Abstract
Objective:
To assess the effects of exercise therapy (ET) on motor control and functional ability of the upper extremity in patients with cervical spinal cord injury (SCI).
Methods:
An extensive systematic literature search in five databases was performed to identify clinical and (randomized) controlled trials, evaluating the effects of ET on motor control and functional ability in patients with SCI. The methodological quality of the selected studies was systematically assessed by three reviewers.
Results:
Eight studies were included. Seven had good-to-fair methodological quality, six reported positive effects of ET on motor control (for example, muscle strength or muscle grade) and four also reported positive effects on functional ability. Five of these studies focused on patients with long-lasting SCI. A great variety of therapeutic approaches were applied, even within ET there was a wide range of training characteristics.
Conclusion:
Although ET is a cornerstone in the treatment of the upper extremity in patients with SCI, only a small number of studies were included in the present review. Most of the included studies reported a positive effect of ET on upper extremity motor control and functional ability in SCI patients. As ET is effective in patients with SCI in the chronic stage, this might have implications for the follow up and further treatment of these patients. Future studies should be more specific in describing the characteristics of ET to verify that the ET is in accordance with the current standards for training and motor relearning.
Similar content being viewed by others
Introduction
The worldwide estimate of the prevalence of spinal cord injury (SCI) is 223–755 per million inhabitants, with an incidence of 10.4–83 per million inhabitants per year.1 These prevalence and incidence figures vary widely because of their relationship with local demographic and socioeconomic factors. Fifty percent of the patients with SCI are diagnosed as complete, and in one-third of the patients, the SCI is reported as tetraplegic.1
In tetraplegia, the arm and hand function is affected to varying degrees, depending on the level and severity of the injury. To predict self-care function in cervical SCI, motor level is superior to neurological level.2 Impaired hand function typically results in reduced independence with respect to performance of the activities of daily living and limits participation in socioeconomic activities.1, 3, 4, 5 Studies have shown that improvement in upper extremity function is one of the greatest needs in patients with tetraplegia.6, 7
Spontaneous recovery of motor function below the initial neurological level occurs in almost all SCI patients and depends on several factors.8
First, the completeness of the lesion.8, 9, 10 In patients with a complete SCI, motor function return occurs mainly within the zone of partial preservation. The recovery in patients with incomplete lesions is more substantial, and highly variable compared with patients with complete lesions.8
Secondly, the initial strength of the partly denervated muscle is a significant predictor of motor recovery to useful strength (grade 3 or higher on the Medical Research Council (MRC) Motor Strength Scale).9 Recovery in muscles with some voluntary function is both faster and more complete than in muscles that initially had no function.8 In addition, rapid onset of strength recovery is a good predictor.9
Thirdly, there is some evidence that the motor grade of the functional level, which was initially classified as lowest, influences the probability of the return of function in the level below.8, 11 Approximately 70–80% of motor-complete tetraplegic patients with some motor strength (MRC motor score grade 1–2) in the zone of injury could recover to the next neurological level within 3–6 months, whereas only 30–40% of patients with no motor strength (MRC motor score grade 0) in the zone of injury would gain a level during the same period.10
The final factor influencing the rate of spontaneous recovery is the time since injury.8, 9, 10 The vast majority of spontaneous recovery (77%) takes place in the first 3 months, with a small amount of further recovery up to 18 months and occasionally longer.8
To enhance function and independence after injury, intensive rehabilitation therapy for the upper extremities in tetraplegic patients is considered to be very important.6, 12, 13 A cornerstone of rehabilitation is exercise therapy (ET). In this respect, ET was defined as a series of movements with the aim to improve the upper extremity motor control (that is, muscle strength or muscle grade) and functional ability (that is, activities of daily living).
The main objective of this review is to investigate the effects of ET on the upper extremity motor control and functional ability of SCI patients by means of a systematic analysis of the literature.
Methods
Literature search
This review is based on a systematic literature search of studies published from January 1964 to April 2007 in the databases of PubMed, the Cochrane Library, EMBASE, the Center for International Rehabilitation Research Information and Exchange (CIRRIE) and the National Rehabilitation Information Center for Independence (REHABDATA). The following keywords were used in this search: spinal cord injury, SCI, spinal cord lesion, quadriplegia, exercise, exercise therapy, rehabilitation therapy, motor recovery, motor power, muscle strengthening, recovery of function and upper extremity. This strategy was adjusted for searching the other databases. In addition to searching the databases, the references of relevant publications were checked.
