Abstract
Study design:
This was a prospective observational study.
Objectives:
To review airway management of patients with acute cervical spinal cord injury (CSCI) who are admitted to the intensive care unit (ICU) and to develop a classification and regression tree (CART) to direct clinical decision making in airway management.
Setting:
This study was carried out in Australia.
Methods:
All patients with CSCI who required intubation and mechanical ventilation and who were admitted to ICU in three tertiary hospitals in Melbourne between October 2004 and May 2009 and two other interstate hospitals between December 2004 and December 2005 were included. Airway management was recorded.
Results:
A total of 114 patients were included. Tracheostomy insertion occurred in 68 patients (59.7%). Using CART analysis, it was found that the variables forced vital capacity, the volume of pulmonary secretion and gas exchange were predictive of airway management on 82.3% occasions with an 8.7% extubation failure rate.
Conclusion:
A CART can be useful in clinical decision making regarding airway management in CSCI.
Similar content being viewed by others
Introduction
Most patients following acute cervical spinal cord injury (CSCI) require a period of mechanical ventilation1 and clinicians must decide whether to insert a tracheostomy or attempt extubation. Decisions regarding airway management, particularly extubation, have implications for patient outcome.2, 3, 4 The rate of tracheostomy insertion ranges from early reports of 11–35%5 to recent reports of up to 69%.6, 7, 8 The recent higher rate of tracheostomy insertion may be reflective of clinicians’ belief that early insertion is beneficial and the historical absence of established clinical predictors for safe extubation. However, a small case–control study has also suggested that some patients receive a tracheostomy unnecessarily and patients who are extubated and receive intensive physiotherapy have a reduced intensive care unit (ICU) length of stay and a reduction in hospital costs.9
Although the clinical factors that influence airway management in other neuromuscular diseases have been reported,3, 4 they remain unknown in CSCI. The aims of this study were to describe airway management for patients admitted with CSCI to the ICU of three specialist spinal centres (SSCs) and two state trauma services (STS); and to identify the factors that most influence decision making in airway management and to develop and validate a classification and regression tree (CART) to assist decision making in airway management in acute CSCI.
Materials and methods
Subjects
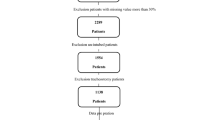
All patients with CSCI who were admitted to an SSC and two STS between October 2004 and May 2009 as well as two other SSC in Australia from December 2004 to December 2005 who required intubation and ventilation were included. To ensure all eligible patients were included, we searched the state SCI database and these data were confirmed by searching the trauma registry. In addition the SSCs provide a state-wide service accepting all patients with SCI in each catchment zone. Patients were excluded if they never required intubation during their ICU stay or if treatment was withdrawn before an airway management decision. Ethical review was obtained from the human research ethics committee at each site.
Procedure
In a nationwide survey, clinicians experienced in the care of patients with CSCI in the ICU were asked to nominate factors that influenced clinical decisions in airway management. In total clinicians identified nine factors (Table 1). These factors were used as the basis of a subsequent data collection form and in the development of the CART that determined which factors best predicted whether patients were extubated or received a tracheostomy.
Demographic and injury data that included injury and neurological level, neurological severity and fracture management were recorded for every patient.
Data collection
For each patient admitted to the trial, the attending intensivist was asked to rank any or all of the factors that influenced clinical decision making in airway management from the nine factors previously identified. The factors that were ranked for each case were entered into analysis.
The nine factors reported to influence clinical decision making identified in the national survey were measured using continuous and ordinal scales (Table 1). The forced vital capacity (FVC) was measured by a spirometer placed in-line with the endotracheal tube. The mental capacity was measured by the performance of three motor tasks and rated on a four-point scale. Neurological level was measured using the highest motor level of the patient as well as the American Spinal Injury Association (ASIA) classification of the injury. Both the neurological motor level and the ASIA classification values were recorded by an independent observer. Sputum production was assessed using a semi-quantitative scale assessed by the frequency of suctioning per hour that has been described previously.10 The greatest numbers of suction passes per hour in the previous 24 h, excluding those associated with physiotherapy treatment, were converted to an ordinal scale and used in analysis. Gas exchange was measured using the PaO2/FiO2.
