Abstract
Study design:
Cross-sectional.
Objective:
To determine the association between leisure-time physical activity (LTPA) and adherence to Eating Well with Canada's Food Guide (CFG) in community-dwelling adults with chronic Spinal Cord Injury (SCI).
Setting:
Ontario, Canada.
Methods:
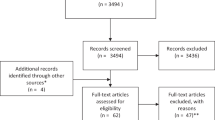
Participants were recruited as part of the Study of Health and Activity in People with SCI (SHAPE-SCI). Dietary data were collected using 24-h recalls and analysed for adherence to CFG recommendations by age group and gender. LTPA was assessed using the Physical Activity Recall Assessment for Persons with SCI. Statistical analysis comprised correlations, multiple regression and χ2.
Results:
We studied 75 adults (n=61 M; 42.4±11.8 years; 25.5±5.2 kg m–2) with chronic (⩾1-year post-injury) SCI. Of these, 37% of participants were inactive, 29% were low-active and 33% were high-active. Fewer than 5% of participants were 100% adherent with CFG; 85% were adherent to ⩽50%. Activity level and overall adherence to CFG were not correlated (r=−0.052, P=0.666). Although there were no associations between LTPA and vegetables and fruit, grain products, milk and alternatives, or other foods (all P>0.05), high activity was associated with consuming less than the minimum number of recommended servings of meat and alternatives (φ=−0.258, P=0.026).
Conclusion:
Clinicians need to be aware of the poor diet quality, and low levels of physical activity, of people with chronic SCI. They should not assume that those who are more active consume better quality diets than those who are low active or inactive.
Sponsorship:
Canadian Institutes of Health Research.
Similar content being viewed by others
Introduction
Improvements in acute care over the past 30 years have led to increases in long-term survival rates in people with spinal cord injury (SCI). A longer life span means that people with SCI risk chronic health problems, including diabetes1 and cardiovascular disease.2 Thus, attenuating risk for chronic disease is important in this population.
Selected lifestyle health behaviours, including consuming a nutritious diet and being physically active, reduce chronic disease risk in able-bodied people.3, 4 Although we have previously reported an association between leisure-time physical activity (LTPA, activity people choose to do in their leisure time) and reduced chronic disease risk factors in those with SCI,5 very little is known about the relationship between LTPA and diet quality in this population. This is not trivial as the able-bodied literature suggests a clustering of lifestyle behaviours; those who are more active consume more nutritious diets, including more fruits and vegetables and fewer servings of meat, than those who are sedentary or low-active.6, 7, 8, 9
Food schemes, such as Eating Well with Canada's Food Guide (CFG),10 assist individuals in ensuring their diets meet nutritional requirements for their age and gender, and allow individuals to plan their diets, maintain a healthy weight and reduce risk of chronic disease. Limited information regarding adherence to food schemes—an indicator of overall diet quality—is available for the SCI population. Tomey et al.11 found men with paraplegia to consume significantly fewer servings of grains, fruit and dairy, but more servings of meat, than able-bodied men enrolled in the 1999–2000 NHANES cohort. These preliminary data suggest that more in-depth study of adherence to food schemes in the SCI population is needed.
Given that physical activity and diet quality are associated in able-bodied people, our objective was to explore the association between LTPA and adherence to CFG in a representative sample of community-dwelling adults with SCI. We hypothesized that higher levels of LTPA would be associated with increased adherence to CFG.
Materials and methods
Participants
The Study of Health and Activity in People with SCI (SHAPE-SCI) is a large (n=696), multi-centre study of physical activity in people with chronic SCI, and for which methods have been published.12 Inclusion criteria required participants to: be residents of Ontario Canada, have obtained a traumatic SCI at least 12 months before participation, be at least 18 years of age, be proficient in written and spoken English, have no self-reported cognitive impairment and rely on the use of a wheelchair when outside the home.
Individuals were invited to participate in a substudy if they lived within a 200-km radius of McMaster University in Hamilton, Ontario, and were able to transfer between a bed and wheelchair. Research ethics boards at the University of Guelph and McMaster University approved the procedures. All participants provided informed consent before being enrolled in the substudy. Participants were remunerated with $10 at the conclusion of the study visit.
