Abstract
To test the association between bilateral nephrectomies in patients with autosomal recessive polycystic kidney disease (ARPKD) and long-term clinical outcome and to identify risk factors for severe outcomes, a dataset comprising 504 patients from the international registry study ARegPKD was analyzed for characteristics and complications of patients with very early (≤ 3 months; VEBNE) and early (4–15 months; EBNE) bilateral nephrectomies. Patients with very early dialysis (VED, onset ≤ 3 months) without bilateral nephrectomies and patients with total kidney volumes (TKV) comparable to VEBNE infants served as additional control groups. We identified 19 children with VEBNE, 9 with EBNE, 12 with VED and 11 in the TKV control group. VEBNE patients suffered more frequently from severe neurological complications in comparison to all control patients. Very early bilateral nephrectomies and documentation of severe hypotensive episodes were independent risk factors for severe neurological complications. Bilateral nephrectomies within the first 3 months of life are associated with a risk of severe neurological complications later in life. Our data support a very cautious indication of very early bilateral nephrectomies in ARPKD, especially in patients with residual kidney function, and emphasize the importance of avoiding severe hypotensive episodes in this at-risk cohort.
Similar content being viewed by others
Introduction
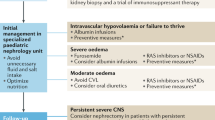
Autosomal recessive polycystic kidney disease (ARPKD) is a severe and mostly early-onset hepatorenal disorder mainly caused by mutations in the PKHD1 gene1,2,3. Mutations in a second gene, DZIP1L, have recently been associated with an ARPKD phenotype3,4. Affected newborns may suffer from massive kidney enlargement and may require early kidney replacement therapy (KRT). Peritoneal dialysis (PD) is then considered the dialysis modality of choice5. It has been suggested that large kidneys may contribute to respiratory problems and may hamper nutritional support6,7. The respiratory situation in ARPKD neonates can be challenging due to pulmonary hypoplasia and additional abdominal pressure by PD. Furthermore, concerns about the feasibility of PD in cases of massive renal enlargement have been raised. In some infants with severe ARPKD, uni- or bilateral nephrectomies are therefore performed with the aim to improve the respiratory, nutritional and dialysis conditions6,7,8. However, nephrectomies have not been shown to improve the respiratory situation and the rationale for nutritional improvement is based on small studies regarding unilateral nephrectomy9,10,11. Even in severely affected infants, residual kidney function may be preserved in ARPKD and may even improve during the first months of life12. Obviously, bilateral nephrectomies result in a life-long need for KRT. Additionally, arterial hypotension has been reported after bilateral nephrectomies and may contribute to neurological or ophthalmological complications in young PD patients13,14,15,16. The association of early bilateral nephrectomies in general and of the timing of the second nephrectomy in particular with long-term outcome in ARPKD patients remains unclear. To address this topic, we analyzed the comprehensive pre-, peri- and postnatal information captured in the ARegPKD registry study17,18.
Results
Characteristics of patient subgroups
At the timepoint of analysis, 504 patients with the clinical diagnosis of ARPKD and sufficient data quality were registered in the ARegPKD registry. Of these, 19 patients (3.8%) with very early bilateral nephrectomies (within first 3 months of life, VEBNE) and further 9 patients (1.8%) with early bilateral nephrectomies (first nephrectomy within first 15 months of life, second nephrectomy at age 4–15 months, EBNE) were identified. We included a control group of 11 patients, who had very large total kidney volumes (TKV) comparable to VEBNE patients (TKV > ~ 200 ml, measured by ultrasound within the first 3 months of life), but were not treated with early nephrectomy or dialysis (TKV control group). Pole-to-pole lengths, single kidney volumes and total kidney volumes did not differ significantly between VEBNE and TKV control patients but TKV control patients were slightly older at measurement (Table 1). To account for effects of very early dialysis (VED) onset, an additional control group was defined with 12 ARPKD patients with dialysis onset within the first 3 months of life without bilateral nephrectomies in their disease course (VED). Patients were grouped according to their clinical status at time of last documented observation in the registry or at time prior to their death. The patient characteristics regarding nephrectomies and KRT are depicted in Table 2.
