Abstract
Deletions of the cell cycle control gene CDKN2A are described as progression markers of non-muscle invasive bladder cancer and to be associated with fibroblast growth factor 3 (FGFR3) mutations. The prognostic role of CDKN2A RNA expression in muscle invasive bladder cancer (MIBC) is under discussion. In 80 MIBC patients (m/f 60/20) who underwent radical cystectomy the expression of CDKN2A and FGFR3 was examined with qRT-PCR (test cohort). The MDA cohort (n = 57) and the TCGA cohort (n = 365) served for validation. The expression of drug target genes and TCGA molecular subtypes was correlated with CDKN2A expression. In the test cohort CDKN2Ahigh patients (n = 8; 10.0%) had a significantly shorter recurrence-free (p = 0.018) and disease-specific (p = 0.006) survival compared to the rest of the cohort. A similar stratification was seen in the validation cohorts (CDKN2Ahigh: n = 7, 12.3%, p = 0.001; n = 46, 12.6%, p = 0.011). In the TCGA cohort these patients had a comparably low expression of drug target genes. The expression of CDKN2A significantly differed among TGCA molecular subtypes. 71.7% of CDKN2Ahigh were TCGA basal squamous tumours but also show divergent molecular features compared to this group. In summary CDKN2A RNA expression-based risk stratification of MIBC allows the identification of a CDKN2Ahigh poor prognosis group with low expression of drug target genes.
Similar content being viewed by others
Introduction
For several decades radical cystectomy (RC) is the standard therapy of muscle invasive bladder cancer (MIBC). Yet, due to a high recurrence rate, 5-year overall survival (OS) of patients with locally advanced tumours is only around 50%1. In the hospital routine decisions on adjuvant, neoadjuvant and palliative medication still mainly rely on clinical parameters. Though deemed crucial in terms of risk stratification and identification of patients in need for a more aggressive treatment, molecular profiling for individual therapy decision-making is still in it’s infancy in MIBC2,3. Furthermore, expression data can give valuable information about drug target gene expression4,5,6.
In the light of bladder cancer initiation several frequent genetic aberrations have been identified. Papillary/non muscle-invasive and non-papillary/muscle-invasive bladder cancer are typically seen as two different molecular entities7. In both groups alterations of “forerunner genes” are seen as an initial event. Whilst in papillary tumours, genetic alterations are mainly restricted to these genes, high risk NMIBC and MIBC often show alterations of major tumour suppressor genes as RB1 or TP538,9.
Loss of heterozygosity (LOH) in the 9p region is one of this typical early events in the formation of bladder cancer and frequently occurs in non-invasive precursor lesions like hyperplasia, dysplasia or carcinoma in situ10,11,12,13. One of the genes found in this region is CDKN2A, which codes for the cell cycle control protein p16. LOH of CDKN2A and decreased expression of the p16 protein are mainly described as a predictor of progression in non muscle-invasive bladder cancer (NMIBC)14. Homozygous deletion of CDKN2A, is also associated with muscle invasion in FGFR3-mutated (fibroblast growth factor receptor 3) tumours15.
On the protein level a meta-analysis16, including data from 17 immunohistochemistry studies with 1032 subjects, investigated the p16 expression in various disease stages and found a significant association between a low expression of p16 and recurrence-free survival in patients with all stages of bladder cancer. When stratifying for T stages this correlation was markedly stronger for NMIBC, but was not found for MIBC (≥T2). The same was found for progression-free survival (PFS). The authors concluded that the p16 expression is affected by clinicopathologic stage and its relevance is mainly to be seen in NMIBC.
Another study found altered p16 protein expression, defined as either no expression of p16 or a very strong p16 expression, to be associated with a worse outcome of MIBC17. These results support a more complex role of CDKN2A and the p16 protein in MIBC.
We therefore aimed to stratify patients with MBIC according to their CDKN2A expression. Since immunohistochemistry is limited in case of quantification and sample comparison, RNA-based methods like qRT-PCR or next generation sequencing are robust alternatives for quantification and stratification of gene expression. The value of CDKN2A mRNA expression has not been systematically investigated in MIBC, yet, but qRT-PCR has already proved to be a valuable tool to determine CDKN2A copy number status18. The CDKN2A RNA-expression-based risk stratification was validated in the MDA and the TCGA cohort. Furthermore we reanalysed TCGA data to reveal correlations of CDKN2A with drug target gene expression and molecular subtypes.
Results
CDKN2A RNA expression allows risk stratification of MIBC patients
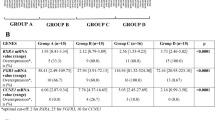
When stratifying for disease-specific death using the partition test, the test cohort of 80 patients with MIBC could be divided into two groups with different CDKN2A expression (CDKN2Ahigh with n = 8, 10.0%; CDKN2Alow with n = 72, 90.0%). Clinicopathologic data did not differ significantly between these groups (Table 1
).
