Abstract
Study design:
Prospective study.
Objectives:
The primary objective of neurophysiological monitoring during surgery is to prevent permanent neurological sequelae. To avoid neurological injury, we applied somatosensory-evoked potentials (SEPs) and/or motor-evoked potentials (MEPs). We evaluated whether the combination of SEP and MEP for spinal surgery may be beneficial.
Setting:
Asian Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
Methods:
Combined SEP/MEP monitoring was attempted in 100 consecutive procedures for spinal operations. Trains of transcranial electrical stimulation over the motor cortex were used to elicit MEPs from the muscles of the upper/lower limbs. The tibial and median nerves were stimulated to record SEP.
Results:
Combined SEP/MEP recording was successfully achieved in 85 of 100 operations. In 61 of 85 operations (71%), SEP and MEP were stable, and all patients remained neurologically intact after surgery. Significant MEP changes were recorded in 20 operations, either combined with (n=4) or without (n=16) SEP changes. In 7 of these 20 operations, MEP recovered to some extent after surgical intervention, and these patients showed no neurological changes. In the remaining 13 operations, MEP did not recover and the patients had a transient (n=4) or a permanent (n=3) motor deficit. Significant SEP changes with stable MEP were observed in four operations, all of which were not related to postoperative motor deficit.
Conclusion:
Combined SEP/MEP monitoring provided higher sensitivity and higher positive/negative predictive value than single-modality monitoring techniques. Detection of MEP changes and adjustment of surgical strategy may prevent irreversible pyramidal tract damage.
Similar content being viewed by others
Introduction
Recent advances in technology and neurophysiological methodologies have significantly altered intraoperative neurophysiological monitoring (IOM) during spinal and spinal cord surgery. Somatosensory-evoked potentials (SEPs) were first used about 30 years ago to monitor the spinal cord during surgical correction for scoliosis.1, 2 Despite preservation of SEPs, however, serious motor deficits were observed, thus bringing into question their capacity to monitor spinal cord motor tracts.
More recently, transcranial, electrically elicited, motor-evoked potentials (Tc-MEPs) have been used to assess the integrity of motor tracts during removal of spinal cord tumors, correction of scoliosis and cervical spine surgery.3, 4, 5, 6 Combined SEP/MEP monitoring has several theoretical advantages over each alone, including the ability to monitor a larger number of patients, the increased accuracy provided by complementary information from two independent systems with a reduced risk of false negatives and perhaps an increased sensitivity in detecting early spinal cord dysfunction.7
To assess whether combined monitoring had any advantages over a single method, as well as to determine its effects on intraoperative patient management, we compared the intraoperative changes of myogenic Tc-MEPs, SEPs and both together with the neurological outcome of spinal surgery. We also determined the reliability and applicability of multimodal MEP and SEP monitoring during spine and spinal cord surgeries in our institution.
Materials and methods
Patient data
Between September 2005 and June 2008, intraoperative SEP/myogenic Tc-MEP monitoring was attempted during 100 consecutive operations (10 anterior, 90 posterior) in 98 patients with spinal disorders. All operations were performed by a senior spinal surgeon (SCR). Of these 98 patients, 52 were men and 46 were women; their median age was 49 years (range 13–71 years). Two patients each underwent two operations during this period. Patient diagnoses are listed in Table 1. Preoperatively, 83 patients were neurologically intact and 15 had mild to severe neurological deficits. The study was approved by the ethics committee of the local hospital.
Anesthesia management
Anesthesia was maintained with continuous infusion of propofol (10 mg kg−1 per h) and remifentanil (0.25 μg kg−1 per min). A single bolus of nondepolarizing short-acting muscle relaxant (rocuronium) was given at induction to facilitate tracheal intubation and ventilation. No paralytic agents were used after induction and intubation. The level of neuromuscular block was monitored by recording the compound muscle action potentials (CMAPs) to a train of four stimuli. Invasive blood pressure, electrocardiogram (ECG), end-tidal carbon dioxide concentration (ETCO2), pulse oximetry and temperature were monitored.
Intraoperative SEPs
Stimulation of SEP was accomplished with square-wave electrical pulses of 0.3 ms duration and a maximum intensity of 25 mA at a frequency of 5 Hz. Surface stimulating electrodes were placed over each median nerve at the wrist and over each posterior tibial nerve at the ankle. Evoked potentials were recorded in a referential fashion from the C3 (right median nerve stimulation), C4 (left median nerve stimulation) and Cz (right and left tibial nerve stimulation) positions and from a reference electrode at FPZ (international 10–20 system).