Indications for nephrectomies
In VEBNE patients, indications for nephrectomies encompassed respiratory failure and/or ventilation problems, abdominal distension and/or massive kidney enlargement and onset of or problems with PD (Table 2). Most patients with sequential nephrectomies started dialysis after the first nephrectomy (11/17, 65%). Two patients of the VED group received very early unilateral nephrectomy. In the TKV control group, two patients received unilateral nephrectomy during combined liver and kidney transplantation surgery later in life.
Pre- and perinatal characteristics
Detailed information on patient characteristics is provided in Table 3. VEBNE and TKV control patients more frequently showed poor postnatal respiratory adaptation and were more often admitted to neonatal intensive care units (NICU). Other characteristics—including gestational age, birth weight, length, head circumference as well as Apgar scores and requirement of respiratory support—did not show relevant differences between the groups.
Long-term complications with focus on neurological development and risk factors for severe neurological complications
In a first step, we addressed the occurrence of relevant symptoms or complications including blood pressure alterations, neurological symptoms, sepsis, cardiopulmonary resuscitation and death in a descriptive manner in the four different patient groups. Among all complications investigated, the most profound differences were observed in the neurological outcome: seizures and severe neurological complications encompassing ischemic defects, hypoxic brain damage, brain infarct, parenchymal defect, severe neurodevelopmental disorder and optic neuropathy with vision loss occurred more frequently in VEBNE patients. While 12/19 (63%) VEBNE patients were affected by severe neurological complications, this was true for only 2/9 (22%) EBNE, 2/12 (17%) VED and none of the 11 TKV control patients. Of the 12 affected VEBNE patients, three suffered from cerebral ischemia, three from infarction, bleeding or parenchymal defects, three from optic neuropathy (with vision loss), two from combined cerebral ischemia or hypoxemia and optic neuropathy, and one from cerebral ischemia with bleeding. The two EBNE patients developed sinus vein thrombosis and bilateral cerebral infarctions, the two VED patients developed posthypoxic ischemic lesions after a very difficult postnatal adaptation and hydrocephalus with brain atrophy. Neurodevelopmental delay occurred most frequently in VEBNE patients. In a re-survey with specific questions on the psychomotoric development, only one of 17 (6%) studied VEBNE patients was classified to have a normal development compared to 2/8 (25%) EBNE patients, 5/11 (46%) VED patients and 5/8 (63%) TKV control patients. Approximately one third of VEBNE patients suffered from severely or very severely affected psychomotoric development each. Younger ages at the timepoint of second nephrectomy were more frequently documented in those patients with severe neurological and developmental complications, especially timepoints of second nephrectomy within the first 3 months of life (Suppl. Figure S1). The proportions of patients receiving some form of specific therapies for developmental complications were high in all four patient groups, ranging from 55% in VED to 94% in VEBNE patients. Microcephaly was hardly found at birth but was most frequently documented in VEBNE patients in the further course (11/19, 58%). Severe hyper- and hypotensive episodes as well as cardiopulmonary resuscitation (CPR) were reported for subcohorts of VEBNE and EBNE patients, without reports in VED and TKV control patients. Proportions of patients with a septic episode prior to the evaluated neurological complication did not differ significantly between the groups (Table 4).
Follow-up time was similar for VEBNE, EBNE and TKV control patients, but shorter for VED patients (Table 4). Severe neurological complications were further studied over time using Kaplan–Meier analyses and Cox regression analyses. Survival without severe neurological complications after 7 years was approximately 30% in VEBNE, 80% in EBNE, 70% in VED patients and 100% in TKV control patients according to Kaplan–Meier survival analysis (Fig. 1). Thus, VEBNE patients showed significantly worse outcome than EBNE or TKV control patients with a similar trend compared to VED patients. Severe neurological complications in the VEBNE group were evident within the 14 months of life in most cases (10/12). Only in two patients, atrophy of the optic nerve was diagnosed at the ages of 2.8 and 6.6 years.
Kaplan–Meier survival without severe neurological complications by patient group. Censored observations (last documented follow-up or death) are marked with a cross. P values were derived using log rank tests. EBNE early bilateral nephrectomies, TKV total kidney volume, VEBNE very early bilateral nephrectomies, VED very early dialysis.