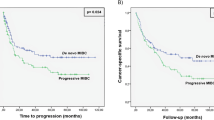
Kaplan-Meier analysis for recurrence-free survival (RFS, Fig. 1a) and disease-specific survival (DSS, Fig. 1b) showed significant differences (p = 0.018 and p = 0.006) between these groups, with CDKN2Ahigh having a worse prognosis (median RFS 16.3 months and median DSS 11.2 months) compared to patients with CDKN2Alow tumours (median RFS 74.2 months and median DSS 131.7 months).
By using the partition test in the MDA cohort of 57 bladder cancer patients a similar cut-off for CDKN2A expression could be defined. As in the test cohort, those patients with the highest CDKN2A expression (n = 7; 12.3%) had a worse prognosis (p = 0.001; median DSS 25.3 months, for CDKN2A median DSS was not reached; Fig. 2a).
When applying the partition test to the TCGA cohort, again a small group of patients with the highest CDKN2A expression (n = 46; 12.6%) with a poor prognosis could be identified (p = 0.011; Fig. 2b). The median overall survival (OS) of CDKN2Ahigh was 18.0 months, compared to 38.2 months in the CDKN2Alow group (n = 319; 87.4%). Clinicopathologic data did not differ significantly between the CDKN2A expression groups in the MDA and the TCGA cohort (Table 2 and Table 3
).
Further dissection of the bigger group of CDKN2Alow tumours in the test cohort and the TCGA cohort did not result in similar subgroup sizes, but yet resulted in different cut-offs with significant differences in prognosis, with patients with an intermediate expression of CDKN2A having a better prognosis as those with a low expression (Supplementary Figure 1).
Expression of drug target genes in dependence on CDKN2A expression
In the TCGA cohort there was a negative correlation between CDKN2A and FGFR3 in all MIBC (ρ = −0.406; p < 0.001). In the test cohort there was also a trend towards a negative correlation between FGFR3 and CDKN2A (ρ = −0.217, p = 0.053). Yet, inter-group comparison did not show a significant difference in FGFR3 expression between CDKN2Alow and CDKN2Ahigh tumours (p = 0493; Fig. 3a). In the TCGA cohort the FGFR3 expression differed significantly between the CDKN2A expression groups (p < 0.001; Fig. 3b).
Stratification for CDKN2A expression also showed a significantly lower expression of ESR2 in CDKN2Ahigh tumours (p < 0.001, Fig. 3c). For the other tested drug target genes (AR, ESR1, ERBB2, PDCD1, CD274 and CTLA4) no significant differences in the two CDKN2A expression groups were seen. Over all MIBC patients from the TCGA cohort AR was negatively correlated with CDKN2A expression (ρ = −0.183; p = 0.004) and PDCD1, CD274 and CTLA4 were positively correlated with CDKN2A expression (ρ = 0.176; p < 0.001; ρ = 0.327; p < 0.001; ρ = 0.171; p < 0.001). Detailed results are given in Supplementary Table 1.
CDKN2A CNV status, downstream target expression and molecular subtypes
In the TCGA cohort patients with CDKN2Alow expression frequently had CDKN2A deletions (38.9%% homozygous deletion, heterozygous deletions: 26.0%) in comparison to more balanced genotypes in the CDKN2Ahigh group (−1: 21.7%, balanced: 34.8%, +1: 43.5%, Supplementary Figure 2a). Chi2 test proved this difference to by significant (p < 0.001). Vice versa, upon stratification of CDKN2A expression for CDKN2A CNV there was also a significant difference between CNV groups (Kruskal-Wallis p < 0.001, Supplementary Figure 2b).
Supplementary Figure 3a illustrates the CDKN2A expression in the CDKN2A expression groups of the TCGA cohort. CDK4, despite being negatively regulated by CDKN2A, showed a slightly, but not significantly higher expression in CDKN2Ahigh (p < 0.139; Supplementary Figure 3b). RB1, which is regulated by CDK4, showed a significantly lower expression in CDKN2Ahigh (p < 0.001, Supplementary Figure 3c) and the downstream transcription factor gene E2F3 was significantly higher expressed in CDKN2Ahigh tumours (p < 0.001, Supplementary Figure 3d). In the complete cohort a positive correlation was observed between CDKN2A and CDK4 gene expression (ρ = 0.222, p < 0.001) and E2F3 gene expression (ρ = 0.212, p < 0.001) and a negative correlation between CDKN2A and RB1 ρ = −0.479 (p < 0.001).
When correlated with copy number status, there was a significant difference in the distribution of updated TCGA subtypes19 (Chi2 p = 0.016; Table 4 and Fig. 4a). Tumours with basal squamous and neuronal expression phenotype were overrepresented in the group of tumours with no deletion. Luminal tumours mainly had a homozygous deletion. Tumours from the basal squamous group on average showed the highest CDKN2A expression and tumours from the luminal group had a comparably low CDKN2A expression. Over all groups Kruskal-Wallis test showed a significantly different distribution, with 33 of 46 tumours (71.7%) in the CDKN2Ahigh group being classified as basal squamous (Fig. 4b).
