disease. J. Neurosci. 26, 9047–9056, doi:10.1523/JNEUROSCI.2797-06.2006 (2006).
Gonzalez-Colaco Harmand, M. et al. Cognitive decline after entering a nursing home: A 22-year follow-up study of institutionalized and noninstitutionalized elderly people. J. Am. Med. Dir. Assoc. 15, 504–508, doi:10.1016/j.jamda.2014.02.006 (2014).
Choi, J. & Twamley, E. W. Cognitive rehabilitation therapies for Alzheimer’s disease: A review of methods to improve treatment engagement and self-efficacy. Neuropsychology Review 23, 48–62 (2013).
Braak, H. & Del Tredici, K. The pathological process underlying Alzheimer’s disease in individuals under thirty. Acta Neuropathol. 121, 171–181, doi:10.1007/s11065-013-9227-4 (2011).
Dickson, T. C. & Vickers, J. C. The morphological phenotype of β-amyloid plaques and associated neuritic changes in Alzheimer’s disease. Neuroscience 105, 99–107, doi:10.1016/S0306-4522(01)00169-5 (2001).
Paxinos, G. & Franklin, K. The Mouse Brain in Stereotaxic Coordinates, Compact | 978-0-12-374244-5 | Elsevier. The Mouse Brain in Stereotaxic Coordinates at https://www.elsevier.com/books/the-mouse-brain-in-stereotaxic-coordinates-compact/paxinos/978-0-12-374244-5 (Date of access:15/02/2016) (2008).
Collins, J. M., King, A. E., Woodhouse, A., Kirkcaldie, M. T. K. & Vickers, J. C. The effect of focal brain injury on beta-amyloid plaque deposition, inflammation and synapses in the APP/PS1 mouse model of Alzheimer’s disease. Exp. Neurol. 267, 219–29, doi:10.1016/j.expneurol.2015.02.034 (2015).
Sommer, C., Straehle, C., Kothe, U. & Hamprecht, F. A. Ilastik: Interactive learning and segmentation toolkit. In Proceedings - International Symposium on Biomedical Imaging 230–233, doi:10.1109/ISBI.2011.5872394 (2011).
Acknowledgements
The authors would like to thank and acknowledge Graeme McCormack, Justin Dittmann, John McManus, and Aidan O’Mara for technical assistance on this project. This study was funded by the J.O. and J.R. Wicking Trust (Equity Trustees). Mathew J. Summers reports personal fees from Eli Lily (Australia) Pty Ltd and from Novotech Pty Ltd, outside of the submitted work.
Author information
Authors and Affiliations
Contributions
K.E.S. contributed to the design of the sudy, wrote initial drafts of the manuscript and undertook the laboratory studies. C.M.F.-M. contributed to the ELISA studies and also to the design of experiments and writing of the manuscript. A.E.K. and J.C.V. contributed to the conceptualization of the project, design of the study and the writing of the manuscript. M.J.S. contributed to the analysis of the study findings and the writing of the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stuart, K.E., King, A.E., Fernandez-Martos, C.M. et al. Environmental novelty exacerbates stress hormones and Aβ pathology in an Alzheimer’s model. Sci Rep 7, 2764 (2017). https://doi.org/10.1038/s41598-017-03016-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03016-0
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.