Intraoperative MEPs
Multipulse transcranial electrical stimulation was performed using a commercially available IOM electrical stimulator (Neuropack MEB-9200K; Nihon Kohden Co., Tokyo, Japan). Disc electrodes (9 mm) were attached to the scalp with collodion 6 cm anterior to Cz and at C3 and C4 (International 10–20 system). Trains of either four or five pulses (individual stimulus duration 50 ms) with interstimulus intervals of 2, 3 or 4 ms were used, depending on which provided the best recording, with a period of at least 30 s between two successive trains. Stimulus intensity was gradually increased (50 V increments from 100 V to a maximum of 600 V) until MEP amplitudes were maximized above a minimum of 20 mV. MEPs were recorded simultaneously from the tibialis anterior and abductor hallucis muscles of both legs and from the abductor pollicis muscles of both arms using a pair of noninsulated subcutaneous needle electrodes inserted 3 cm apart in each muscle.
Electrophysiological monitoring
Neurophysiological monitoring was performed throughout surgery. Baseline readings were obtained before skin incision and for intradural surgery after opening of the dura mater. Waveforms were analyzed for latency and peak-to-peak amplitude. Stimulation was alternated between SEP and MEP in continuous order. SEP amplitude reductions of >50% of baseline values and latency increases >10% were regarded as significant.8 During propofol maintenance anesthesia, MEP amplitude decrements >50% of baseline values were considered indicative of significant change, providing the levels of neuromuscular blockade and general anesthesia were unchanged.7, 8 CMAPs were recorded either before or after each MEP trial. The surgical team was immediately informed of any significant IOM changes. The operation was paused or the surgical strategy was modified in every case of IOM changes.
Patient outcomes, statistical analysis
The neurological state of each patient was evaluated before surgery, immediately after surgery and 7 days and 6 weeks later. For statistical analysis, SPSS software (version 12.0, 2003; SPSS Inc., Chicago, IL, USA) was used. The paired t-test was used for statistical analysis of the differences in noncategorical variables between intraoperative factors and neurological sequelae. Possible univariate association between intraoperative factors and EP changes was tested using Spearman's rank correlation coefficients. A P-value less than 0.05 was considered statistically significant.
Results
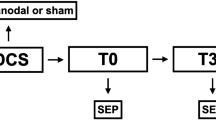
None of the patients had epileptic attacks during or after surgery, and there were no burn marks at stimulation sites. No response to either modality could be recorded in 4 of the 100 procedures; all of these patients had severe preoperative neurological deficits. Either MEP or SEP monitoring was possible in 11 procedures. Overall, EP monitoring was possible in 96 operations (Figure 1), with SEPs monitored in 93 and MEPs in 88. During eight operations, only SEPs could be reliably recorded, whereas only MEPs could be obtained in one patient with a cervical spondylotic compressive myelopathy and in two patients with intradural extramedullary (IDEM) schwannomas.
Combined SEP/MEP monitoring
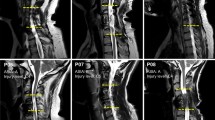
Combined SEP/MEP monitoring was possible in 85 operations, remaining unchanged in 61 (71%). None of these patients had a new postoperative neurological deficit. Significant SEP changes with stable MEP occurred during only four procedures (5%), with one patient having a transient hypesthesia, but no motor deficit, after surgery. Significant MEP changes but stable SEPs were recorded in 16 of the 85 operations (19%). A >50% decrease in amplitude with complete or incomplete recovery was the most frequent change (Figure 2). Three patients sustained a transient (Figure 3) and one a permanent motor deficit. Simultaneous significant SEP/MEP deteriorations were observed in 4 of 85 procedures (5%). In all four procedures, MEP changes were detected earlier than SEP alterations. In two patients, MEP and SEP were lost bilaterally, and both had permanent motor deficits after surgery. Unilateral MEP loss with significant SEP deterioration was observed in the other two patients. The patient with irreversible unilateral MEP loss had a transient motor and sensory deficit, whereas the patient with reversible changes had no neurological deficits (Table 2).
(a) Tracing of somatosensory-evoked potential (SEP) (left panel) and motor-evoked potential (MEP) (middle panel) during the critical stage of the operation. Deterioration of MEP with stable SEP occurred during instrumentation. MEP monitoring prompted a temporary halt of instrumentation, correction hypotension with full recovery of the amplitude. Thereafter, instrumentation was continued. The patient was neurologically intact after surgery. CT 2D sagittal reconstructed image (b) and T2-weighted MRI (c) showing a Klippel–Feil syndrome with signal change of the spinal cord. TN, tibial nerve; AP, abductor pollicis muscle.