(a) In the TCGA cohort the distribution of TCGA RNA-expression subtypes significantly differs according to CDKN2A copy number status (Chi2 0.016). (b) Vice versa there were significant differences in the CDKN2A expression in these subtypes (bas squam = basal squamous, lum = luminal, lum inf = luminal infiltrated, lum pap = luminal papillary, neur = neuronal). Of the analyzed, typically subtype defining, genes, KRT20, GATA3 and FOXA1 showed a differing expression in the CDKN2A expression groups (c–e). (*p < 0.05; **p < 0.01; ***p < 0.001).
When looking at specific genes, typically determining RNA expression subtypes, GATA3 (ρ = −0.162; p = 0.002) and FOXA1 (ρ = −0.299; p < 0.001) showed an inverse correlation with the CDKN2A expression. Both genes also showed a significantly lower expression in CDKN2Ahigh tumours compared to CDKN2Alow tumours (both p < 0.001; Fig. 4d,e). Furthermore KRT20 was significantly lower expressed in CDKN2Ahigh tumours (p = 0.028; Fig. 4c). Detailed results are given in Supplementary Table 2.
Discussion
Deletions of CDKN2A and the underexpression of p16, the protein coded by CDKN2A, are well-investigated molecular risk factors for tumour progression in NMIBC. Based on this, one could conclude that deletion or underexpression of CDKN2A/p16 is also an indicator of increased aggressiveness and worse prognosis in MIBC. Yet, some data point to a more complex situation in MIBC. For instance, gene expression studies have shown distinct RNA expression patterns for Ta tumours and MIBC, with T1 tumours showing either one or the other signature20. To more deeply investigate the role of CDKN2A expression in tumour prognosis and its association with drug target genes like FGFR3, we performed qRT-PCR expression profiling and reanalysis of existing CDKN2A and FGFR3 RNA expression data of MIBC after RC. Compared to immunohistochemistry studies of p16, RNA-testing with qRT-PCR has the advantages of a higher dynamic width and a higher sensitivity. Furthermore qRT-PCR testing allows an observer-independent interpretation of quantifiably results.
In the three analyzed cohorts the groups with the highest expression of CDKN2A (10.0–12.6% of the examined patients) were identified to have a worse prognosis compared to the remaining patients. This is controversial to previous assumptions derived from findings in NMIBC, where deletion of CDKN2A, typically going along with a lowered expression, is deemed as a marker for poor prognosis2,21,22.
However, already in 2004 it was shown that both a low and a high expression of the p16 protein can be a predictor of worse outcome after RC17. The overall prevalence of altered p16 protein expression was 54% of the analyzed tumours. The results of last-mentioned study show that both high and low expression of CDKN2A and p16, respectively, are associated with a worse outcome of MIBC patients. Though we could not find similar cut-off values in the different cohorts to distinguish between patients with low and intermediate expression of CDKN2A in the present study, patients with an intermediate expression seem to have the best prognosis, pointing to a diverse role of CDKN2A as prognosis marker in MIBC.
Functionally it is well known that impaired function or expression of p16, either due to CDKN2A deletion, mutation or hypermethylation, leads to cell cycle deregulation via overactivation of CDK4 and CDK6, which results in hyperphosphorylation of retinoblastoma protein (RB), the protein product of RB1. The subsequent liberation of E2F transcription factor family members mediates changes in gene expression, promoting the transition from G1 to S phase23. Besides this mechanism, loss of RB1 also results in tumour formation and progression24.
This close relation between CDKN2A/p16 and RB has been repeatedly described in urinary bladder cancer25,26. Yet, this does not intuitively explain why those MIBC with the highest CDKN2A expression show a poor prognosis. Sjödahl et al. reported two different genomic circuits operative in urothelial carcinomas: one defined by high FGFR3 and CCND1 expression, low CDKN2A expression, often associated with CDKN2A loss and the other one defined by E2F3 amplifications and overexpression, RB1 deletions and low expression and high CDKN2A/p16 expression27. Whilst the first circuit is mainly found in tumours termed urobasal A and urobasal B, the latter circuit was mainly associated with genomically unstable tumours28,29. These tumours also on the protein level typically showed no or low expression of KRT5 and KRT14, aberrant expression of KRT20 and a low expression of EGFR, but a high expression of ERBB2. According to this immunohistochemistry-based classification, genetically unstable tumours had a worse DSS compared to urobasal tumours, but better than squamous cancer cell-like tumours in a mixed population of NMIBC and MIBC27. Recent work from our own group has also shown high CDKN2A expression to be associated with shorter progress-free survival in T1 urothelial carcinoma30. The group of CDKN2Ahigh MIBC consistently identified in a proportion between 10.0 and 12.6% in all three datasets analyzed in the present study therefore might reflect a subgroup of genomically instable tumours, which account for 21.5% of advanced bladder cancers as described by Sjödahl et al.29. The reported overexpression of CDKN2A in genomically unstable tumours could be a sign of an in vain countermeasure to reduce cell cycle activity, which is deregulated due to other molecular aberrations.
