Abstract
The purpose of this cross-sectional retrospective study was to determine the relationship between the retinal displacements and the retinal thickness in eyes with epiretinal membrane (ERM) after vitrectomy with internal limiting membrane (ILM) peeling. To accomplish this, we measured the retinal thickness using optical coherence tomography (OCT) and the retinal displacement using OCT angiography to obtain 3 mm × 3 mm en face images before, and 2, 4, and 8 weeks following the surgery from 20 eyes of 20 patients. The distance between the retinal vessel bifurcations and the fovea was significantly displaced centrifugally and asymmetrically in the 4 quadrants postoperatively (P < 0.001). The foveal avascular zone (FAZ) was significantly enlarged, and the central foveal thickness (CFT) and the inner nuclear layer (INL) thickness were significantly thinner postoperatively. The displacements were significantly correlated with the changes in the FAZ area (r = 0.717, P < 0.001), the CFT (r = − 0.702, P < 0.001), and the INL thickness (r = − 0.702, P < 0.001). In conclusion, the distance between the retinal bifurcations and the fovea was asymmetrically expanded after the surgery and was significantly correlated with the morphological changes. These results indicate that a horizontal macular contraction is correlated with vertical retinal contraction in the eyes with an ERM.
Similar content being viewed by others
Introduction
An idiopathic epiretinal membrane (ERM) is a relatively common retinochoroidal disorder in older individuals1,2, and it can cause an inner retinal displacement of the macula area and a disruption of the foveal structure3. These alterations cause traction on the retina in the macular area which can lead to visual dysfunction and metamorphopsia. Vitrectomy and removal of the ERM with or without internal limiting membrane (ILM) peeling is used to release the traction and is effective in improving the visual dysfunction, metamorphopsia, and visual acuity4,5,6. Thus, it is important to know how the retina in the macular area is displaced in more detail after the surgery because the displacement will affect the visual function.
Optical coherence tomography (OCT) enables clinicians to obtain information of the microstructures of the fovea, and earlier studies have reported that the retinal layer at the fovea is thickened and the outer retinal layers are disrupted in eyes with an ERM7,8,9. The integrity of the outer retinal layers is important for vision in retinochoroidal disorders, and their alterations have been evaluated10,11,12. However, there have been only a few reports on the changes of the inner retinal layers in eyes with ERM after surgery13. This is important because the integrity of the inner retina is a major determinant of the visual dysfunctions in eyes with an ERM.
OCT angiography (OCTA) is a noninvasive and safe technique that can obtain images of the microvasculature of the retina and the choroid. OCTA has enabled clinicians to investigate the retinal vasculature in situ repeatedly in short intervals14,15. The displacements of the inner retina can be evaluated using the superficial OCTA en face images of the retina before and after surgery16. Thus, OCTA is a suitable method for evaluating whether there is a displacement of the inner retina postoperatively. Akahori et al. evaluated the displacement of the inner retina after surgery in eyes with a macular hole16. However, there has not been a study that investigated the displacement of the retina after vitrectomy that removed an ERM.
Thus, the purpose of this study was to determine the relationship between the displacements of the inner retina and the retinal thicknesses in eyes with an ERM after vitrectomy with ILM peeling. To accomplish this, the superficial foveal avascular zone (FAZ) and the displacement of the retina were measured in the OCTA images, and the retinal thickness including the central foveal thickness (CFT) was measured in the spectral-domain OCT (SD-OCT) B scan images of eyes with an ERM before and after its removal. In addition, the relationships between the values determined by OCTA and SD-OCT were evaluated after vitrectomy with ILM peeling for the removal of an ERM.
Methods
Subjects
We reviewed the medical records of all patients with a unilateral, idiopathic ERM who had undergone vitrectomy with ILM peeling at the Nagoya University Hospital from December 2016 to March 2019. All of the patients had undergone comprehensive ophthalmic examinations. Additionally, OCTA and SD-OCT (Spectralis®, Heidelberg Engineering, Heidelberg, Germany) images were obtained before, and 2, 4, and 8 weeks following the surgery. The size and the location of the ERM and ILM peeling were determined from the videos recorded during the surgery. Eyes with severe cataract, macular diseases, history of other ocular diseases, and high myopia of > − 5 diopters (D) were excluded.