Overall, severe neurological complications occurred in 16 of 51 (31%) analyzed patients (Table 5). According to Cox regression analysis, the report of severe neurological complications was associated with multiple factors, such as documentation of microcephaly during the course of follow-up as well as weaker and more common neurological symptoms like seizures and reports of severe hypertensive and hypotensive episodes. Furthermore, patients with very early bilateral nephrectomies seemed to be at special risk.
To identify independent risk factors associated with severe neurological complications, multivariate Cox regression analysis with consecutive backward selection was performed (including seizures, documentation of microcephaly, severe hypertensive episodes, severe hypotensive episodes and VEBNE), which revealed the report of a severe hypotensive episode and very early bilateral nephrectomies to be independent risk factors for severe neurological complications (Table 5). In this multivariate analysis, patients with very early bilateral nephrectomies were at fivefold elevated risk for severe neurological complications.
Deaths
Three VEBNE patients died due to cerebral ischemia (age 3.2 months), respiratory failure (7.8 months) and massive postoperative bleeding after revision of dialysis catheter (age 73.8 months). Two EBNE patients died, one due to a septic episode in leukemia (age 40.4 months) and the other patient due to aspiration (75.0 months). Causes of death in six VED patients were indicated as sepsis (ages 5.4 months, 5.7 months, 13.3 months), lung hemorrhage (age 1.8 months) and parental wish to withdraw care in two cases (ages 0.8 months, 2.2 months). Importantly, four of the six deceased VED patients did not display major or severe neurological complications before death. Three out of the four VED patients that passed away without withdrawal of care died after the fifth month of life. One patient from the TKV control group died shortly postnatally due to respiratory failure.
Discussion
The management of severely affected neonates and infants with ARPKD remains a matter of intense debate. The aim of this study was to examine the association of the timing of bilateral nephrectomies with long-term complications in ARPKD patients.
In our analysis, ARPKD patients with very early bilateral nephrectomies (VEBNE) within the first 3 months of life showed significantly more neurological complications than patients who underwent bilateral nephrectomies receiving their second nephrectomy after the third month of life (EBNE). The severe neurological anomalies observed in VEBNE patients encompassed cerebral ischemia or infarcts, parenchymal brain defects, brain volume decrease, subdural bleeding and (anterior ischemic) optic neuropathy. These complications occurred predominantly during the first year of life.
The rationale of drawing a line for evaluation of consequences of bilateral nephrectomies at the age of 3 months was based on two considerations: firstly, major maturation processes of autonomic cardiovascular control seem to occur within the first 3 months of life19,20. Animal models suggest that renal sympathetic nerve control matures postnatally21. Secondly, both plasma renin activities and aldosterone levels22,23 have been reported to peak within the first 3 months with a steep decline afterwards. Data from healthy infants demonstrated a remarkable increase of systolic blood pressure during the first 6 weeks and a physiologic dip of diastolic blood pressure after birth with a gradual increase during the first year of life from month two to three on24. Summarizing these hypotheses, the removal of both kidneys in this early phase of life might result in the maximum impact by abolishing blood pressure autoregulation. Plotting the occurrence of severe neurological complications against the age at second nephrectomy supports the choice of drawing a line at the age of 3 months as critical time point (Suppl. Figure S1).
Interestingly, our analysis demonstrated that VEBNE and severe hypotensive episodes were independently associated with severe neurological complications. In addition to VEBNE additional factors leading to hypotensive episodes seem to be involved, e.g. acute illnesses25. Previous smaller case series reported an anephric status and ARPKD as risk factors for development of anterior ischemic optic neuropathy in patients on PD26. Hypovolemia has been reported in half of the affected infants with anterior ischemic optic neuropathy on PD26. In our study, optic neuropathy was frequently observed in the VEBNE group. One might speculate about common pathophysiologic mechanisms underlying to all types of cerebral defects, such as reduced cerebral autoregulation and chronic hypotension with increased vulnerability in acute hypotensive episodes. Fluid management per se can pose major challenges in infants on PD, but might affect blood pressure more immediately in anephric infants. In our analysis, we did not have comprehensive data on the fluid status of patients. It is worth noting that cardiopulmonary resuscitation was documented most frequently in the VEBNE patient group. Despite the challenges of fluid management in anephric infants, PD remains the preferred modality for ARPKD infants11. A recent analysis showed that technique survival in ARPKD is comparable to that observed in other early-onset kidney diseases, although PD in ARPKD may require smaller fill volumes and/or more cycles27. Our analysis emphasizes in particular the association of documented pronounced hypotensive episodes with severe neurological complications in ARPKD patients receiving early bilateral nephrectomies and underlines the recommendation of very tight blood pressure control for all anephric children on PD. Furthermore, measures to avoid hypotensive episodes on PD need to be considered, e.g. by avoiding high glucose solutions or by sodium supplementation in dialysate and nutritionally25,28,29. On the other hand, ARPKD specific therapeutic options and clinical studies are eagerly awaited for this severely affected patient population.