Study selection
The initial selection of articles was based on title and abstract. Three reviewers (MGMK, GJS and MJAJ) independently selected and summarized the studies and scored their methodological quality. The reviewers met regularly to discuss their findings and decisions. In case of disagreement, consensus was reached by discussion.
To be selected for review, a study had to
-
1)
involve patients with a complete or incomplete cervical SCI;
-
2)
investigate ET, possibly compared with other therapies (that is, electrical stimulation, biofeedback);
-
3)
focus on upper extremity motor control (and possibly functional abilities);
-
4)
be a clinical trial or (randomized) controlled trial; and
-
5)
be reported in a full-length publication in a peer-reviewed journal.
Studies focusing on the application of ET for paraplegic patients or on the lower extremities were excluded. To enable the most complete review of the current literature, the search was not limited by the stages of rehabilitation.
Methodological quality judgement
To obtain insight into the methodological quality of the included trials, the study designs were classified according to Jovell and Navarro-Rubio14 (Table 1).
Data extraction
The analysis of the contents of the selected studies was based on a structured diagram. By constructing this diagram, the general contents of the studies were scanned for:
-
1)
patient characteristics;
-
2)
intervention(s) implemented in the study;
-
3)
outcome measures for the evaluation of the effects; and
-
4)
conclusions based on the results.
The conclusions were considered to be positive if the change between pre- and post-treatment measurement was significant or if there was a significant difference between several groups as calculated by an appropriate statistical test for the research question and the data characteristics. Statistical significance was set at P<0.05.
Results
Selection of studies
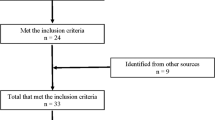
The systematic literature search in PubMed resulted in the identification of 447 studies. Eight of these studies15, 16, 17, 18, 19, 20, 21, 22 fulfilled the selection criteria, and were included in the present review. Additional searches in the Cochrane Library, EMBASE, CIRRIE and REHABDATA databases, and checking the references of relevant publications, resulted in no further inclusions. An overview of the characteristics of the reviewed articles is presented in Table 2.
Methodological quality judgement
Seven15, 16, 17, 18, 19, 21, 22 of the selected studies were small randomized controlled trials with at least a pre- and post-treatment measurement and a methodological score of III, according to Jovell and Navarro-Rubio.14 One study20 was classified as a non-controlled trial with a methodological score of IX. However, patient characteristics and intervention parameters in this study were unclear, and the results and conclusions were incomplete. Therefore, it was excluded from further analysis.
Intervention
In six studies,15, 16, 17, 18, 19, 22 ET was compared with a combination of ET and an additional therapy; three studies16, 17, 18 compared ET with ET in combination with electromyographic feedback; and five studies15, 16, 18, 19, 22 compared ET with ET in combination with various kinds of electrical stimulation. The additional electrical stimulation therapies consisted of somatosensory electrical stimulation of the median nerve,22 neuromuscular stimulation16, 19 and electrical stimulation of partly innervated muscles.15, 18 One study21 focused on the effects of ET in combination with patient education. Table 3 presents the training characteristics of ET in the selected studies.
Patients
The size of the experimental and control groups were comparable in the selected studies and ranged from 522 to 14.17 In six studies,15, 16, 17, 18, 19, 22 the neurological level at baseline ranged from C4 to C7. The study of Hicks et al.21 also included patients with paraplegia, but only the results of the patients with tetraplegia were taken into account in the present systematic review. The time since injury was at least 1 year in six studies.15, 16, 17, 19, 21, 22 Only the study of Kohlmeyer et al.18 contained patients with acute SCI.
Outcome measures
A total of 17 outcome measures were identified across the seven included studies (Table 4). Five studies16, 17, 18, 21, 22 assessed functional outcomes and all seven studies15, 16, 17, 18, 19, 21, 22 assessed motor control. The functional tests consisted of four different outcome measures: self-feeding,16, 17, 18 hygiene and dressing skills,16, 17 mobility16 and upper extremity function.22 Different outcome measures were used to assess motor control. In three studies, the muscle strength was assessed and in five studies the muscle grade. Other outcome measures were quality of life and psychological well-being,21 arm ergometry performance,21 motor-evoked potentials and motor thresholds of the thenar musculature22 and the range of motion of the elbow.15
Content of studies
Six studies16, 17, 18, 19, 21, 22 reported short-term follow-up improvements in motor control or functional ability of the upper extremity as a result of ET, or ET in combination with electrical stimulation or biofeedback (Table 4). Kohlmeyer et al.18 and the two studies of Klose et al.16, 17 compared ET, electrical stimulation and biofeedback. They reported no treatment group superior to any other. Hicks et al.21 reported progressive ET, twice a week to be effective in increasing arm strength, arm ergometry, quality of life and psychological well-being. Beekhuizen and Field-Fote22 concluded that ET is effective in improving strength, which may be further enhanced by the addition of somatosensory stimulation. Needham-Shropshire et al.19 reported neuromuscular stimulation to be more beneficial in improving motor score in patients with a chronic SCI. Only Seeger et al.15 reported no significant improvement in muscle strength after electrical stimulation or conventional exercise in patients with a chronic SCI. None of the studies measured long-term follow-up improvements.