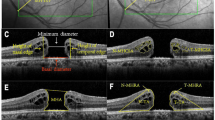
Measurements using optical coherence tomographic images
We analyzed all of the horizontal and vertical cross-sectional Spectralis® OCT images recorded at each visit after the surgery. The retinal layer thicknesses were measured on the same selected central foveal location during the follow-up period with the embedded caliper measurement tool in the OCT. The CFT was defined as the thickness from the surface of the ILM to the outer border of the RPE at the central fovea (Fig. 1A). The thickness of the inner and outer retinal layers was measured at the superior, temporal, inferior, and nasal quadrants at 240 µm away from the center of the fovea in the vertical and horizontal scan images. The inner layer (INL) thickness and outer retinal layer (ORL) thickness (outer nuclear layer + outer plexiform layer) of these 4 quadrants were measured with the caliper function.
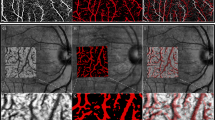
Preoperative fundus photographs and optical coherence tomographic (OCT) images of a 67-year-old man with an idiopathic epiretinal membrane (ERM). (A) Spectral domain OCT image (Spectralis). (B) Superficial foveal retinal capillary plexuses observed in OCT angiography (OCTA) image. The central foveal thickness (CFT) was measured as the distance between the surface of the ILM and the outer border of the retinal pigment epithelium at the center of the fovea. The inner nuclear layer (INL) thickness and the outer retinal layer (ONL) thickness were measured at 240 µm away from the fovea. The preoperative fundus photograph and a superimposed OCTA image at the superficial retinal capillary network layer. The retinal vasculature is shown by the white lines. The OCTA images are divided into 4 sectors by drawing a line from the retinal vessel bifurcations to the fovea. Then a line was drawn perpendicular to the original line. This divided the retina into the temporal, superior, nasal, and inferior quadrants. In addition, each quadrant was subdivided into an inner region and an outer region. The inner sector was defined as the region within a distance of 1 mm from the fovea and outer sector was outside the 1 mm region.
Optical coherence tomography angiography (OCTA)
We obtained the 3 × 3 mm en face images of the microvasculature in the macular region using the Angioplex (Zeiss Meditec. Inc, Germany) OCTA device16. The images of the superficial capillary network layer were used to measure the displacements of the retina and the area of the foveal avascular zone (FAZ; Fig. 2).
Representative pre- and postoperative fundus and OCT and OCTA images. Preoperative fundus photograph and a superimposed OCTA image of the superficial retinal capillary network of a 72-year-old woman with an ERM (A). The retinal vasculature is shown by the white lines. The postoperative fundus photograph with an OCTA image at Week 2 after the vitrectomy (B). The retinal vasculature is shown as red lines. The magnified OCTA preoperative image (white, C) and postoperative image (red, D) are superimposed in E. The images of the pre- and postoperative images were adjusted by matching retinal vessels around the optic disc. Pre- (F) and postoperative (G) SD-OCT images. The distance between the arrows was longer after the surgery.
All of the images were reviewed by the two graders (AM and TI) and low quality images were excluded from the analyses. The two graders measured the vascular displacements independently and were masked of the other clinical findings.
Measurements of displacement of retina using OCTA images
The displacement of retina was measured using the OCTA images as described in detail16. We adjusted the changes between the pre- and postoperative OCTA images by matching the retinal vasculature around the optic disc (Fig. 1B). The displacements of the retina were made relative to the fovea. To do this, we measured the distance between the fovea and an easily identifiable retinal vessels bifurcation pre- and postoperatively.
We divided the OCTA en face images into 4 quadrants as the superior, temporal, inferior, and nasal quadrants (Fig. 1B). Additionally, we divided each quadrant into an inner and outer region. The inner region was defined as the area within 1 mm from the fovea and the outer region was > 1 mm peripheral to the fovea. The average of the changes in the distance in each quadrant and region was determined.