Controversial to an association with the genomically unstable subtype is the fact, that 71,7% of the tumours with CDKN2Ahigh from the TCGA cohort are termed as basal squamous according to the 2017 TCGA publication19. Yet, this group (35% of MIBC in the TCGA cohort), also comprises 41% of tumors with CDKN2A deep deletions, meaning that CDKN2Ahigh tumours, which do not show any homozygous deletion of CDKN2A, are in part not a representative, but a highly selected subgroup of basal squamous tumours. In line with this and unlike reported for basal squamous tumors in the TCGA publication, CDKN2Ahigh tumours also do not show an elevation of PDCD1, CD274 and CTLA4 expression.
With regard to drug target gene expression, CDKN2A expression showed a negative correlation with FGFR3 expression in the TCGA cohort and a trend towards a negative correlation in the test cohort. The TCGA publication from 2014 proposed a correlation between CDKN2A deletion or underexpression and activating mutations of FGFR3 or FGFR3 overexpression4. They also reported an inverse correlation between CDKN2A and FGFR3 RNA expression. According to their mutational data they proposed three subtypes of bladder cancer: (A) focally amplified, (B) papillary CDKN2A-deficient and FGFR3-mutant and (C) TP53/cell-cycle-mutant. The study of Rebouissou and colleagues confirmed a high incidence of CDKN2A deletions (hemizygous 23.7%, homozygous 17.5%) and FGFR3 mutations (62.1%) in NMIBC15. In MIBC the rates of CDKN2A deletions were even higher (hemizygous 27.9%, homozygous 22.5%). Both in NMIBC and in MIBC there was a significant coincidence of CDKN2A deletions and activating mutations of FGFR3 and NMIBC tumours with this feature had an increased progression rate.
Due to their low FGFR3 expression, patients with CDKN2Ahigh tumours presumably do not seem to be suitable candidates for a therapy targeting FGFR3, whilst patients with a high FGFR3 expression might benefit from such an approach. The tyrosine kinases inhibitor Pazopanib is already approved for the treatment of advanced or metastatic kidney cancer and certain sarcoma entities, but there is only limited data about its application in MIBC: A small phase II trial on 19 unselected patients with metastatic bladder cancer reported a median PFS of only 1.9 months31. Another phase II study of 41 unselected patients with metastatic bladder cancer after failure of chemotherapy reported an overall initial response rate of 17%, but PFS and OS were poor32. However, there were also two patients with sustained long-term response. The RNA expression of FGFR3 in these tumours is not reported in the trial. Another group reported a case of a woman with a metastatic bladder cancer carrying an activating FGFR3 mutation33. This patient showed a durable remission of more than 6 months upon treatment with Pazopanib. In vitro results also suggest a synergistic effect of Pazopanib with Docetaxel in the treatment of bladder cancer cells34, pointing to a potential role of Pazopanib in combination therapy of cases with a suitable molecular profile. Besides Pazopanib, several other substances targeting FGFRs are currently under investigation35 and AZ12908010, AZD4547, PD173074, TKI-258/Dovitinib, SU5402 and BGJ-398 showed promising results in vitro36,37,38,39. Yet, clinical data is scarce and partially controversial: By systemic administration of Dovitinib biologically active concentrations could be consistently achieved in 13 patients with NMIBC40. However, long-term administration was not possible due to frequent toxicities. In another study Dovitinib showed a better tolerability but the antineoplastic effect in patients with FGFR3-mutated and FGFR3 wild type urothelial bladder cancer was poor41. For AZD4547 a case of long term response is described42. BGJ-398 showed an overall response rate of 36% in patients with pretreated advanced or metastatic urothelial carcinoma and was well tolerated43.
Besides a low FGFR3 expression, CDKN2Ahigh tumours also showed a low ESR2 expression and AR was negatively correlated with CDKN2A. CDKN2A expression was positively correlated with PDCD1, CD274 and CTLA4 expression. Yet, this did not result in a differential expression in CDKN2Ahigh tumours. In general the expression of the tested drug target genes was rather low in CDKN2Ahigh tumours. Therefore they may represent a high risk population both in terms of prognosis and limited treatment options.
Correlation of CDKN2A with the downstream markers CDK4, RB1 and E2F3 in the TCGA cohort also point to a more complex role of CDKN2A in the biology of MIBC: Unlike to be assumed by the known mechanism of CDKN2A-CDK4 interaction, with CDKN2A typically deactivating CDK4, the expression of both genes is not inversely but positively correlated. Furthermore, the tumour suppressor RB1, which is the subsequent gene in this signaling cascade44, is significantly downregulated upon increasing CDKN2A expression, indicating a more active cell cycle despite a high CDKN2A expression. Since the P16 protein mainly functionally regulates downstream targets via binding of CDK4 and CDK6, preventing them from interaction with cyclin D, which then results in reduced phosphorylation of RB1, phosphorylation data of RB1 would offer a more precise information about the pathway activity downstream of P16. Yet, there are currently no larger datasets analyzing RB1 phosphorylation status in bladder cancer.