Statistical analysis
Statistical analyses were undertaken using SPSS PASW version 18 (SPSS Inc., Chicago, IL, USA) and the statistical package R (The R Foundation for Statistical Computing, Vienna, Austria). Descriptive statistics using frequencies and percentages were used to describe categorical data. For continuous data mean and standard deviation or median and inter-quartile range for non-parametric data were recorded. Student's t-tests and Mann–Whitney U-tests were used to determine the differences between groups for continuous variables. Pearson's χ2-test of independence was used to analyse the difference between categorical data.
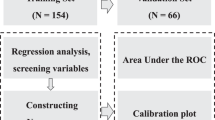
CART analysis was used to determine which of the nine factors were discriminative in airway management. The purpose of the CART is to determine a set of if–then logical splits conditions that permit accurate prediction of classification of cases. The split at each node is found that generates the greatest improvement in predictive accuracy. CART has been previously used for prediction in ICU populations.11 An unbiased estimate of the true misclassification rate was obtained using cross-validation.
In the cohort of patients who received a tracheostomy some were unable to perform an FVC due to sedation or injury above the C4 level. To make clinically meaningful comparisons between groups, we also calculated median FVC for patients who were able to perform the procedure.
To report the results in a clinically meaningful way, we dichotomized the scales for pulmonary secretions and mental capacity. Pulmonary secretions were classified as requiring suctioning hourly or more than hourly (suction ⩽ or >2) and mental capacity as either cooperative or not (mental state ⩽ or >1).
Results
Demographics
From October 2004 to the end of May 2009 141cases were identified of which 114 cases met the inclusion criteria. All eligible cases were included. Of the 114 cases, 68 (59.7%) patients received a tracheostomy and 46 (40.4%) patients were extubated. Of the 114 patients, 36 patients required initial intubation for respiratory failure or airway protection at the time of the injury and 78 patients were initially electively intubated for either transport to a tertiary facility or surgical stabilization. Nine of the thirty-six patients (25%) who required emergent intubation were subsequently able to be extubated. No patient used non-invasive ventilation as an alternative strategy to invasive airway management. The demographic data for the total population and the sub-groups extubated and receiving tracheostomy are presented in Table 2. In the group of patients who received a tracheostomy the median FVC was influenced by the number of patients who were unable to perform the manoeuvre due to either the neurological severity of the injury or an inability to cooperate. If these patients were excluded, and only those who were able to perform an FVC were considered (n=27), the median and interquartile range values for FVC were 1200 ml (800–1500 ml)/17.14 ml kg−1 (11.43–21.43 ml kg−1).
Four patients (8.7%) failed extubation and subsequently received a tracheostomy.
The majority of patients (92%) required surgical stabilization for fracture management. The remaining patients were managed in a halo-thoracic device. All patients managed in a halo-thoracic device received a tracheostomy as part of standard care. Airway management decisions were made in the first 72 h following stabilization surgery and as such, the surgical approach did not impact on the airway management decision.
Airway management
The ASIA classifications for the total population, for patients who were extubated and those who received a tracheostomy are presented in Table 3. The distribution of ASIA classification and injury level is presented in Table 4 and the motor levels of patients who were extubated, those who received a tracheostomy and the total population are presented in Table 5.
For patients suffering an ASIA A injury (n=72), 48 patients received a tracheostomy (66.7%) and in incomplete injuries 47.6% received a tracheostomy. The relationship between airway management and ASIA classification is presented in Figure 1.
All patients with injuries above the C4 level received a tracheostomy (n=12).
Fifty-six patients had injuries between C5 and C8. The relationship between airway management and ASIA classification is presented in Figure 2.
Classification and regression tree
In 18 patients data collection was incomplete. It was assumed that these were missing completely at random. As a result CART analysis was performed on 96 patients.
Of the nine factors identified by clinicians that influenced airway management only FVC (830 ml/11.9 ml kg−1), volume of pulmonary secretions (the requirement for hourly suction) and gas exchange (PaO2/FiO2 188.8) was shown to be important categorical discriminators of airway management (Figure 3). The distribution of patients in the terminal nodes of the classification tree is presented in Table 6.