Discussion
Improvement of the upper extremity function is one of the greatest needs in patients with tetraplegia.6, 7 Therefore, an intensive rehabilitation program is considered to be very important to optimize function and functional ability of the upper extremity in these patients.7, 12 Although ET constitutes a substantial part of the upper extremity rehabilitation in SCI patients, only a few controlled trials reported on its effectiveness. Nevertheless, clinical experience has shown that ET is important, for example, to prevent contract and useless hands.23 Seven studies fulfilled the selection criteria, in which ET for the upper extremity was investigated in cervical SCI patients. In this systematic review, they were qualitatively analyzed to assess the effectiveness of ET.
Six studies16, 17, 18, 19, 21, 22 reported positive effects owing to ET, electrical stimulation or biofeedback. Three studies reported positive effects on muscle strength, three studies on muscle grade and four studies on the functional ability of the upper extremity. Five of these studies focused on the chronic stage of SCI. As most of the studies focused on chronic SCI, it is reasonable to presume functional ability and motor control would not change to a great extent without therapy. This is in accordance with the findings of Hicks et al.,21 they reported no significant change in the upper extremity function in the control group of chronic SCI patients receiving education only.
A plausible explanation for motor function improvement in the chronic stage is reorganization of the brain and spinal cord.22, 24 In this respect, a distinction must be made between skill training and strength training. Skill training induces synaptogenesis, synaptic potentiation and the reorganization of movement representations within the motor cortex. Strength training alters spinal motoneuron excitability and induces synaptogenesis within the spinal cord.24 All training experiences induce changes in spinal reflexes, which are dependent on the specific demands of the task.24 Finally, functional activities can also be improved by learning and using compensatory strategies.17
In the acute stage of SCI, it is difficult to differentiate between spontaneous recovery and the effects of ET. However, it appears reasonable that the principles of maximizing the function of spared fibers and the reorganization of the brain and spinal cord, as mentioned for chronic SCI patients, also apply to acute SCI patients.
Although the quality of the studies was good to fair, a potential bias in these research findings is the small number of patients and the lack of control groups. Four studies did not include a control group and remarkable is that, three studies used the ET group as control group. Another potential bias is the great variety in outcome measures, which makes it difficult to compare the results between studies.
The exact characteristics (for example, content) of ET were not described in detail in every study. Also the intensity of ET is not clear in all cases and varies between the studies. Furthermore, the type of exercise differs between studies. This makes it difficult to compare ET between the studies, as different types of exercise will lead to dissimilar recovery. The incomplete description of ET makes it difficult to check whether ET is in accordance with the principles of training and the key variables of motor learning.
The three principles of training, namely overload, specificity and reversibility, are important. Overload states that for an effect of training to occur, a system or tissue must be challenged with an intensity, duration and frequency of exercise to which it is not adjusted. The principle of specificity indicates that the training effect is limited to the system and tissues involved in the activity.25 Reversibility is a consequence of the overload principle, and indicates that the gains are quickly lost when the overload is removed. The most important variable affecting the learning of motor skills is the intensity of practice itself.26 According to the intensity of practice, motivation also plays an important role in learning. If the level of motivation is too low, people may not be sufficiently motivated to practice at all, and no learning will occur. Information about performance, that is, feedback, is the single most important variable for motor learning. Augmented feedback (information in addition to intrinsic sensory feedback that comes from an external source to the person performing the skill)27 appears to have several possible mechanisms for enhancing learning.28 It acts as information, forms associations between movement parameters and the resulting action, can have a motivational role29 and will also enhance the cortical changes associated with motor learning.30 In addition to these independent variables affecting the learning of motor skills, the structure of practice is also important. Intensity, task specificity and goal-orientated practice are important principles of motor control.31 Further studies should provide systematic information about these aspects.