The 2014 TCGA publication, comprising data from 131 MIBC, described four different subtypes based on RNA expression data4. These subtypes are mainly determined by the expression of luminal cytokeratins KRT8 and KRT18, basal cytokeratins KRT5, KRT6A, KRT6B, KRT6C, KRT15, the transcription factors GATA3 and FOXA1 and uroplakins. The updated 2017 publication19 suggests five molecular subtypes and implemented elements from other subtyping approaches8,9,45. We correlated the expression of CDKN2A with the aforementioned subtype determining genes. In the TCGA cohort there was a negative correlation with GATA3 and FOXA1 (ρ = −0.162 and −0.299), which are urothelial differentiation markers. For both genes also a significantly lower expression was seen in CDKN2Ahigh tumours. And also KRT20, typically associated with luminal tumours, showed a lower expression in this group. Fitting to this TCGA basal squamous tumours have the highest CDKN2A expression, whilst tumours from the luminal TCGA subtype group had an exclusively low expression.
Our results are limited by the fact that both our CDKN2A PCR assay and the RNA expression analysis in the MDA and the TCGA cohort do not discriminate between the CDKN2A transcripts. Therefore further analyses substratifying between the transcripts for p16 and p14 could add valuable information.
Furthermore the three analyzed cohorts are not directly comparable due to the different techniques (qRT-PCR in the test cohort, RNA expression microarray in the MDA cohort and RNAseq in the TCGA cohort) used for quantification and different data normalization protocols.
Taken together the CDKN2A RNA expression does not present as a continuum. On the one hand this indicates that quantifiably tools can be helpful to accurately deduce prognosis from CDKN2A RNA expression. On the other hand this also reflects a more complex biology behind the variation of CDKN2A expression in MIBC. In line with this, the expression of CDKN2A and p16 differs among molecular subtypes.
With the chosen approach we were able to identify a subgroup of patients with high CDKN2A expression with poor prognosis and comparably low expression of drug target genes. These tumours seem to partly correspond to both the basal squamous subtype described in the 2017 TCGA classification19 and the genomically unstable tumours described by Sjödahl et al.29. CDKN2A therefore might be a valuable component in the molecular risk stratification of MIBC and a potential indicator for targeted therapy decision-making.
Methods
Study population, RNA isolation and qRT-PCR
The test cohort consisted of 80 patients (mean age 66 years, range 46–93 years) with MIBC who underwent radical cystectomy at the Mannheim University Hospital Center between January 1998 and December 2006. Clinical and pathological data were retrospectively obtained from medical records (ethics approval 2016-814R-MA of the medical ethics committee II of the medical faculty Mannheim of the University of Heidelberg).
RNA extraction was performed as described before46. 10 μm sections from FFPE tissue samples were used for RNA extraction with a commercially available bead-based extraction method (XTRACT kit; STRATIFYER Molecular Pathology GmbH, Cologne, Germany). RNA was eluted with 100 μl elution buffer and stored at −80 °C until used.
The RNA expression of CDKN2A and FGFR3 was determined in relation to the housekeeping gene calmodulin 2 (CALM2) using 1-step qRT-PCR with validated TaqMan gene expression assays (STRATIFYER catalogue numbers: CDKN2A: MP672, FGFR3: MP599 and CALM2: MP501). Primers and labeled hydrolysis probes were selected using Primer Express® Software (Applied Biosystems/Life Technologies, Karlsruhe, Germany) and were controlled for single nucleotide polymorphisms. All primers, probes and amplicons were checked for their specificity against nucleotide databases at NCBI using Basic Local Alignment Search Tool (BLAST). Primers and probes were purchased from Eurogentec S.A. (Seraing, Belgium). For each primer/probe set, the amplification efficiency was tested, aiming to reach comparable efficiency of >90% (efficiency range from 97.7 to 99.7%). Primers and hydrolysis probes were diluted to 100 µM, using a stock solution with nuclease-free water (Life Technologies GmbH, Darmstadt, Germany). qRT-PCR was applied for the relative quantification of CDKN2A and FGFR3. For PCR, 0.5 µM of each primer and 0.25 µM of each probe were used. All quantitative reverse-transcription PCRs were performed in triplicates using the SuperScript® III Platinum® One-Step qRT-PCR kit (Invitrogen/Life Technologies, Darmstadt, Germany) according to the manufacturer’s instructions. Experiments were performed on a Stratagene Mx3005p (Agilent Technologies, Waldbronn, Germany) with 30 min at 50 °C and 2 min at 95 °C followed by 40 cycles of 15 s at 95 °C and 30 s at 60 °C. PCR amplification of each gene was performed in triplicates in each patient. Expression relative to CALM2 was determined using the 40-ΔCT method.