Methods
Data for the larger SHAPE-SCI were collected during a pre-scheduled telephone interview conducted on a random day of the week, and included: demographic and impairment details including level of injury (paraplegia vs tetraplegia), health history, predictors of LTPA, reports of secondary complications and well-being, as well as the Physical Activity Recall Assessment for persons with SCI (PARA-SCI).13 The PARA-SCI is a semi-structured telephone questionnaire that measures the type, duration, intensity and frequency of physical activity over a 3-day period, and which is administered by trained research assistants. The scale measures time spent performing lifestyle activities, LTPA and cumulative activity; only LTPA was included in the current analyses. The total number of minutes spent performing mild, moderate and heavy LTPA for the 3-day period was summed and divided by three to yield a daily mean.
If participants were eligible for, and consented to being enrolled in, the substudy, then trained research assistants visited the participants in their homes within 2 weeks of the initial telephone call. The research assistants conducted a 24-h recall with each participant, using food models and the multiple pass method as previously described.14 Dietary data were analyzed using EATracker,15 an online dietary analysis program, which assesses the number of servings consumed for each food group according to Eating Well with CFG.10 EATracker uses typical portion sizes to constitute a serving size (for example, one can of pop). Foods not included in the EATracker database were manually divided into their food group components wherein necessary and added to the total generated by EATracker. The recommended number of servings for each food group of CFG, by age and gender, is shown in Table 1. A participant was considered adherent to a food group if she consumed the minimum number of recommended servings, by age and gender, for that group. To assess overall adherence to CFG, the number of food groups to which a participant adhered was divided by the number of food groups (4) and then converted into a percentage. Participants were thus identified as being 0, 25, 50, 75 or 100% adherent to CFG, representing adherence to the minimum number of recommended servings of 0 of the 4 food groups, or 1, 2, 3 or all 4, respectively. Participants’ intake of other foods was also assessed. Other foods are those not included in any of the four food groups and include items such as jam, pop, potato chips, and so on.10 CFG recommends Canadians limit intake of these foods,10 therefore it was not possible to determine adherence. Instead, the association between LTPA and the number of other foods servings was examined.
Participants were weighed in light clothing and without shoes, using a portable, digital, wheelchair scale (Health O Meter 2450KL, Brooklyn, NY, USA), in kg to the nearest decimal place. They were then transferred from their wheelchairs to a spine board (National Lifesaving Society item EQ-10, Edmonton, AB, Canada) on their beds to provide a hard, flat surface on which to measure length. Length was measured in cm to the nearest decimal place, from crown to heel, using a flexible, non-elastic tape measure. Body mass index was calculated as weight (kg) per length (m2). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Statistical analysis
Data were analyzed using SPSS Version 16.0 (SPSS, Inc., Chicago, IL, USA). A P-value ⩽0.05 was considered significant. Data were assessed for normality; LTPA and intake of other foods were found to be highly skewed. Therefore, when analyzed as a continuous variable, LTPA was transformed using square root. When analyzed as a categorical variable, visual binning was used to create tertiles of the number of minutes of LTPA performed per day (inactive, 0.00 min day–1; low-active, 0.01–26.67 min day–1; high-active, ⩾26.68 min day–1) and of servings of other foods consumed (<6.00, 6.01–11.00 and >11.01). Differences in level of LTPA by level of injury (paraplegia vs tetraplegia) and intake of other foods were examined by χ2 analysis.
Regression analysis was conducted to determine whether a correlation existed between level of LTPA and intake of other foods. Multiple regression analysis was performed to determine correlations between LTPA (expressed as a continuous variable) and overall adherence to CFG (0, 25, 50, 75 or 100%) in one regression, and to the four food groups in a second regression. Crosstab analysis, to calculate the φ coefficient, was performed to determine whether the frequency of adherence to each food group differed by level of LTPA (expressed as a categorical variable).
Results
Characteristics of the study sample are presented in Table 2. The average age of participants was 42.4±11.8 years and the average duration of injury was 15.0±10.5 years. Mean body mass index was 25.5±5.2 kg m–2. A total of 37 participants had paraplegia; the remainder 38 had tetraplegia.