Surgical techniques
A standard 25-gauge (G) three-port pars plana vitrectomy (PPV) was performed by one surgeon (TI) using the Constellation system (Alcon Laboratories, Inc., Fort Worth, TX, USA). After core vitrectomy, the ERM and ILM were peeled circumferentially from the retina with ILM-peeling forceps in all cases. Finally, we performed a peripheral vitrectomy with shaving and carefully inspection of the periphery over 360 degrees.
Cataract surgery and implanted a foldable acrylic IOL into the capsular bag were performed on all 19 phakic eyes.
Statistical analyses
One-way analysis of variance (ANOVA) was used to determine the significance of the correlations between the displacements in the four quadrants and the time of the surgery. Pearson’s correlation coefficient tests were used to determine the significance of the associations between the changes in the displacement of each bifurcation and other variables. All statistical analyses were performed using the Statistical Package for Social Sciences for Windows 21.0 (SPSS Inc, Chicago, IL).
Ethics statement
The Ethics Committee of Nagoya University Hospital approved the procedures used in this cross-sectional retrospective study. The procedures conformed to the tenets of the Declaration of Helsinki. All of the patients signed an informed consent form before the surgery.
Results
Demographics of patient
Forty-one eyes of 41 patients with an ERM underwent vitrectomy with ILM peeling and SD-OCT and OCTA examinations between December 2017 and March 2019. Twenty-one eyes were excluded: 8 for a pseudo macular hole, 3 for macular degeneration, 1 for macular edema, 3 for severe cataract that prevented obtaining high quality OCTA images, and 6 moved to another hospital immediately after the surgery that did not have sufficient postoperative examinations. In the end, 20 eyes of 20 patients (mean age, 70.6 ± 6.6 years) were studied. The demographics of the patients and the surgical procedures are shown in Table 1.
The mean postoperative best-corrected visual acuity (BCVA) was significantly improved (P < 0.001). The mean size of the ILM peeled area was 4.78 ± 0.44 disc diameters (DDs).
Changes in distance between retinal bifurcations and fovea
The mean number of retinal bifurcations that was identified was 71.0 ± 16.1/eye. The repeatability of the changes in the distance between the fovea and retinal vessel bifurcations between the graders was excellent with an ICC of 0.99.
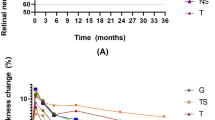
The distance between the fovea and retinal vessel bifurcations was significantly greater after the vitrectomy than before in all four quadrants (P < 0.001; Table 2), and the distance increased during the follow-up period (P < 0.001; Fig. 3A, Table 2). The outer sectors were significantly displaced in the temporal and the superior quadrants during the follow-up period, but the inner sector was significantly displaced only in the nasal quadrant during the follow-up period.
Displacements in the four quadrants after surgery and comparisons among the quadrants. The distance from the fovea and retinal vessel bifurcations was significantly shorter in all of the quadrants throughout the postoperative period (P < 0.001) (A). The outer sector was significantly displaced in the temporal and the superior quadrants during the follow-up period, but the inner sector was significantly displaced only in the nasal quadrant during the follow-up period. Comparisons of the changes in the distances in the 4 quadrants at Week 8 (B). The distance in the nasal quadrant was significantly greater than that in the temporal and inferior quadrants. The distances in the superior quadrant were significantly greater than that in the inferior quadrant.
The changes in the distance between the fovea and retinal vessel bifurcations at Week 8 was selected to compare the alterations in the 4 quadrants. The change in the distance in the nasal quadrant was significantly greater than that in the inferior (P < 0.001) and temporal (P = 0.036) quadrants, and it was significantly greater in the superior quadrant than the inferior quadrant (P = 0.005; Fig. 3B).
Changes in foveal avascular zone (FAZ) area
The mean preoperative FAZ area was 0.06 ± 0.03 mm2 in eyes with ERM, and it was significantly smaller than that of the fellow eye at 0.38 ± 0.07 mm2 (P < 0.001). The mean postoperative FAZ was 0.07 ± 0.03 mm2 at 2 weeks, 0.08 ± 0.03 mm2 at 4 weeks, and 0.09 ± 0.03 mm2 at 8 weeks after surgery. The increase in the area during the postoperative period was significant (P < 0.001). Of the 20 eyes, the area of FAZ in 18 eyes became larger after surgery.