The overall estimate of correct classification of the CART to predict either tracheostomy or extubation was 86.5%. This estimate is optimistic, being obtained from the same data that were used to generate the classification. The estimate of misclassification obtained from cross-validation corrects for this, and was found to be 82.3%, and hence the estimated misclassification rate was 17.7%. The extubation failure rate was 8.7%. The characteristics of the patients who failed extubation and the reasons for failure are presented in Table 7.
Discussion
Judicious airway management decisions are essential in the ICU. A delayed or failed extubation can result in increased ICU length of stay, ventilator-associated pneumonia, mortality and costs.2 Unnecessarily inserting a tracheostomy places patients at increased risk of complications in the short and long term,12 is costly and may result in an increased length of stay in the ICU.9 The results of this study suggest that a CART that uses FVC, gas exchange and sputum production as discriminative variables has good potential to predict airway management for patients having acute CSCI, was associated with only an 8.7% extubation failure rate and would be a useful tool for clinicians in the ICU.
Previous studies have reported risk factors for the placement of a tracheostomy in patients with CSCI that include the level and neurological severity of the injury, pre-morbid illness, pre-existing pulmonary impairment, the presence of pneumonia and age.6, 7 This is the first study to identify a combination of clinical factors that may discriminate between patients who are extubated and those that received a tracheostomy. The advantage of the CART is that it identifies the most important of the factors that clinicians consider important at the point when decisions are made.
In patients with neurological impairment the use of traditional weaning indices has been associated with high rates of extubation failure.13 Previously Navalesi et al.14 reported that a pragmatic composite assessment that included clinical indicators of cough efficacy, the burden of pulmonary secretions and gas exchange improved clinical decision making in a cohort of neurologically impaired patients. The results of the current study in CSCI support those of Navalesi et al.
Although the model discriminates extremely well for patients with an FVC of less than 830 ml (11.9 ml kg−1) and in the setting of abundant pulmonary secretions and poor gas exchange, classifying extubation remains contentious. This may reflect the variability in clinical decision making surrounding extubation in the data set from which the model was derived and also the small number of patients in the terminal nodes. The split criterion of 830 ml for FVC was lower than previously described for patients who could potentially be extubated. Clinicians may have been reluctant to extubate a patient with an FVC of less than 1000 ml as previously this value was independently associated with extubation failure in patients with neuromuscular impairment.3 The interquartile ranges of FVC for patients who were extubated and those that received a tracheostomy and were able to perform the manoeuvre reflect a zone of uncertainty in airway management between 1000 ml/14.3 ml kg−1 and 1500 ml/21.4 ml kg−1, which was reflected in the model.
Of the 114 patients 59.7% received a tracheostomy that, despite differences in methodology, is consistent with previous reports that have included both complete and incomplete injuries in analyses.6
The overall extubation failure rate was 8.7%, which is comparable to previous reports of between 5 and 20% in heterogeneous ICU populations.15 This is the first report of extubation failure rate in patients with CSCI. The main reasons for extubation failure were related to pulmonary secretion retention and inadequate cough.
Overall this cohort of patients had a higher incidence of ASIA A injuries (63.2%) than previously reported (37.8%).6 This was because in this study, only patients who were intubated at some point during their ICU stay were included. This distinction is important when comparing airway management because, as can be observed in the results of this study and others,6, 7, 8 patients with an ASIA A injury are more likely to require a tracheostomy. Other demographic data were relatively consistent with previous reports.6, 7
The tracheostomy rate in ASIA A injuries was consistent with one previous report,7 but much lower than another.6 These differences may be reflective of the variability in clinical practice associated with airway management in tetraplegia. A further contributing factor may be the level of respiratory support services available at an institution. Intensive respiratory treatment, protocolized care and non-invasive ventilation have been shown to reduce the need for tracheostomy placement.9, 16, 17 Further study is required to investigate the effect of intensive respiratory therapy on airway management in patients with CSCI below the level of C3.
Forty-two patients suffered an incomplete CSCI. The rate of tracheostomy (47.6%) was substantially higher than previously reported (19.2%).6 The only other recent evidence comes from a study exploring airway management in cervical injuries below C4.8 These investigators reported a tracheostomy rate for incomplete injuries of 50%, which was comparable to the current study for the same injury levels (40%). This discrepancy may be explained by the spectrum of injury severity that is encompassed by an incomplete injury. However, this heterogeneity should have been reduced by only including patients who required intubation during the ICU stay. The management of these patients warrants further investigation.