Tracing of somatosensory-evoked potential (SEP) (a) and motor-evoked potential (MEP) (b) during the critical stage of the operation. Unilateral loss of MEP was accompanied by stable SEP and no recovery. A transient motor deficit of right hand occurred postoperatively. (c) T1-weighted gadolinium-enhanced MRI demonstrating a recurrent intramedullary spinal cord tumor (histology: clear cell carcinoma). TN, tibial nerve; AP, abductor pollicis; TA, tibialis anterior muscle.
Sensitivity and specificity
Overall, a postoperative motor deficit was observed in seven patients, with paresis being transient in four and permanent in three. All of these new motor deficits were detected by MEP monitoring, making the sensitivity of MEP 100%. Significant MEP changes were seen in 20 operations, but a postoperative motor deficit was detected only in 7, making the specificity of MEP 35%. SEP monitoring detected new motor or sensory deficits in four out of eight operations, making its sensitivity 50%. Significant SEP changes occurred during eight procedures, with three patients sustaining postoperative motor deficits and one patient a postoperative hypesthesia. The SEP specificity in our series was 50%.
Risk factors for neurological complications
The incidence of neurological sequelae was higher in patients with abnormal preoperative neurology (6/15 vs 2/83; P<0.000) and in those with spinal tumors (7/70 vs 1/28; P=0.013). Although no neurological complications occurred in patients with extradural tumors, new postoperative deficits developed in five patients with intramedullary spinal cord tumors (IMSCTs) and in two with IDEM spinal cord tumors. Of the patients without tumors, only one experienced neurological sequelae, accompanied by ossification of the ligamentum flavum in the thoracic spine (Table 3). There was no significant correlation between neurological sequelae and either the type of spinal operation (anterior vs posterior) or intraoperative factors, such as ECG, ETCO2, temperature, blood pressure and instrumentation. No correlation was observed between any of the above factors, except systemic hypotension, and the incidence of intraoperative EP changes that were not complicated by neurological sequelae. Correction of systemic hypotension was correlated with the rate of recovery from intraoperative EP deterioration not associated with postoperative neurological deficits (P=0.037).
Surgical impact of combined IOM
Combined IOM resulted in alteration of surgical strategy in all cases with significant potential changes. MEP deterioration prompted a pause and a thorough inspection of the operation site after exclusion of external factors as a cause of amplitude reduction (mean arterial pressure, hemoglobin, hematocrit, technical problems and so on). Depending on the procedure and the cause of positive recordings, we took specific measures (Table 3).
In the group with IMSCT (n=13), reactions to MEP deterioration typically include temporary or definite halt of resection, temporarily ceasing the retraction of the dorsal columns, rinsing of the operative site with nimodipine. In two operations, we observed that MEP spontaneously recovered after surgery was stopped. In the case with the anaplastic astrocytoma, MEP deterioration occurred early in the course of resection. Because there was no recovery of MEP, only partial removal of the tumor was achieved.
On the other hand, MEP amplitude decline occurred near the end of resection during surgery of ependymomas (n=4). After a temporary halt of the surgery, spontaneous recovery of MEP was observed (n=2), and surgery was continued, resulting in complete removal. In one operation, unilateral MEP loss/SEP deterioration occurred during the en bloc resection of the ependymoma. We decided to change the surgical strategy to piecemeal resection, and surgery was continued, resulting in subtotal removal, no postoperative neurological deficit. In the remaining procedure, corrective measures did not promote MEP recovery, and resection was abandoned (Table 3, patient 18).
Corrective maneuvers for IDEM tumors (n=8) consisted of a temporary halt of the surgery, release of retraction and change in the site of resection. Surgical measures resulted in complete recovery of MEP in five operations. Complete removal was achieved in all procedures. One patient with irreversible loss of MEP demonstrated a permanent motor deficit (Table 3, patient 5). There were four procedures with isolated SEP deteriorations. In three operations with SEP deterioration, tumor resections were continued with a pause because of stable MEP. Complete removal was achieved in all procedures, resulting in no postoperative neurological deficit. The remaining case was operated on a cervical intramedullary schwannoma. SEP decline paralleled midline myelotomy. The procedure was continued, and the patient demonstrated a transient hypesthesia of the upper extremity after surgery.