None of the TKV control patients with massively enlarged kidneys developed severe neurological complications. Caution is required not to anticipate postnatal severe courses in all cases of newborns with pre- and perinatal anomalies30.
Severe neurological complications were observed in two VED patients: in one patient cerebral ischemia occurred during a very difficult postnatal adaptation requiring intense cardiorespiratory support and unilateral nephrectomy. This patient passed away at the age of 4 weeks after withdrawal of intensive care treatment upon parental request. The other patient died from sepsis at 13 months of age after documentation of hydrocephalus with brain atrophy 1 month earlier. All four of the six deceased VED infants who did not experience severe neurological complications deceased within the first 8 months of life. This is important for the interpretation of the Kaplan–Meier survival analysis for severe neurological complications (Fig. 1). Due to their early death, these patients were no longer at risk for severe neurological complications. Thus, death could be a competing risk for severe neurological complications in this specific subcohort. Survival without severe neurological complications tended to be better in VED compared to VEBNE patients, although statistical significance was missed due to small sample size. Importantly, the majority of the deceased VED patients died well beyond 3 months of age. EBNE patients were also severely affected with similar Apgar values as VEBNE and early dialysis dependency. Yet, only two of nine EBNE patients suffered from severe neurological sequelae, arguing against an intrinsic ARPKD-specific neurologic phenotype.
The current study faces limitations: as severely affected and/or early deceased patients are likely to be underrepresented in our registry study, the obtained sample sizes of the four groups are rather small. Furthermore, there might be a center bias in deciding for nephrectomies in infants. The risk factor severe hypotensive episodes needs to be interpreted carefully: the report and documentation might be biased by the personal perception of the attending physicians and severely affected children might spend more time in hospital, where blood pressure documentation could reveal anomalies more frequently. Hypotensive episodes are known to frequently occur within hypovolemia in infants on PD25,31,32. Our study describes interesting associations of severe hypotensive episodes and the decision to perform VEBNE with severe neurological complications, but we cannot prove causality due to the retrospective registry data underlying the analysis. Importantly, in severely affected infants there may be situations where the decision for uni- or bilateral nephrectomies appears inevitable. Given our data a thorough discussion of all relevant aspects both with the parents and the attending medical team seems important.
Conclusion
Neurological complications occur more frequently in patients with bilateral nephrectomies performed during the first 3 months of life compared to patients with the second nephrectomy performed between 4 and 15 months of age. Our data suggest utmost caution in the decision-making process for very early bilateral nephrectomies, especially in infants with partially conserved residual renal function, and support postponing the second nephrectomy when possible. Importantly, every effort should be made to avoid pronounced hypotensive episodes in this population.
Methods
Registry
The international cohort study ARegPKD follows patients with the clinical diagnosis of ARPKD according to the previously described protocol17,18. In summary, basic data and regular follow-up data sets are obtained and are subject to regular data quality control. The study protocol was approved by the Ethics Committee of the Faculty of Medicine of Cologne University and the Institutional Review Boards of participating sites. Informed consent was obtained from all subjects or, if subjects are under 18, from a parent and/or legal guardian according to applicable local regulations. All methods were carried out in accordance with relevant guidelines and regulations.
For this specific analysis ischemic brain defects, hypoxic brain damage, brain infarct, parenchymal defect, severe neurodevelopmental disorder and optic neuropathy with vision loss were rated as severe neurological complication. For detailed classification of neurocognitive development, we re-surveyed data on head circumferences at birth and during further course, school education, specific therapies, developmental milestones and psychological/intelligence testing for the studied subcohort: psychomotoric development was classified as normal or mildly, severely or very severely disordered. Head circumferences at birth were graded in percentiles according to the revised Fenton growth chart33.