Interesting technological innovations in rehabilitation could make it easier to control and report these variables. Virtual reality is a promising modality for the creation of favorable practice environments in neurorehabilitation.32 By means of virtual reality in rehabilitation it is possible to focus on different key concepts of motor (re-)learning: repetitive practice, feedback about performance and motivation.30 Advantages of the use of virtual reality is the ability to make tasks easier, less dangerous, more fun, more challenging and easier to learn because of the salient feedback that can be provided during practice.30, 32 Although the amount of practice is an important variable for motor learning, variations in direction, timing and speed are needed to optimize the development of skills. These variations can be controlled with virtual reality.32 Moreover, humans can learn motor skills in a virtual environment and transfer the motor learning to the real world.33
In addition to virtual reality, robotics is intended to be an adjunctive tool to increase the intensity of therapy. By means of these devices, it is possible to support the arm (compensation of gravity). This facilitates arm movements that enable patients to perform more training repetitions.34
Conclusion
Although ET is a cornerstone in the treatment of upper extremity in patients with SCI, only a small number of clinical and randomized controlled trials were found in literature. Most of the studies reported a positive effect of ET on upper extremity motor control and functional abilities in SCI patients. As ET is effective in patients with SCI in the chronic stage, this might have implications for the follow-up and treatment of these patients. Future studies should be more specific in describing the characteristics of ET to verify ET is in accordance with the current standards for training and motor relearning.
References
Wyndaele M, Wyndaele JJ . Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord 2006; 44: 523–529.
Marino RJ, Rider-Foster D, Maissel G, Ditunno JF . Superiority of motor level over single neurological level in categorizing tetraplegia. Paraplegia 1995; 33: 510–513.
Beekhuizen KS . New perspectives on improving upper extremity function after spinal cord injury. J Neurol Phys Ther 2005; 29: 157–162.
Ditunno Jr JF, Cohen ME, Hauck WW, Jackson AB, Sipski ML . Recovery of upper-extremity strength in complete and incomplete tetraplegia: a multicenter study. Arch Phys Med Rehabil 2000; 81: 389–393.
Harvey LA, Batty J, Jones R, Crosbie J . Hand function of C6 and C7 tetraplegics 1–16 years following injury. Spinal Cord 2001; 39: 37–43.
Snoek GJ, IJzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F . Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004; 42: 526–532.
Anderson KD . Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004; 21: 1371–1383.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007; 45: 190–205.
Ditunno JF, Flanders AE, Kirshblum S, Granziani V, Tessler A . Predicting outcome in traumatic spinal cord injury. In: Kirshblum S, Campagnolo, Delisa (eds). Spinal Cord Medicine. Lippincott Williams and Wilkins: Philadelphia, 2007, pp 108–122.
Ditunno Jr JF, Stover SL, Freed MM, Ahn JH . Motor recovery of the upper extremities in traumatic quadriplegia: a multicenter study. Arch Phys Med Rehabil 1992; 73: 431–436.
Ditunno Jr JF . The John Stanley Coulter Lecture. Predicting recovery after spinal cord injury: a rehabilitation imperative. Arch Phys Med Rehabil 1999; 80: 361–364.
Kirshblum S, Ho CH, House JG, Druin E, Nead C, Drastal S . Rehabilitation of spinal cord injury. In: Kirshblum S, Campagnolo, Delisa (eds). Spinal Cord Medicine. Lippincott Williams and Wilkins: Philadelphia, 2001, pp 275–298.
Murphy CP, Chuinard RG . Management of the upper extremity in traumatic tetraplegia. Hand Clin 1988; 4: 201–209.
Jovell AJ, Navarro-Rubio MD . Evaluation of scientific evidence. Med Clin (Barc) 1995; 105: 740–743.
Seeger BR, Law BM, Creswell JE, Stern LM, Potter G . Functional electrical stimulation for upper limb strengthening in traumatic quadriplegia. Arch Phys Med Rehabil 1989; 70: 663–667.
Klose KJ, Schmidt DL, Needham BM, Brucker BS, Green BA, Ayyar DR . Rehabilitation therapy for patients with long-term spinal cord injuries. Arch Phys Med Rehabil 1990; 71: 659–662.
Klose KJ, Needham BM, Schmidt D, Broton JG, Green BA . An assessment of the contribution of electromyographic biofeedback as an adjunct therapy in the physical training of spinal cord injured persons. Arch Phys Med Rehabil 1993; 74: 453–456.