Discussion
The number of patients in whom spinal cord function could be adequately monitored was increased by combining SEPs and MEPs, particularly in patients with preoperative neurological deficits. In our series, spinal cord monitoring was possible by using the alternative modality in three patients with sensory deficits who could not be monitored by SEPs and in eight with motor deficits who could not be monitored by MEPs. We achieved successful monitoring of both modalities in 85% of operations, comparable to rates using different stimulating and recording methods.9, 10 SEPs were recorded in a larger number of operations than MEPs (93 vs 88), but were less sensitive. In 16 patients, only the MEPs changed intraoperatively, with 4 of these patients having motor deficits after surgery. SEP changes were never observed in the absence of MEP changes. The higher sensitivity (relative to SEPs) of MEPs to spinal cord dysfunction is consistent with previous reports.11, 12, 13, 14 There were no false negative SEPs or MEPs but 6 (75%) false-positive SEPs and 13 (65%) false-positive MEPs.
Corrective measures when MEPs deteriorate
In this study, correction of systemic hypotension was correlated with the rate of recovery from intraoperative EP deterioration. On the average, the mean arterial blood pressure was elevated to 91 mm Hg to facilitate an increase in spinal cord blood flow. If neurophysiological signals failed to improve following elevation of the mean arterial blood pressure, applied correction was reduced or anchoring hardware was removed. If there still was no indication of adequate signal improvement, a steroid bolus could be administered.15 Finally, if there was no noticeable neurophysiological improvement in response to all other forms of intervention, the spinal implant was removed or tumor resection was abandoned.
Criteria for MEP interpretation
MEP recordings are considered stable if changes are <50% in amplitude.16, 17, 18 In this study, we used 50% instead of 80% or the absence/presence criteria because epidural D-wave recordings were not available during most procedures. By applying the 50% criterion, there were no false negative results but the rate of false positives, defined as patients neurologically intact postoperatively despite intraoperative MEP changes, was >60%. Had we applied the 80% criterion, two patients with postoperative motor deficits would have been missed, but the rate of false-positive results would have been reduced to about 20%. The combined use of epidural D-wave recording and muscle MEPs (mMEPs) is probably the optimal way to assess motor pathways during spinal cord surgery.19 Applying absence/presence criteria and the epidural D-wave recording could reduce the rate of false-positive results.20
A free-running electromyogram (EMG) may also be used to detect early motor tract injury during spinal cord tumor surgery.21 We recently use a combined MEP/SEP and free-running EMG monitoring during spine and spinal cord surgery, and we have repeatedly observed that intraoperative EMG changes without EP changes and EMG changes precede the EP changes. These observations suggest that free-running EMG criteria may improve the reliability of IOM during spinal cord surgery, but require confirmation by a prospective controlled trial on a larger group of patients.
Does the use of monitoring improve the functional outcome?
The real impact of IOM on the neurological outcome after spinal surgery remains debated and very difficult to prove based on control studies. In fact, those spinal surgeons who operate with the assistance of IOM, and believe in its efficacy to prevent neurological deficit, would not accept a prospective randomized study given the ethical and medico-legal concerns of designating a ‘control group’. A limitation of this study is that our study design was not a randomized and controlled one. This question has been answered by a historical control study in patients from Sala with IMSCT.19 The result was a neurological outcome advantage for the monitored group. Extent of resection did not differ in both groups, documenting that the use of monitoring does not make the surgeon too ‘timid’ to proceed until a tumor resection is, indeed, complete.
Conclusion
We used the combined IOM of SEP and mMEPs elicited by transcranial electrical stimulation in a consecutive series of 85 surgically treated spinal disorders. This combination provided higher sensitivity and positive and negative predictive values than each single modality alone. Detection of MEP changes and adjustment of the surgical strategy may prevent irreversible pyramidal tract damage. Furthermore, stable IOM recordings are encouraging the surgeon to proceed with spinal procedures.
References
Nash Jr CL, Lorig RA, Schatzinger LA, Brown RH . Spinal cord monitoring during operative treatment of the spine. Clin Orthop Relat Res 1977; 126: 100–105.
Engler GL, Spielholz NJ, Bernhard WN, Danziger F, Merkin H, Wolff T . Somatosensory evoked potentials during Harrington instrumentation for scoliosis. J Bone Joint Surg 1978; 60: 528–532.
Deletis V, Sala F . Intraoperative neurophysiological monitoring during spine surgery: an update. Curr Opin Orthop 2004; 15: 154–158.
MacDonald DB, Al Zayed Z, Khoudeir I, Stigsby B . Monitoring scoliosis surgery with combined multiple pulse transcranial electric motor and cortical somatosensory-evoked potentials from the lower and upper extremities. Spine 2003; 28: 194–203.
DiCindio S, Theroux M, Shah S, Miller F, Dabney K, Brislin RP et al. Multimodality monitoring of transcranial electric motor and somatosensory-evoked potentials during surgical correction of spinal deformity in patients with cerebral palsy and other neuromuscular disorders. Spine 2003; 28: 1851–1856.