Leisure-time physical activity
Overall, participants engaged in an average of 30.15±45.25 min LTPA day–1, or a median of 10 min day–1 (range 0–260 min day–1). A total of 28 (37%) participants were inactive, 22 (29%) were low-active and 25 (33%) were high-active. Activity differed significantly (χ2=7.75, df=2, P=0.021) by level of injury; more participants with paraplegia (n=18) than tetraplegia (n=7) were high-active. Conversely, 11 participants with paraplegia were inactive compared with 17 participants with tetraplegia. More detailed information regarding duration, types and intensities of LTPA of this sample is described elsewhere.5
Adherence to CFG
Of the whole sample of 75 participants, 8 were 0% adherent to CFG, 33 were 25% adherent, 23 were 50% adherent, 8 were 75% adherent and 3 were 100% adherent. One-quarter (26.7%) of participants were adherent to each of vegetables and fruit and grain products recommendations, one-third (34.7%) to milk and alternatives and two-thirds (65.3%) to meat and alternatives.
Association between LTPA and adherence to CFG
There was no correlation between LTPA and overall adherence to CFG (r=−0.052, P=0.666). Crosstab results presented in Table 3 revealed a negative association between level of LTPA and adherence to meat and alternatives (φ=−0.258, P=0.026), confirmed by multiple regression analysis (B=−2.365, P=0.013). Table 3 revealed no association between LTPA and adherence to the remaining three food groups, also confirmed by multiple regression analysis (fruits and vegetables (B=0.164, P=0.148), grain products (B=−0.052, P=0.656) or milk and alternatives (B=0.193, P=0.102)).
Association between LTPA and intake of other foods
The entire study sample (100%) reported consuming other foods. There was no correlation between LTPA and consumption of Other Foods (r=−0.007, P=0.954). Crosstab results indicated there was no relationship between levels of LTPA and other foods consumed (χ2=2.47, df=4, P=0.649).
Discussion
This is the first study investigating the association between LTPA and adherence to the 2007 Eating Well with CFG in community-dwelling adults with chronic SCI. Participants were poorly adherent to CFG. Although there were no associations between LTPA and overall adherence to CFG, high-active participants did not consume the minimum recommended number of servings of meat and alternatives. There was no association between LTPA and amount of other foods consumed.
We found overall adherence to CFG, and thus diet quality, to be poor. The majority of participants (85%) were ⩽50% adherent to the food scheme; fewer than 5% were 100% adherent. We therefore explored adherence to the minimum number of recommended servings within each food group; these results fared no better. Only one-quarter to one-third of participants were adherent to each of milk and alternatives, vegetables and fruit, and grain products; two-thirds were adherent to meat and alternatives. Interpreting these findings relative to able-bodied adult Canadians is difficult as no data describing adherence to the revised 200710 CFG have yet been published. However, Garriguet16 reported that the average number of daily servings from each of vegetables and fruit and milk products (but not grain products or meat and alternatives) consumed by adult Canadians, as per the 1992 version of CFG, were below recommendations. Concerns regarding diet quality of Canadians appear to extend beyond our sample of community-dwelling adults with chronic SCI.
Nutrients of concern with consistently low intakes of vegetables and fruit, grain products and milk and alternatives include, but are not limited to, dietary fibre (as found, for example, in whole-grain foods and skins of fruit) and bone-related nutrients (for example, calcium and vitamin D, as found in dairy products). Dietary fibre has an important role in managing neurogenic bowel17 and bone-related nutrients are critical for a population already at increased risk for osteoporosis.18 Both dietary fibre and calcium intakes have recently been found to be low in the SCI population.19 Taken together, these results suggest that overall, community-dwelling adults with chronic SCI may be at increased risk for diet-related chronic conditions.
There were no associations between physical activity and either overall adherence to CFG, or to most individual food groups of the Guide. This was unexpected. The null findings are not due to a lack of statistical power; post hoc calculations indicated that we had sufficient participants to detect an association. Alternatively, the lack of variability in food guide adherence (that is, most participants were nonadherent) may have undermined our ability to detect a relationship. However, on close examination of the π coefficients in Table 3 (and with the exception of the high-active and meat and alternatives association), none even approached clinical significance, suggesting a true lack of association between physical activity and adherence to individual food group recommendations. These results not only inform future research, perhaps more importantly, they also point to an urgent need to address the poor diet quality of people with chronic SCI.