All PKHD1 variants were classified according to criteria of the American College of Medical Genetics (ACMG)34. Sonography-based kidney volumes were calculated according to the ellipsoid formula (length × width × depth × π/6) and standardized to standard deviation scores (SDS) to pediatric normal values35,36.
Statistics
Data analysis was performed on the dataset available in September 2018 using SPSS 25 (IBM Corp., Armonk, NY, USA) for statistical analyses. Data completeness varied by variable. Continuous variables were described using the number of non-missing values, mean and standard deviation (SD) as well as median and interquartile range (IQR). For binary or categorical variables, absolute and relative frequencies were provided. Event-free survival rates were estimated by the Kaplan–Meier method. Follow-up duration in the four groups were calculated using the reverse Kaplan–Meier method, displayed as median (IQR) and compared using log-rank test. Differences of (continuous) sonographic parameters between VEBNE and control group were compared by Mann–Whitney U test. Differences between the four patient groups were assessed by Kruskal–Wallis tests for continuous and by chi-squared tests for binary or categorical variables. The statistical tests did not adjust formally for multiplicity due to the exploratory nature of the analysis. No imputation was performed.
To investigate the predictive value of clinical risk factors for severe neurological outcome, Cox regression analysis was performed for each risk factor separately. The parameters with a p value below 0.10 were then included in a Cox multiple regression analysis with consecutive backward selection for variables with a p value below 0.10.
To assess the differences of survival without severe neurological complications in the four patient groups, Kaplan–Meier analysis and log rank tests were used. All analyses are exploratory and p values of less than 0.05 were considered significant in a descriptive manner in distinguishing between the groups.
Data availability
The data that support the findings of this study are available, on reasonable request, from the corresponding author.
Abbreviations
- ARPKD:
-
Autosomal recessive polycystic kidney disease
- CLKTx:
-
Combined liver and kidney transplantation
- CVVH:
-
Continuous veno-venous hemofiltration
- EBNE:
-
Early bilateral nephrectomies
- FTT:
-
Failure to thrive
- HR:
-
Hazard ratio
- HD:
-
Hemodialysis
- KRT:
-
Kidney replacement therapy
- NE:
-
Nephrectomy/nephrectomies
- P:
-
Percentile
- PD:
-
Peritoneal dialysis
- PTP:
-
Pole-to-pole
- SDS:
-
Standard deviation scores
- TKV:
-
Total kidney volume
- VEBNE:
-
Very early bilateral nephrectomies
- VED:
-
Very early dialysis
References
Ward, C. J. et al. The gene mutated in autosomal recessive polycystic kidney disease encodes a large, receptor-like protein. Nat Genet 30, 259–269 (2002).
Onuchic, L. F. et al. PKHD1, the polycystic kidney and hepatic disease 1 gene, encodes a novel large protein containing multiple immunoglobulin-like plexin-transcription-factor domains and parallel beta-helix 1 repeats. Am J Hum Genet 70, 1305–1317 (2002).
Bergmann, C. et al. Polycystic kidney disease. Nat Rev Dis Primer 4, 50 (2018).
Lu, H. et al. Mutations in DZIP1L, which encodes a ciliary-transition-zone protein, cause autosomal recessive polycystic kidney disease. Nat Genet 49, 1025–1034 (2017).
Zurowska, A. M. et al. Clinical practice recommendations for the care of infants with stage 5 chronic kidney disease (CKD5). Pediatr. Nephrol. Berl. Ger. 28, 1739–1748 (2013).
Luoto, T. T., Pakarinen, M. P., Jahnukainen, T. & Jalanko, H. Liver disease in autosomal recessive polycystic kidney disease: clinical characteristics and management in relation to renal failure. J. Pediatr. Gastroenterol. Nutr. 59, 190–196 (2014).
Hoyer, P. F. Clinical manifestations of autosomal recessive polycystic kidney disease. Curr. Opin. Pediatr. 27, 186–192 (2015).