Reanalysis of existing datasets
57 patients with MIBC (mean age 66 years, range 41–89) from the MDA cohort45 and 365 patients with MIBC (mean age 68 years, range 34–90 years) identified from the TCGA (The Cancer Genome Atlas) project served for outcome validation. Illumina array RNA expression data of the MDA cohort was downloaded from Gene Expression Omnibus (GSE48276).
TCGA RNA sequencing expression data (z-score normalized data) of CDKN2A and the drug target genes FGFR3, AR, ESR1, ESR2, ERBB2, PDCD1 (PD1), CD274 (PDL1) and CTLA4 were downloaded from CBioPortal47. Furthermore the expression of TCGA molecular subtype determining genes KRT5, KRT6A, KRT6B, KRT6C, KRT8, KRT14, KRT18, KRT20, UPK1A, UPK1B, UPK2, UPK3A, UPK3B, GATA3 and FOXA1, of the CDKN2A downstream target genes CDK4 and RB1, the copy number variation (CNV) data of CDKN2A and the annotated updated TCGA RNA expression subtypes19 were extracted.
Statistics
Statistical analyses were performed using SAS JMP version 11.0 (SAS Institute, Cary, NC, USA) and Graphpad PRISM (Version 7.0; Graph Pad Software Inc., La Jolla, CA, USA). Cut-Off definitions were done by partitioning tests for decision trees to determine different CDKN2A expression groups. Student’s t-test and Chi2 test were used to compare for differences in the distribution of clinical parameters, TCGA subtypes and CDKN2A CNV data between the CDKN2A expression groups.
Kaplan Meier analyses were performed for DSS and RFS in the test cohort and for DSS and OS in the validation cohorts and were tested for significance using Log-Rank test.
Both in the test cohort and in the TCGA cohort CDKN2A expression was correlated with FGFR3 expression using Spearman correlation. In the TCGA cohort CDKN2A expression was also correlated with the expression of AR, ESR1, ESR2, ERBB2, PDCD1, CD274, CTLA4, KRT5, KRT6A, KRT6B, KRT6C, KRT8, KRT14, KRT18, KRT20, UPK1A, UPK1B, UPK2, UPK3A, UPK3B, GATA3, FOXA1, CDK4, RB1, E2F2 and KI67.
Student’s t-test was used to test for differences in gene expression in the CDKN2A expression groups in the test cohort and the TCGA cohort. For the analysis of CDKN2A expression according to CDKN2A copy number status and RNA-expression subtypes Kruskal-Wallis test with post hoc Dunn’s test for multiple comparisons was performed in the TCGA cohort. Graphs were designed with Graphpad Prism. P-values < 0.05 were deemed statistically significant.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Due to its retrospective character, for this type of study formal consent is not required.
References
Yafi, F. A. et al. Contemporary outcomes of 2287 patients with bladder cancer who were treated with radical cystectomy: a Canadian multicentre experience. BJU Int. 108, 539–545 (2011).
Kojima, T., Kawai, K., Miyazaki, J. & Nishiyama, H. Biomarkers for precision medicine in bladder cancer. Int. J. Clin. Oncol. https://doi.org/10.1007/s10147-016-1068-8 (2016).
McConkey, D. J., Choi, W. & Dinney, C. P. N. Genetic subtypes of invasive bladder cancer. Curr. Opin. Urol. 25, 449–458 (2015).
Cancer Genome Atlas Research Network. Comprehensive molecular characterization of urothelial bladder carcinoma. Nature 507, 315–322 (2014).
Mitra, A. P. & Lerner, S. P. Potential role for targeted therapy in muscle-invasive bladder cancer: lessons from the cancer genome atlas and beyond. Urol. Clin. North Am. 42, 201–215, viii (2015).
Carneiro, B. A. et al. Emerging therapeutic targets in bladder cancer. Cancer Treat. Rev. 41, 170–178 (2015).
McConkey, D. J. et al. Molecular genetics of bladder cancer: Emerging mechanisms of tumor initiation and progression. Urol. Oncol. 28, 429–440 (2010).
Hedegaard, J. et al. Comprehensive Transcriptional Analysis of Early-Stage Urothelial Carcinoma. Cancer Cell 30, 27–42 (2016).
Choi, W. et al. Genetic Alterations in the Molecular Subtypes of Bladder Cancer: Illustration in the Cancer Genome Atlas Dataset. Eur. Urol. https://doi.org/10.1016/j.eururo.2017.03.010 (2017).
Tsai, Y. C. et al. Allelic losses of chromosomes 9, 11, and 17 in human bladder cancer. Cancer Res. 50, 44–47 (1990).
Hartmann, A. et al. Occurrence of chromosome 9 and p53 alterations in multifocal dysplasia and carcinoma in situ of human urinary bladder. Cancer Res. 62, 809–818 (2002).
Obermann, E. C. et al. Frequent genetic alterations in flat urothelial hyperplasias and concomitant papillary bladder cancer as detected by CGH, LOH, and FISH analyses. J. Pathol. 199, 50–57 (2003).