The only significant association between LTPA and adherence to individual food group recommendations indicated that high-active participants did not consume the minimum recommended number of servings of meat and alternatives. This finding is not unique to the SCI population; active vs sedentary able-bodied adults have been reported to consume fewer meat servings/less protein.6, 9 We propose two possible reasons for this finding. As meat is high in fat, high-active people may reduce their intake of foods from the meat and alternatives group in an effort to reduce total fat intake; this is supported by the fact that those who engage in LTPA consume significantly less fat (particularly saturated fat, of which meat is an excellent source) than those who are sedentary.9 Also, people with SCI who spend much of their leisure time being physically active may not have the time or energy to prepare meats, the latter which involves unwrapping, seasoning, cooking and finally, cutting.
Strengths and limitations
This is the first study to examine associations between LTPA and overall diet quality, using the updated Eating Well with CFG, in people with chronic SCI. It is important to consider these two lifestyle behaviours together because the incidence of chronic diseases is higher in the SCI population, and yet may be attenuated by clustered lifestyle health behaviours. Use of the Physical Activity Recall Assessment for persons with SCI strengthened our design as it is the first, and currently the only, measure of physical activity specifically designed for use in the SCI population. Food models provided participants with a visual representation of serving sizes, which may have improved accuracy of dietary intake data. The multiple pass method allowed us to gain information about brand names and cooking methods, providing rich detail about each food item consumed. Finally, our sample was larger than that typically included in SCI studies and importantly, mirrored the larger Canadian SCI population with respect to gender distribution and level of injury,20 making our findings generalizable.
We must acknowledge some of the limitations of our study. We are unable to comment on the usual food intakes of our participants as 24-h recalls provide only cross-sectional data. In the absence of a SCI-specific food guide to assess diet quality, we used CFG, which was designed for healthy, able-bodied people. We recognize that no information on nutrient intakes of our sample population is provided; we refer the reader to our recently published paper on this topic.21 Although we included women, the sample size was not large enough to undertake separate analyses by gender. Despite these limitations, we extend the literature by having investigated diet quality relative to LTPA, a grossly understudied area in the SCI literature.
Conclusion
This is the first investigation of the association between LTPA and diet quality in the SCI population. Adherence to Eating Well with CFG was poor, as were physical activity levels. LTPA and overall adherence were not associated. Together, these findings suggest that clinicians should (1) be aware of the overall poor diet quality, and low activity levels, of people with chronic SCI; (2) not assume that those who are more active necessarily consume better quality diets than those who are low-active or inactive; (3) prioritize management of lifestyle behaviours in the care of people living with chronic SCI.
This exploratory study provides a framework for future research, providing insight into the lifestyle health behaviours of people living with SCI. We recommend future studies include larger sample sizes, and investigate any interactive or multiplicative effects of consuming a poor quality diet and partaking in little or no physical activity, on chronic disease risk and secondary complications.
References
Lavela SL, Weaver FM, Goldstein B, Chen K, Miskevics S, Rajan S et al. Diabetes mellitus in individuals with spinal cord injury or disorder. J Spinal Cord Med 2006; 29: 387–395.
Myers J . Cardiovascular disease after SCI: prevalence, instigators, and risk clusters. Topics in SCI Rehab 2009; 14: 1–14.
Aldana SG, Greenlaw RL, Diehl HA, Salberg A, Merrill RM, Ohmine S et al. Effects of an intensive diet and physical activity modification program on the health risks of adults. J Am Diet Assoc 2005; 105: 371–381.
Fung TT, McCullough ML, Newby PK, Manson JE, Meigs JB, Rifai N et al. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr 2005; 82: 163–173.
Buchholz AC, Martin Ginis KA, Bray SR, Craven BC, Hicks AL, Hayes KC et al. Greater daily leisure time physical activity is associated with lower chronic disease risk in adults with spinal cord injury. Appl Physiol Nutr Metab 2009; 34: 640–647.
Matthews CE, Hebert JR, Ockene IS, Saperia G, Merriam PA . Relationship between leisure-time physical activity and selected dietary variables in the Worcester Area Trial for Counseling in Hyperlipidemia. Med Sci Sports Exerc 1997; 29: 1199–1207.