Beaunoyer, M. et al. Optimizing outcomes for neonatal ARPKD. Pediatr. Transplant. 11, 267–271 (2007).
Bean, S. A., Bednarek, F. J. & Primack, W. A. Aggressive respiratory support and unilateral nephrectomy for infants with severe perinatal autosomal recessive polycystic kidney disease. J. Pediatr. 127, 311–313 (1995).
Shukla, A. R., Kiddoo, D. A. & Canning, D. A. Unilateral nephrectomy as palliative therapy in an infant with autosomal recessive polycystic kidney disease. J. Urol. 172, 2000–2001 (2004).
Guay-Woodford, L. M. et al. Consensus expert recommendations for the diagnosis and management of autosomal recessive polycystic kidney disease: report of an international conference. J. Pediatr. 165, 611–617 (2014).
Cole, B. R., Conley, S. B. & Stapleton, F. B. Polycystic kidney disease in the first year of life. J. Pediatr. 111, 693–699 (1987).
Riechardt, S., Koch, M., Oh, J. & Fisch, M. Early bilateral nephrectomy in neonatal autosomal recessive polycystic kidney disease: Improved prognosis or unnecessary effort?. Urol. Ausg. A 56, 882–886 (2017).
Hassinger, A. B. & Garimella, S. Refractory hypotension after bilateral nephrectomies in a Denys–Drash patient with phenylketonuria. Pediatr. Nephrol. Berl. Ger. 28, 345–348 (2013).
Al-Kaabi, A. et al. Bilateral anterior ischaemic optic neuropathy in a child on continuous peritoneal dialysis: case report and literature review. Sultan Qaboos Univ. Med. J. 16, e504–e507 (2016).
van Lieburg, A. F. & Monnens, L. A. Persistent arterial hypotension after bilateral nephrectomy in a 4-month-old infant. Pediatr. Nephrol. Berl. Ger. 16, 604–605 (2001).
Ebner, K. et al. Rationale, design and objectives of ARegPKD, a European ARPKD registry study. BMC Nephrol. 16, 22 (2015).
Ebner, K., Schaefer, F., Liebau, M. C. & ARegPKD Consortium. Recent Progress of the ARegPKD Registry Study on autosomal recessive polycystic kidney disease. Front. Pediatr. 5, 18 (2017).
Yiallourou, S. R., Sands, S. A., Walker, A. M. & Horne, R. S. C. Maturation of heart rate and blood pressure variability during sleep in term-born infants. Sleep 35, 177–186 (2012).
Yiallourou, S. R., Sands, S. A., Walker, A. M. & Horne, R. S. C. Postnatal development of baroreflex sensitivity in infancy. J. Physiol. 588, 2193–2203 (2010).
Booth, L. C. et al. Maturation-related changes in the pattern of renal sympathetic nerve activity from fetal life to adulthood. Exp. Physiol. 96, 85–93 (2011).
Bauer, J. H. Age-related changes in the renin-aldosterone system. Physiological effects and clinical implications. Drugs Aging 3, 238–245 (1993).
Siegler, R. L., Crouch, R. H., Hackett, T. N., Walker, M. & Jubiz, W. Potassium-renin-aldosterone relationships during the first year of life. J Pediatr 91, 52–55 (1977).
Report of the Second Task Force on Blood Pressure Control in Children. Task force on blood pressure control in children. National Heart, Lung, and Blood Institute, Bethesda, Maryland. Pediatrics 1987(79), 1–25 (1987).
Schaefer, F. Peritoneal dialysis in infants: never lose sight of-and from-arterial hypotension!. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 35, 123–124 (2015).
Dufek, S. et al. Anterior ischemic optic neuropathy in pediatric peritoneal dialysis: risk factors and therapy. Pediatr. Nephrol. Berl. Ger. 29, 1249–1257 (2014).
Akarkach, A. et al. Maintenance peritoneal dialysis in children with autosomal recessive polycystic kidney disease: a comparative cohort study of the international pediatric peritoneal dialysis network registry. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 75, 460–464 (2020).
Di Zazzo, G. et al. Anterior ischemic optical neuropathy in children on chronic peritoneal dialysis: report of 7 cases. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 35, 135–139 (2015).