Changes in retinal layer thickness
The mean preoperative CFT area was 406.3 ± 79.9 µm in eyes with an ERM which was significantly thicker than that of the fellow eye at 183.8 ± 16.7 µm (P < 0.001). The mean postoperative CFT was significantly thinner than the baseline thickness during the entire follow-up period (P = 0.020: Table 3).
The mean preoperative INL thickness was 70.9 ± 22.8 µm in the temporal, 91.8 ± 48.9 µm in the superior, 77.6 ± 27.5 in the nasal, and 69.5 ± 30.8 µm in the inferior quadrants. The mean postoperative INL thickness was significantly thinner only in the temporal quadrant during follow-up period (P < 0.001).
The mean preoperative ORL thickness was 238.9 ± 36.3 µm in the temporal, 221.6 ± 25.5 µm in the superior, 226.6 ± 28.1 µm in the nasal, and 235.8 ± 33.2 µm in the inferior quadrant. The mean postoperative ORL thickness was significantly thinner only in the temporal quadrant during the follow-up period (P < 0.001).
Relationships between displacements of retinal bifurcations and other factors
Single linear regression analysis showed that the changes in the distance between the retinal bifurcations and the fovea was significantly correlated with the changes in the area of the FAZ (r = 0.717, P < 0.001; Fig. 4), the CFT (r = − 0.702, P < 0.001) (Fig. 5), and the INL thickness (r = − 0.702, P < 0.001; Fig. 6), but not significantly correlated with the pre-and postoperative BCVA. The degree of the displacement of each vessel bifurcation at any time point was not significantly correlated with its preoperative distance from the fovea. The ORL thickness was not significantly correlated with other variables, e.g. the retinal displacement, the area of FAZ, the CFT, and the INL thickness.
Graphs showing the relationship between the changes in the INL thickness and the changes in the distance from the bifurcations. The changes in the INL thickness were significantly correlated with the changes in the distance between the fovea for all the bifurcations in each eye (A), but there was no significant correlation in the change between the ORL thickness and the distance (B).
Correlation between the CFT and the distance from the fovea to the bifurcations. The change in CFT was significantly correlated with the change in the distance between the fovea and all the bifurcations (A). In addition, the preoperative CFT was significantly correlated with the change in the distance between the fovea and all of bifurcations (B).
Correlation between the FAZ and the changes in the distance from the fovea to the bifurcations. The changes in FAZ area was significantly correlated with the change in the distance between the fovea and all of the bifurcations (A). In addition, the preoperative FAZ area was significantly correlated with the changes in distance between the fovea and all of the bifurcations (B).
Discussion
One of the advantages of using the OCTA images to evaluate the displacement is the ability to measure many points in a short time. We measured an average of 71.0 points for each eye in the OCTA images, which was a much larger number than previous reports17,18,19. Our results showed that the distance between the retinal bifurcations and the fovea was significantly displaced centrifugally and asymmetrically in all 4 quadrants after the removal of the ERM by vitrectomy with ILM peeling. The FAZ area became significantly smaller and the CFT significantly thicker than that of the fellow eyes before surgery, and the FAZ area was enlarged and the CFT became thinner after the surgery. The changes in the displacement of the retinal bifurcations was significantly correlated with that in the area of the FAZ, the CFT, and the INL thickness.
Recent advances in vitrectomy surgery and ERM removal with ILM peeling have improved surgical safety and visual outcomes for ERM patients. Actually, there have been reports showing that vitrectomy with ILM peeling resulted in better visual improvement and lower ERM recurrence rates6,20. Thus, we planted to perform ILM in addition to ERM peeling for eyes with ERM.
The retina was centrifugally displaced in all of the 4 quadrants, and the size of FAZ, which was much smaller than the fellow eye before surgery and was enlarged with time after the surgery. These results clearly show that the retina in the macular region was significantly displaced centrifugally after the surgery and which is consistent with previous reports17,18,19.