Oppert J-M, Thomas F, Charles MA, Benetos A, Basdevant A, Simon C . Leisure-time and occupational physical activity in relation to cardiovascular risk factors and eating habits in French adults. Public Health Nutr 2006; 9: 746–754.
Gillman MW, Pinto BM, Tennstedt S, Glanz K, Marcus B, Friedman RH . Relationships of physical activity with dietary behaviors among adults. Prev Med 2001; 32: 295–301.
Camoes M, Lopes C . Dietary intake and different types of physical activity: full-day energy expenditure, occupational and leisure-time. Public Health Nutr 2007; 11: 841–848.
Health Canada. Eating Well with Canada's Food Guide. Health Canada: Ottawa, ON, 2007. Publ. 4651.
Tomey KM, Chen DM, Wang X, Braunschweig CL . Dietary intake and nutritional status of urban community-dwelling men with paraplegia. Arch Phys Med Rehab 2005; 86: 664–671.
Martin Ginis KA, Latimer AE, Hicks AE, Buchholz AC, Bray SR, Craven BC et al. Establishing evidence-based physical activity guidelines: methods for the study of health and activity in people with spinal cord injury (SHAPE SCI). Spinal Cord 2008; 46: 216–221.
Martin Ginis KA, Latimer AE, Hicks AL, Craven BC . Development and evaluation of an activity measure for people with spinal cord injury. Med Sci Sports Exerc 2005; 37: 1099–1111.
Gibson RS . Measurement errors in dietary assessment. In: Gibson RS (ed). Principles of Nutritional Assessment, 2nd edn. Oxford University Press: New York, 2005, p 42.
Dietitians of Canada 2008. EATracker [online]. Available from http://www.dietitians.ca/public/content/eat_well_live_well/english/eatracker/backgrounder.asp [accessed 9 September 2009].
Garriguet D . Canadians’ eating habits. Health Rep 2007; 18: 17–32. Statistics Canada, Catalogue 82–003.
Kirk PM, King RB, Temple R, Bourjaily J, Thomas P . Long-term follow-up of bowel management after spinal cord injury. SCI Nurs 1997; 14: 56–63.
Jiang SD, Jiang LS, Dai LY . Mechanisms of osteoporosis in spinal cord injury. Clin Endocrinol (Oxf) 2006; 65: 555–565.
Groah SL, Nash MS, Ljungberg IH, Libin A, Hamm LF, Ward E et al. Nutrient intake and body habitus after spinal cord injury: an analysis by sex and level of injury. J Spinal Cord Med 2009; 32: 25–33.
Canadian Paraplegic Association. Spinal cord injury facts. 2008. http://www.canparaplegic.org/en/SCI_Facts_67/items/6.html [accessed 9 September 2009].
Walters JL, Buchholz AC, Martin Ginis KA . Evidence of dietary inadequacy in adults with chronic spinal cord injury. Spinal Cord 2009; 47: 318–322.
Acknowledgements
We thank the participants; Rebecca Bassett and Iwona Chudzik for their assistance collecting data; and B Catherine Craven, Keith Hayes, Audrey Hicks, Amy Latimer, Mary Ann McColl, Patrick Potter and Karen Smith for critical review of the paper during preparation stages. Funding was provided by the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Knight, K., Buchholz, A., Martin Ginis, K. et al. Leisure-time physical activity and diet quality are not associated in people with chronic spinal cord injury. Spinal Cord 49, 381–385 (2011). https://doi.org/10.1038/sc.2010.103
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.103
Keywords
This article is cited by
-
Nutritional status in chronic spinal cord injury: a systematic review and meta-analysis
Spinal Cord (2019)
-
Self-management interventions for skin care in people with a spinal cord injury: part 1—a systematic review of intervention content and effectiveness
Spinal Cord (2018)
-
Special considerations in the urological management of the older spinal cord injury patient
World Journal of Urology (2018)
-
Self-management interventions to improve skin care for pressure ulcer prevention in people with spinal cord injuries: a systematic review protocol
Systematic Reviews (2016)
-
Vegetable dishes, dairy products and fruits are key items mediating adequate dietary intake for Japanese adults with spinal cord injury
Spinal Cord (2015)