KDOQI Work Group. KDOQI Clinical Practice Guideline for Nutrition in Children with CKD: 2008 update Executive summary. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 53, 11–104 (2009).
Burgmaier, K. et al. Risk factors for early dialysis dependency in autosomal recessive polycystic kidney disease. J. Pediatr. https://doi.org/10.1016/j.jpeds.2018.03.052 (2018).
Vidal, E. & Schaefer, F. Hypotension in infants on chronic peritoneal dialysis: mechanisms, complications, and management. Adv. Perit. Dial. Conf. Perit. Dial. 31, 54–58 (2015).
Rippe, B. & Venturoli, D. Optimum electrolyte composition of a dialysis solution. Perit. Dial. Int. J. Int. Soc. Perit. Dial. 28(Suppl 3), S131-136 (2008).
Fenton, T. R. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 13, 59 (2013).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. Off. J. Am. Coll. Med. Genet. 17, 405–424 (2015).
Scholbach, T. & Weitzel, D. Body-surface-area related renal volume: a common normal range from birth to adulthood. Scientifica 2012, 949164 (2012).
Weitzel, D. Nieren und ableitende Harnwege. In Die Ultraschalluntersuchung des Kindes (eds Deeg, K.-H. et al.) 289–324 (Springer, Berlin, Heidelberg, 1997).
Acknowledgements
We thank Ms Regina Brinster and Mr Samuel Kilian for support in conducting statistical analysis. Parts of this work have been presented as a poster presentation at ASN “Kidney Week 2019” in Washington, DC, USA on November 7th 2019 (please see https://www.asn-online.org/education/kidneyweek/2019/program-abstract.aspx?controlId=3232194 as accessed on the 11th of April 2020).
Funding
We thank the German Society for Pediatric Nephrology (GPN) and the ESCAPE Network for their support. ML was supported by grants of the GPN, the European Society for Paediatric Nephrology (ESPN), the German PKD foundation, the Koeln Fortune program, the GEROK program of the Medical Faculty of University of Cologne, and the Marga and Walter Boll-Foundation. FS and ML are supported by the the German Federal Ministry of Research and Education (BMBF grant 01GM1515 and 01GM1903). KB was supported by the Koeln Fortune program of the Medical Faculty of University of Cologne and the Marga and Walter Boll-Foundation. This work was generated within the European Reference Network for Rare Kidney Disorders (ERKNet). Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Contributions
K.B. and M.L. drafted the manuscript. K.B. and M.B. performed statistical analysis. K.B., G.A., M.B., A.K.B., F.E., M.G., I.G., J.K., C.K., L.M., A.M., D.M., L.P., L.P., A.P., G.S., R.S., R.S., M.S., K.T.J., M.T., L.T.W., E.W., D.W., S.W., I.Z., J.D., J.O., F.S. and M.L. coordinated clinical care of patients and gathered clinical or genetic information. K.B., J.O., F.S. and M.L. set up this substudy, F.S. and M.L. set up the ARegPKD database, M.L. had overall oversight of the project. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
ML has received honoraria for scientific lectures from Pfizer. Representing the University Hospital of Cologne ML has been counselling Otsuka in an advisory board. DM, represented by KU Leuven University, received an educational grant from Otsuka and participated in an advisory board. The other authors declare no potential conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Burgmaier, K., Ariceta, G., Bald, M. et al. Severe neurological outcomes after very early bilateral nephrectomies in patients with autosomal recessive polycystic kidney disease (ARPKD). Sci Rep 10, 16025 (2020). https://doi.org/10.1038/s41598-020-71956-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-71956-1
This article is cited by
-
Native nephrectomy in advanced pediatric kidney disease: indications, timing, and surgical approaches
Pediatric Nephrology (2024)
-
Shift from severe hypotension to salt-dependent hypertension in a child with autosomal recessive polycystic kidney disease after bilateral nephrectomies: a case report
BMC Nephrology (2023)
-
Complications and prognosis of patients diagnosed with autosomal recessive polycystic kidney disease in neonatal period
CEN Case Reports (2023)
-
Autosomal-rezessive polyzystische Nierenerkrankung (ARPKD)
Der Nephrologe (2022)
-
Translational research approaches to study pediatric polycystic kidney disease
Molecular and Cellular Pediatrics (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.