In comparing the displacements between the inner and outer sectors of the superior and inferior quadrants, the distance in those sectors should be similar from the optic disc and the nasal displacement caused by the ILM peeling should not be different. The displacement of the bifurcation in the outer sector was greater than that in the inner sector in those quadrants. Accordingly, the farther the bifurcations were to the fovea, the greater were the displacements. These results corroborate the centrifugal displacements after the surgery.
On the other hand, the displacements in the inner sectors were greater than that in the outer sectors only in the nasal quadrant. In addition, the retina in the nasal quadrant was displaced the most among the four quadrants after the surgery. It has been reported that the retina is displaced nasally after ILM peeling in eyes with retinochoroidal diseases21,22 including eyes with a macular hole16,23,24. Consequently, the retina in the macula area was displaced nasally in addition to centrifugally in our cohort. Akahori et al. reported that there was greater displacements of the bifurcations farther from the optic disc14. The postoperative asymmetrical displacement in the temporal and nasal quadrants can be explained as a displacement of the nasal retina by the same directional forces, viz., centrifugally and nasally, but the temporal retina was displaced by different directional forces. This asymmetrical displacement might affect the recovery of the visual dysfunction and distortion postoperatively.
Our study showed that the INL thickness became thinner after surgery and the change in the INL thickness was significantly correlated with the degree of retinal displacement. These results imply that the INL is thickened by a centripetal traction of the ERM on the macula resulting in the development of aniseikonia and metamorphopsia. The release of the traction causes the retinal displacement which is correlated with the reduction of the INL thickness. These observations support the earlier findings25,26,27,28.
A contraction of the ERM exerts tangential traction on the inner retina and overlying vessels, causing a movement of the retinal vessels toward the center29,30. In addition, the preoperative FAZ area and the CFT were correlated with the displacement of retina. Furthermore, the change in the FAZ area was correlated with the displacement of the bifurcations and the change in the CFT which is in good agreement with a previous report. These results suggest that the enlarged FAZ is related to the greater displacement of retina and reduction of the CFT. There have been several reports showing an association of the displacement of the retina with the changes in the retinal structures using OCT31 or retinal vasculature using OCTA32,33. Our results corroborate these earlier reports. Thus, a smaller preoperative FAZ and a thicker CFT may indicate greater macular contraction caused by the traction of the ERM and the progression of the disease process. Taken together, these findings indicate that the horizontal contraction in the macular area is correlated with the vertical contraction of the retina in eyes with an ERM.
In our cohort, the BCVA was not significantly correlated with the retinal displacement. There are several explanations for this. First, we evaluated the inner retinal displacement because retinal vessels are located in the inner retina but the structure of the outer retina may be more important for vision than the retinal displacements34. Second, there are several reports that the structure at the fovea is related to the vision in many retinochoroidal diseases which was not evaluated11,35.
This study has several limitations. First, we evaluated the displacement after a relatively short period of 8 weeks after the surgery. Second, the mean size of the ERM and ILM peeled was 4.78 ± 0.44 DD, and the size was not consistent among the eyes. Third, an imaging of the 6 × 6 mm area would be more helpful in terms of recognizing vasculature in a wider area. However, the resolution of the image is worse than that in smaller area of 3 × 3 mm, and this would make it more difficult to detect the bifurcations. Thus, we chose to use the 3 × 3 mm image. Fourth, we did not evaluate the eyes for aniseikonia and metamorphopsia, and it might have been better to investigate these parameters in addition to the BCVA to determine the functional changes after surgery. To resolve these limitations, prospective studies on a larger number of eyes with a longer follow-up periods are needed.
In conclusion, the distance between the retinal bifurcations and the fovea was asymmetrically increased after removal of the ERM by vitrectomy with ILM peeling. The change in the distances was correlated with the changes in the FAZ area and the CFT. These results indicate that a horizontal macular contraction is correlated with vertical retinal contraction in the eyes with an ERM.
References
Fraser-Bell, S., Guzowski, M., Rochtchina, E., Wang, J. J. & Mitchell, P. Five-year cumulative incidence and progression of epiretinal membranes: The Blue Mountains Eye Study. Ophthalmology110, 34–40 (2003).