Hilibrand AS, Schwartz DM, Sethuraman V, Vaccaro AR, Albert TJ . Comparison of transcranial electric motor and somatosensory evoked potential monitoring during cervical spine surgery. J Bone Joint Surg Am 2004; 86-A: 1248–1253.
Pelosi L, Lamb J, Grevitt M, Mehdian SM, Webb JK, Blumhardt LD . Combined monitoring of motor and somatosensory evoked potentials in orthopaedic spinal surgery. Clin Neurophysiol 2002; 113: 1082–1091.
Burke D, Nuwer MR, Daube J, Fischer C, Schramm J, Yingling CD et al. Intraoperative monitoring. The International Federation of Clinical Physiology. Electroencephalogr Clin Neurophysiol Suppl 1999; 52: 133–148.
Stephen JP, Sullivan MR, Hicks RG, Burke DJ, Woodforth IJ, Crawford MR . Cotrel-Dubousset instrumentation in children using simultaneous motor and somatosensory evoked potential monitoring. Spine 1996; 21: 2450–2457.
Nagle KJ, Emerson RG, Adams DC, Heyer EJ, Roye DP, Schwab FJ et al. Intraoperative monitoring of motor evoked potentials: a review of 116 cases. Neurology 1996; 47: 999–1004.
Calancie B, Harris W, Broton JG, Alexeeva N, Green BA . ‘Threshold-level’ multipulse transcranial electrical stimulation of motor cortex for intraoperative monitoring of spinal motor tracts: description of method and comparison to somatosensory evoked potential monitoring. J Neurosurg 1998; 88: 457–470.
MacDonald DB, Janusz M . An approach to intraoperative monitoring of thoracolumbar aneurysm surgery. J Clin Neurophysiol 2002; 19: 43–54.
Weinzierl MR, Reinacher P, Gilsbach JM, Rohde V . Combined motor and somatosensory evoked potentials for intraoperative monitoring: intra- and postoperative data in a series of 69 operations. Neurosurg Rev 2007; 30: 109–116.
Costa P, Bruno A, Bonzanino M, Massaro F, Caruso L, Vincenzo I et al. Somatosensory- and motor-evoked potential monitoring during spine and spinal cord surgery. Spinal Cord 2007; 45: 86–91.
Schwartz DM, Sestokas AK . A systems-based algorithmic approach to intraoperative neurophysiological monitoring during spinal surgery. Semin Spine Surg 2002; 14: 136–145.
Neuloh G, Pechstein U, Cedzich C, Schramm J . Motor evoked potential monitoring with supratentorial surgery. Neurosurgery 2004; 54: 1061–1070.
Neuloh G, Schramm J . Motor evoked potential monitoring for the surgery of brain tumours and vascular malformations. Adv Tech Stand Neurosurg 2004; 29: 171–228.
Rohde V, Will BE, Hahn G, Bien S, Zentner J . Motor evoked potentials during embolization of arteriovenous malformations for the detection of ischemic complications. Zentralbl Neurochir 1999; 60: 74–80.
Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F et al. Motor evoked potential monitoring improves outcome during surgery for intramedullary spinal cord tumor: A historical control study in 50 patients. Neurosurgery 2006; 58: 1129–1143.
Kothbauer KF, Deletis V, Epstein FJ . Intraoperative monitoring. Pediatr Neurosurg 1998; 29: 54–55.
Skinner S, Nagib M, Bergman T, Maxwell R, Msangi G . The initial use of free-running electromyography to detect early motor tract injury during resection of intramedullary spinal cord lesions. Neurosurgery 2005; 56: 299–314.
Acknowledgements
None of the authors has any financial interest in the subject under discussion in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hyun, S., Rhim, S., Kang, J. et al. Combined motor- and somatosensory-evoked potential monitoring for spine and spinal cord surgery: correlation of clinical and neurophysiological data in 85 consecutive procedures. Spinal Cord 47, 616–622 (2009). https://doi.org/10.1038/sc.2009.11
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.11
Keywords
This article is cited by
-
Intraoperative evoked potentials in patients with ossification of posterior longitudinal ligament
Journal of Clinical Monitoring and Computing (2022)
-
One-stage posterior focus debridement, interbody grafts, and posterior instrumentation and fusion in the surgical treatment of thoracolumbar spinal tuberculosis with kyphosis in children: a preliminary report
Child's Nervous System (2016)
-
Multimodal intraoperative monitoring during intramedullary spinal cord tumor surgery
Acta Neurochirurgica (2015)