Hartmann, A. et al. Frequent genetic alterations in simple urothelial hyperplasias of the bladder in patients with papillary urothelial carcinoma. Am. J. Pathol. 154, 721–727 (1999).
Bartoletti, R. et al. Loss of P16 expression and chromosome 9p21 LOH in predicting outcome of patients affected by superficial bladder cancer. J. Surg. Res. 143, 422–427 (2007).
Rebouissou, S. et al. CDKN2A homozygous deletion is associated with muscle invasion in FGFR3-mutated urothelial bladder carcinoma. J. Pathol. 227, 315–324 (2012).
Gan, X. et al. Prognostic and Clinicopathological Significance of Downregulated p16 Expression in Patients with Bladder Cancer: A Systematic Review and Meta-Analysis. Dis. Markers 2016, 5259602 (2016).
Shariat, S. F. et al. p53, p21, pRB, and p16 expression predict clinical outcome in cystectomy with bladder cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 22, 1014–1024 (2004).
Aveyard, J. S. & Knowles, M. A. Measurement of relative copy number of CDKN2A/ARF and CDKN2B in bladder cancer by real-time quantitative PCR and multiplex ligation-dependent probe amplification. J. Mol. Diagn. JMD 6, 356–365 (2004).
Robertson, A. G. et al. Comprehensive Molecular Characterization of Muscle-Invasive Bladder. Cancer. Cell 171, 540–556.e25 (2017).
Lindgren, D. et al. Combined gene expression and genomic profiling define two intrinsic molecular subtypes of urothelial carcinoma and gene signatures for molecular grading and outcome. Cancer Res. 70, 3463–3472 (2010).
Downes, M. R. et al. Analysis of papillary urothelial carcinomas of the bladder with grade heterogeneity: supportive evidence for an early role of CDKN2A deletions in the FGFR3 pathway. Histopathology 70, 281–289 (2017).
Gallucci, M. et al. Status of the p53, p16, RB1, and HER-2 genes and chromosomes 3, 7, 9, and 17 in advanced bladder cancer: correlation with adjacent mucosa and pathological parameters. J. Clin. Pathol. 58, 367–371 (2005).
Rayess, H., Wang, M. B. & Srivatsan, E. S. Cellular senescence and tumor suppressor gene p16. Int. J. Cancer 130, 1715–1725 (2012).
Di Fiore, R., D’Anneo, A., Tesoriere, G. & Vento, R. RB1 in cancer: different mechanisms of RB1 inactivation and alterations of pRb pathway in tumorigenesis. J. Cell. Physiol. 228, 1676–1687 (2013).
Benedict, W. F. et al. Level of retinoblastoma protein expression correlates with p16 (MTS-1/INK4A/CDKN2) status in bladder cancer. Oncogene 18, 1197–1203 (1999).
Mizuarai, S. et al. Expression ratio of CCND1 to CDKN2A mRNA predicts RB1 status of cultured cancer cell lines and clinical tumor samples. Mol. Cancer 10, 31 (2011).
Sjödahl, G. et al. Toward a molecular pathologic classification of urothelial carcinoma. Am. J. Pathol. 183, 681–691 (2013).
Lerner, S. P. et al. Bladder Cancer Molecular Taxonomy: Summary from a Consensus Meeting. Bladder Cancer Amst. Neth. 2, 37–47 (2016).
Sjödahl, G., Eriksson, P., Liedberg, F. & Höglund, M. Molecular classification of urothelial carcinoma: global mRNA classification versus tumour-cell phenotype classification. J. Pathol. 242, 113–125 (2017).
Breyer, J. et al. High CDKN2A/p16 and Low FGFR3 Expression Predict Progressive Potential of Stage pT1 Urothelial Bladder Carcinoma. Clin. Genitourin. Cancer, https://doi.org/10.1016/j.clgc.2018.01.009 (2018).
Pili, R. et al. A phase II safety and efficacy study of the vascular endothelial growth factor receptor tyrosine kinase inhibitor pazopanib in patients with metastatic urothelial cancer. Clin. Genitourin. Cancer 11, 477–483 (2013).
Pinciroli, P. et al. Molecular Signature of Response to Pazopanib Salvage Therapy for Urothelial Carcinoma. Clin. Genitourin. Cancer 14, e81–90 (2016).
Palma, N., Morris, J. C., Ali, S. M., Ross, J. S. & Pal, S. K. Exceptional Response to Pazopanib in a Patient with Urothelial Carcinoma Harboring FGFR3 Activating Mutation and Amplification. Eur. Urol. 68, 168–170 (2015).
Li, Y., Yang, X., Su, L.-J. & Flaig, T. W. Pazopanib synergizes with docetaxel in the treatment of bladder cancer cells. Urology 78, 233.e7–13 (2011).
Patani, H. et al. Landscape of activating cancer mutations in FGFR kinases and their differential responses to inhibitors in clinical use. Oncotarget 7, 24252–24268 (2016).