Fraser-Bell, S., Ying-Lai, M., Klein, R. & Varma, R. Prevalence and associations of epiretinal membranes in latinos: The Los Angeles Latino Eye Study. Invest. Ophthalmol. Vis. Sci.45, 1732–1736 (2004).
Ichikawa, Y., Imamura, Y. & Ishida, M. Inner nuclear layer thickness, a biomarker of metamorphopsia in epiretinal membrane, correlates with tangential retinal displacement. Am. J. Ophthalmol.193, 20–27 (2018).
Sivalingam, A. et al. Visual prognosis correlated with the presence of internal-limiting membrane in histopathologic specimens obtained from epiretinal membrane surgery. Ophthalmology97, 1549–1552 (1990).
Pesin, S. R. et al. Vitrectomy for premacular fibroplasia. Prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology98, 1109–1114 (1991).
Park, D. W. et al. Macular pucker removal with and without internal limiting membrane peeling: Pilot study. Ophthalmology110, 62–64 (2003).
Ooto, S. et al. High-resolution imaging of the photoreceptor layer in epiretinal membrane using adaptive optics scanning laser ophthalmoscopy. Ophthalmology118, 873–881 (2011).
Inoue, M. et al. Inner segment/outer segment junction assessed by spectral-domain optical coherence tomography in patients with idiopathic epiretinal membrane. Am. J. Ophthalmol.150, 834–839 (2010).
Watanabe, A., Arimoto, S. & Nishi, O. Correlation between metamorphopsia and epiretinal membrane optical coherence tomography findings. Ophthalmology116, 1788–1793 (2009).
Ogasawara, Y., Iwase, T., Yamamoto, K., Ra, E. & Terasaki, H. Relationship between abnormalities of photoreceptor microstructures and microvascular structures determined by optical coherence tomography angiography in eyes with branch retinal vein occlusion. Retina.40, 350–358 (2018).
Kobayashi, M. et al. Association between photoreceptor regeneration and visual acuity following surgery for rhegmatogenous retinal detachment. Invest. Ophthalmol. Vis. Sci.57, 889–898 (2016).
Hasegawa, T., Ueda, T., Okamoto, M. & Ogata, N. Relationship between presence of foveal bulge in optical coherence tomographic images and visual acuity after rhegmatogenous retinal detachment repair. Retina.34, 1848–1853 (2014).
Okawa, Y. et al. Foveal structure and vasculature in eyes with idiopathic epiretinal membrane. PLoS ONE14, e0214881 (2019).
Jia, Y. et al. Split-spectrum amplitude-decorrelation angiography with optical coherence tomography. Opt Express.20, 4710–4725 (2012).
Jia, Y. et al. Quantitative optical coherence tomography angiography of vascular abnormalities in the living human eye. Proc. Natl. Acad. Sci. USA112, E2395-2402 (2015).
Akahori, T. et al. Macular displacement after vitrectomy in eyes with idiopathic macular hole determined by optical coherence tomography angiography. Am. J. Ophthalmol.189, 111–121 (2018).
Rodrigues, I. A., Lee, E. J. & Williamson, T. H. Measurement of retinal displacement and metamorphopsia after epiretinal membrane or macular hole surgery. Retina.36, 695–702 (2016).
Yang, H. K. et al. Improvement of horizontal macular contraction after surgical removal of epiretinal membranes. Eye (Lond).25, 754–761 (2011).
Koizumi, H. et al. Three-dimensional evaluation of vitreomacular traction and epiretinal membrane using spectral-domain optical coherence tomography. Am. J. Ophthalmol.145, 509–517 (2008).
Chang, W. C. et al. Vitrectomy with or without internal limiting membrane peeling for idiopathic epiretinal membrane: A meta-analysis. PLoS ONE12, e0179105 (2017).
Yoshikawa, M. et al. Macular migration toward the optic disc after inner limiting membrane peeling for diabetic macular edema. Invest. Ophthalmol. Vis. Sci.54, 629–635 (2013).
Kumagai, K., Ogino, N., Furukawa, M., Ooya, R. & Horie, E. Early centripetal displacements of capillaries in macular region caused by internal limiting membrane peeling. Clin. Ophthalmol.12, 755–763 (2018).