Consistent with previous studies,6, 7 all patients with an injury above the C4 level had a tracheostomy inserted. For these patients there was usually a requirement for ongoing mechanical ventilatory assistance. Owing to respiratory muscle insufficiency, the insertion of a tracheostomy for injuries above the C4 level is accepted as standard practice.18 However, the use of continuous non-invasive ventilation has been advocated for the management of selected high cervical injuries.19 Although non-invasive ventilation has been successfully used in ICU in select patient groups,20 there is little evidence to support the role as an alternative to invasive ventilation in the setting of high CSCI in the ICU. Further research on patient selection, comparison of risk benefit analysis and clinical outcomes would be required for a change in clinical practice to occur.
The most common injury level was C4 and C5 with 75% of all injuries occurring at these levels. The tracheostomy insertion rate for complete injuries at this level was 61.5%, which was substantially lower than previously reported with a rate between 75%7 and 100%.6 This was also observed for lower CSCI between C5 and C8 with a tracheostomy rate of 46% compared with a previous report of 69.3%,8 reflecting a more aggressive approach to extubation in mid-cervical injuries in these Australian centres.
Airway management for lower CSCI requires clinical judgement8 and was the site for the greatest variability in airway management. For patients who received a tracheostomy there was a higher percentage with abundant pulmonary secretions compared with other levels of injuries reflecting the decision making priorities for airway management at levels below C4.
This study has several limitations related to the small sample size. Sample size dictated the development and validation of the model was performed using the same data set potentially resulting in an over-optimistic model. Nonetheless, this cohort represents patients predominantly from a large regional spinal injury service and in contrast to previous studies includes only patients who required intubation and ventilation and in whom airway management decisions were required. The measurement of FVC in CSCI can be limited as some patients are unable to perform the procedure to meet American Thoracic Society guidelines, but are able to meet modified American Thoracic Society guidelines.21 These patients are important to include in future considerations regarding airway management decisions as they represent a vulnerable cohort of patients who are likely to require ICU management with transient ventilatory support following injury.
This study represents the first step in developing a guideline using CART methodology to assist decision making in airway management in CSCI. Further possible studies include the validation of the algorithm on an independent data set at another ICU at an SSC. Potentially, this model will assist judicious decision making regarding airway management for patients with CSCI avoiding unnecessary tracheostomy and unsuccessful extubation that place the patient at increased risk.2, 3, 4, 12 The early identification of patients who require a tracheostomy may also reduce the delay to extubation, which has been shown to affect patient outcomes adversely.2 By facilitating timely airway management decisions the duration of mechanical ventilation and ICU length of stay may be reduced. In addition, it may provide useful information to assist with communication and planning for patients and their families.
References
Velmahos G, Toutouzas K, Chan L, Tillou A, Rhee P, Murray J et al. Intubation after cervical spinal cord injury: to be done selectively or routinely? Am Surg 2003; 69: 891–894.
Epstein SK . Extubation failure: an outcome to be avoided. Crit Care 2004; 8: 310–312.
Nguyen TN, Badjatia N, Malhotra A, Gibbons FK, Qureshi MM, Greenberg SA . Factors predicting extubation success in patients with Guillain–Barré syndrome. Neurocrit Care 2006; 5: 230–234.
Seneviratne J, Mandrekar J, Wijdicks EFM, Rabinstein AA . Predictors of extubation failure in myasthenic crisis. Arch Neurol 2008; 65: 929–933.
Biering-Sorensen M, Biering-Sorensen F . Tracheostomy in spinal cord injured: frequency and follow-up. Paraplegia 1992; 30: 656–660.
Como JJ, Sutton ERH, McCunn M, Dutton RP, Johnson SB, Aarabi B et al. Characterizing the need for mechanical ventilation following cervical spinal cord injury with neurologic deficit.J Trauma 2005; 59: 912–916.