Kohlmeyer KM, Hill JP, Yarkony GM, Jaeger RJ . Electrical stimulation and biofeedback effect on recovery of tenodesis grasp: a controlled study. Arch Phys Med Rehabil 1996; 77: 702–706.
Needham-Shropshire BM, Broton JG, Cameron TL, Klose KJ . Improved motor function in tetraplegics following neuromuscular stimulation-assisted arm ergometry. J Spinal Cord Med 1997; 20: 49–55.
Schalow G . Recovery from spinal cord injury achieved by 3 months of coordination dynamic therapy. Electromyogr Clin Neurophysiol 2002; 42: 367–376.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003; 41: 34–43.
Beekhuizen KS, Field-Fote EC . Massed practice versus massed practice with stimulation: effects on upper extremity function and cortical plasticity in individuals with incomplete cervical spinal cord injury. Neurorehabil Neural Repair 2005; 19: 33–45.
Bedbrook G . The Care and Management of Spinal Cord Injury. Springer Verlag: New York, Heidelberg, Berlin, 1981.
Adkins DL, Boychuk J, Remple MS, Kleim JA . Motor training induces experience-specific patterns of plasticity across motor cortex and spinal cord. J Appl Physiol 2006; 101: 1776–1782.
Powers SK, Howley ET (eds). The physiology of training: effect on VO2 max, performance, homeostasis, and strength. In: Exercise Physiology, Theory and Application to Fitness and Performance, 5 edn. McGraw-Hill: New York, 2004, pp 249–275.
Schmidt RA, Lee TD . Condition of practice. In: Motor Control and Learning: A Behavioural Emphasis, 4 edn. Human Kinetics: Champaign, IL, 2005.
Magill RA . Augmented feedback. In: Motor Learning and Control: Concepts and Applications, 7 edn. McGraw-Hill: New York, 2004.
van Dijk H, Jannink MJ, Hermens HJ . Effect of augmented feedback on motor function of the affected upper extremity in rehabilitation patients: a systematic review of randomized controlled trials. J Rehabil Med 2005; 37: 202–211.
Schmidt RA, Lee TD . Augmented feedback. In: Motor Control and Learning: A Behavioural Emphasis, 4 edn. Human Kinetics: Champaign, IL, 2005.
Holden MK . Virtual environments for motor rehabilitation: review. Cyberpsychol Behav 2005; 8: 187–211.
Hesse S, Schmidt H, Werner C, Bardeleben A . Upper and lower extremity robotic devices for rehabilitation and for studying motor control. Curr Opin Neurol 2003; 16: 705–710.
Stewart JC, Yeh SC, Jung Y, Yoon H, Whitford M, Chen S-Y et al. Intervention to enhance skilled arm and hand movements after stroke: a feasibility study using a new virtual reality system. J Neuroeng Rehabil 2007; 4: 21.
Standen PJ, Cromby JJ . Can students with developmental disability use virtual reality to learn skills which will transfer to the real world? Paper presented at the Virtual Reality and Persons with Disabilities Conference 1995, San Francisco, CA.
Jannink MJA, Prange GB, Stienen AHA, Van der Kooij H, Kruitbosch JM, IJzerman MJ et al. Reduction of muscle activity during repeated reach and retrieval with gravity compensation in stroke patients. Proceedings of the 10th International Conference on Rehabilitation Robotics (ICORR) June 13–15, 2007, Noordwijk aan Zee, the Netherlands, pp 472–476 (doi:10.1109/ICORR.2007.4428468).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kloosterman, M., Snoek, G. & Jannink, M. Systematic review of the effects of exercise therapy on the upper extremity of patients with spinal-cord injury. Spinal Cord 47, 196–203 (2009). https://doi.org/10.1038/sc.2008.113
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.113
Keywords
This article is cited by
-
Treatment of shoulder pain in people with spinal cord injury who use manual wheelchairs: a systematic review and meta-analysis
Spinal Cord (2022)
-
Safety and efficacy of transcranial direct current stimulation in upper extremity rehabilitation after tetraplegia: protocol of a multicenter randomized, clinical trial
Spinal Cord (2022)
-
Rehabilitation of hand function after spinal cord injury using a novel handgrip device: a pilot study
Journal of NeuroEngineering and Rehabilitation (2017)
-
Eye-tracking computer systems for inpatients with tetraplegia: findings from a feasibility study
Spinal Cord (2015)
-
Is body weight-support treadmill training effective in increasing muscle trophism after traumatic spinal cord injury? A systematic review
Spinal Cord (2015)