Kawano, K. et al. Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling. Eye (Lond).27, 871–877 (2013).
Ishida, M. et al. Retinal displacement toward optic disc after internal limiting membrane peeling for idiopathic macular hole. Am. J. Ophthalmol.157, 971–977 (2014).
Okamoto, F., Sugiura, Y., Okamoto, Y., Hiraoka, T. & Oshika, T. Associations between metamorphopsia and foveal microstructure in patients with epiretinal membrane. Invest. Ophthalmol. Vis. Sci.53, 6770–6775 (2012).
Chung, H. et al. Relationship between vertical and horizontal aniseikonia scores and vertical and horizontal OCT images in idiopathic epiretinal membrane. Invest. Ophthalmol. Vis. Sci.56, 6542–6548 (2015).
Arimura, E. et al. Retinal contraction and metamorphopsia scores in eyes with idiopathic epiretinal membrane. Invest. Ophthalmol. Vis. Sci.46, 2961–2966 (2005).
Nomoto, H. et al. Quantification of changes in metamorphopsia and retinal contraction in eyes with spontaneous separation of idiopathic epiretinal membrane. Eye (Lond).27, 924–930 (2013).
Minchiotti, S. et al. Human idiopathic epiretinal membranes express NGF and NGF receptors. Retina.28, 628–637 (2008).
Gupta, P., Sadun, A. A. & Sebag, J. Multifocal retinal contraction in macular pucker analyzed by combined optical coherence tomography/scanning laser ophthalmoscopy. Retina.28, 447–452 (2008).
Kofod, M. & la Cour, M. Quantification of retinal tangential movement in epiretinal membranes. Ophthalmology119, 1886–1891 (2012).
Nelis, P., Alten, F., Clemens, C. R., Heiduschka, P. & Eter, N. Quantification of changes in foveal capillary architecture caused by idiopathic epiretinal membrane using OCT angiography. Graefes Arch. Clin. Exp. Ophthalmol.255, 1319–1324 (2017).
Mastropasqua, R. et al. Early retinal flow changes after vitreoretinal surgery in idiopathic epiretinal membrane using swept source optical coherence tomography angiography. J Clin Med.8, 2 (2019).
Hosoda, Y., Ooto, S., Hangai, M., Oishi, A. & Yoshimura, N. Foveal photoreceptor deformation as a significant predictor of postoperative visual outcome in idiopathic epiretinal membrane surgery. Invest. Ophthalmol. Vis. Sci.56, 6387–6393 (2015).
Hasegawa, T., Ueda, T., Okamoto, M. & Ogata, N. Presence of foveal bulge in optical coherence tomographic images in eyes with macular edema associated with branch retinal vein occlusion. Am. J. Ophthalmol.157, 390-396.e391 (2014).
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Contributions of authors: The design and conduct of the study (T.I.); collection of data (A.M.); management, analysis, and interpretation of data (A.M., T.I., T. A., G.K., K.Y., E. R.); and preparation, review, and approval of the manuscript (A.M., T.I., T. A., G.K., K.Y., E. R., H.T.).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Momota, A., Iwase, T., Akahori, T. et al. Association between displacement and thickness of macula after vitrectomy in eyes with epiretinal membrane. Sci Rep 10, 13227 (2020). https://doi.org/10.1038/s41598-020-70197-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70197-6
This article is cited by
-
A novel vector field analysis for quantitative structure changes after macular epiretinal membrane surgery
Scientific Reports (2024)
-
Microperimetric evaluation for different methods of epiretinal membrane surgery
BMC Ophthalmology (2023)
-
Displacement of the retina and changes in the foveal avascular zone area after internal limiting membrane peeling for epiretinal membrane
Japanese Journal of Ophthalmology (2023)
-
Vascular tortuosity analysis in eyes with epiretinal membrane imaged by optical coherence tomography angiography
BMC Ophthalmology (2022)
-
Stellungnahme von BVA, DOG und RG zur Entwicklung, Diagnostik und Behandlung der epiretinalen Gliose
Der Ophthalmologe (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.