He, Y. et al. Daidzein exerts anti-tumor activity against bladder cancer cells via inhibition of FGFR3 pathway. Neoplasma 63, 523–531 (2016).
Lamont, F. R. et al. Small molecule FGF receptor inhibitors block FGFR-dependent urothelial carcinoma growth in vitro and in vivo. Br. J. Cancer 104, 75–82 (2011).
Chell, V. et al. Tumour cell responses to new fibroblast growth factor receptor tyrosine kinase inhibitors and identification of a gatekeeper mutation in FGFR3 as a mechanism of acquired resistance. Oncogene 32, 3059–3070 (2013).
Cheng, T. et al. Fibroblast growth factor receptors-1 and -3 play distinct roles in the regulation of bladder cancer growth and metastasis: implications for therapeutic targeting. PloS One 8, e57284 (2013).
Hahn, N. M. et al. A Phase II Trial of Dovitinib in BCG-Unresponsive Urothelial Carcinoma with FGFR3 Mutations or Overexpression: Hoosier Cancer Research Network Trial HCRN 12–157. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. https://doi.org/10.1158/1078-0432.CCR-16-2267 (2016).
Milowsky, M. I. et al. Phase 2 trial of dovitinib in patients with progressive FGFR3-mutated or FGFR3 wild-type advanced urothelial carcinoma. Eur. J. Cancer Oxf. Engl. 1990 50, 3145–3152 (2014).
Rodriguez-Vida, A. et al. Complexity of FGFR signalling in metastatic urothelial cancer. J. Hematol. Oncol.J Hematol Oncol 8, 119 (2015).
Pal, S. K. et al. Efficacy of BGJ398, a fibroblast growth factor receptor (FGFR) 1-3 inhibitor, in patients (pts) with previously treated advanced/metastatic urothelial carcinoma (mUC) with FGFR3 alterations. J. Clin. Oncol. 34 (2016).
Nagata, M., Muto, S. & Horie, S. Molecular Biomarkers in Bladder Cancer: Novel Potential Indicators of Prognosis and Treatment Outcomes. Dis. Markers 2016, 8205836 (2016).
Choi, W. et al. Identification of distinct basal and luminal subtypes of muscle-invasive bladder cancer with different sensitivities to frontline chemotherapy. Cancer Cell 25, 152–165 (2014).
Kriegmair, M. C. et al. Expression of the p53 Inhibitors MDM2 and MDM4 as Outcome Predictor in Muscle-invasive Bladder Cancer. Anticancer Res. 36, 5205–5213 (2016).
Cerami, E. et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404 (2012).
Acknowledgements
All authors are part of the BRIDGE (Bladder Cancer Research Initiative for Drug Targets Germany) Consortium e.V, on behalf of which the manuscript was submitted. We would like to thank Stefanie Herlein (Institute of Pathology, University of Erlangen-Nuremberg, Erlangen, Germany), Elke Veltrup and Silke Claas (STRATIFYER Molecular Pathology GmbH, Köln, Germany) for excellent technical support. We acknowledge financial support by Deutsche Forschungsgemeinschaft within the funding programme Open Access Publishing, by the Baden-Württemberg Ministry of Science, Research and the Arts and by Ruprecht-Karls-Universität Heidelberg.
Author information
Authors and Affiliations
Contributions
R.S., W.O., A.H., C.B., R.M.W. and P.E. planned the study and the experiments. T.S.W., C.A.W. and P.E. assembled the test cohort. C.A.W., S.B., R.S., M.E. and A.H. performed pathologic evaluation of tissue sections. R.M.W. performed PCR analyses. T.S.W., A.H., R.M.W. and P.E. performed PCR data analysis. T.S.W., A.H., R.M.W. and P.E. performed analyses of the TCGA cohort. T.S.W., J.B., A.H. and P.E. wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Worst, T.S., Weis, CA., Stöhr, R. et al. CDKN2A as transcriptomic marker for muscle-invasive bladder cancer risk stratification and therapy decision-making. Sci Rep 8, 14383 (2018). https://doi.org/10.1038/s41598-018-32569-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-32569-x
Keywords
This article is cited by
-
FISH analysis reveals CDKN2A and IFNA14 co-deletion is heterogeneous and is a prominent feature of glioblastoma
Brain Tumor Pathology (2024)
-
Identification and verification of a novel anoikis-related gene signature with prognostic significance in clear cell renal cell carcinoma
Journal of Cancer Research and Clinical Oncology (2023)
-
Increased mRNA expression of CDKN2A is a transcriptomic marker of clinically aggressive meningiomas
Acta Neuropathologica (2023)
-
Identification and validation of EMT-immune-related prognostic biomarkers CDKN2A, CMTM8 and ILK in colon cancer
BMC Gastroenterology (2022)
-
The prognostic significance of CDKN2A homozygous deletion in IDH-mutant lower-grade glioma and glioblastoma: a systematic review of the contemporary literature
Journal of Neuro-Oncology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.