Harrop J, Sharan A, Scheid E, Vaccaro A, Przybylski G . Tracheostomy placement in patients with complete cervical spinal cord injuries: American Spinal Injury Association Grade A. J Neurosurg 2004; 100: 20–23.
Hassid VJ, Schinco MA, Tepas JJ, Griffen MM, Murphy TL, Fryberg ER et al. Definitive establishment of airway control is critical for optimal outcome in lower cervical spinal cord injury. J Trauma 2008; 65: 1328–1332.
Berney S, Stockton K, Denehy L, Berlowitz D . Can early extubation and intensive physiotherapy decrease length of stay of acute quadriplegic patients in intensive care? A retrospective case control study. Physiother Res Int 2002; 7: 14–22.
Mokhlesi B, Tulaimat A, Gluckman TJ, Wang Y, Evan AT, Corbridge TC . Predicting extubation failure after successful completion of a spontaneous breathing trial. Respir Care 2007; 52: 1710–1717.
Trujillano J, Badia M, Serviá L, March J, Rodriguez-Pozo A . Stratification of the severity of critically ill patients with classification trees. BMC Med Res Methodol 2009; 9: 83.
Engels PT, Bagshaw SM, Meier M, Brindley PG . Tracheostomy: from insertion to decannulation. Can J Surg 2009; 52: 427–433.
Frutos-Vivar F, Ferguson ND, Esteban A, Epstein SK, Arabi Y, Apezteguia C et al. Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest 2006; 130: 1664–1771.
Navalesi P, Frigerio P, Moretti MP, Sommariva M, Vesconi S, Baiardi P et al. Rate of reintubation in mechanically ventilated neurosurgical and neurologic patients: evaluation of a systematic approach to weaning and extubation. Crit Care Med 2008; 36: 2986–2992.
Epstein SK . Endotracheal extubation. Respir Care Clin N Am 2000; 6: 321–360.
McMichan J, Michel L, Westbrook P . Pulmonary dysfunction following traumatic quadriplegia. J Am Med Assoc 1980; 243: 528–531.
Tromans AM, Mecci M, Barrett FH, Ward TA, Grundy DJ . The use of the BIPAP bi-phasic positive airway pressure system in acute spinal cord injury. Spinal Cord 1998; 36: 481–484.
Gutteridge GA . Spinal injuries. In: Bersten AD, Soni N (eds). Oh's Intensive Care Manual. Butterwoth Heinemann Elservier: Phildelphia, 2009, 803–813.
Bach J, Hunt D, Horton J . Traumatic tetraplegia noninvasive respiratory management in the acute setting. Am J Phys Med Rehabil 2002; 81: 792–797.
Burns KEA, Adhikari NKG, Keenan SP, Meade M . Use of non-invasive ventilation to wean critically ill adults off invasive ventilation: meta-analysis and systematic review. Br Med J 2009; 338: b1574.
Kelley A, Garshick E, Gross ER, Lieberman SL, Tun CG, Brown R . Spirometry testing standards in spinal cord injury. Chest 2003; 123: 725–730.
Acknowledgements
We thank Dr Geoff Gutteridge for his editorial assistance and the Victorian Neurotrauma Initiative for their fellowship support to Susan Berney.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Berney, S., Gordon, I., Opdam, H. et al. A classification and regression tree to assist clinical decision making in airway management for patients with cervical spinal cord injury. Spinal Cord 49, 244–250 (2011). https://doi.org/10.1038/sc.2010.97
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.97
Keywords
This article is cited by
-
The feasibility of using mouthpiece ventilation in the intensive care unit for post-extubation breathing support after acute tetraplegia
Spinal Cord (2023)
-
Classification and regression tree (CART) model to assist clinical prediction for tracheostomy in patients with traumatic cervical spinal cord injury: a 7-year study of 340 patients
European Spine Journal (2022)
-
Current Topics in the Management of Acute Traumatic Spinal Cord Injury
Neurocritical Care (2019)
-
Classification and regression tree model for predicting tracheostomy in patients with traumatic cervical spinal cord injury
European Spine Journal (2017)
-
A novel crossover operator based on variable importance for evolutionary multi-objective optimization with tree representation
Journal of Heuristics (2015)





 =discriminating variables from the CART analysis.
=discriminating variables from the CART analysis.