Abstract
Study design:
Retrospective case series.
Objectives:
The objective of this study is to identify imaging and intraoperative characteristics that may predict surgical resection for myxopapillary ependymoma (MPE). The diffuse involvement in the conus–filum region makes complete resection challenging. The preoperative characteristics that may estimate the extent of resection has not been reported.
Setting:
Toronto, Canada.
Methods:
All MPE cases between 1972 and 2005 at a single institution were identified and reexamined by a neuropathologist. Neurological outcomes (Frankel scale), clinical features, operative findings, pre and postoperative imaging results were reviewed.
Results:
A total of 18 operations were performed on 15 MPE patients (8 females/7 males; age range: 18–71 years). Median postoperative follow-up was 56 months. Three patients (17%) developed tumor regrowth requiring reoperations. Preoperative magnetic resonance imaging (MRI; in 14/18 procedures) determined that tumors involved the conus in 70% of cases, which was significantly associated with intraoperative findings (P=0.02). Complete microsurgical resection was accomplished in 4 out of 7 cases where conus was not involved, but in only 1 out of 10 cases with conus involvement (P=0.056). The degree of conus involvement in one case was unclear. None of patients with total surgical resection developed recurrence. All patients survived at long-term follow-up.
Conclusion:
Our series is the first to correlate MPE involvement to conus medullaris on preoperative MRI with intraoperative findings, and examine its significance on surgical resectability. This information could guide clinicians in preoperative planning and advising patients on treatment options and potential risks/benefits. MRI is very sensitive (100%) and moderately specific (67%) in detecting direct anatomical contact between conus and MPE tumors.
Similar content being viewed by others
Introduction
Myxopapillary ependymomas (MPEs) are the most common glial tumor arising in the conus–filum region. Kernohan1, 2 was the first to recognize MPE as a distinct subtype of ependymoma. Currently, MPE is classified as a slow growing, grade I tumor, according to the current WHO classification of central nervous system tumors.3
The goal of surgical resection, which is the primary mode of therapy, is to achieve complete resection while minimizing postoperative neurological deficits. The extent of the surgical resection is variable, given the complex anatomical relationship of these tumors to the surrounding nerve roots and conus medullaris. The strategic location of MPE in the conus–cauda area, the tendency for these lesions to present late with extensive local disease and dense attachment to eloquent neural structures, has been shown to limit the completeness of surgical resection.4, 5 These anatomical limitations may also be associated with an increased risk of local recurrence, although previous reports have largely relied on plain or computed tomography–myelography (Table 1).6
Magnetic resonance imaging (MRI) has evolved as the test of choice for both diagnosis of MPE and determination of the extent of tumor involvement to the neural elements.7, 8 MRI features of MPE have been described previously;7 however, MRI sensitivity in predicting conus/cauda involvement has not been determined.
In the present paper, we sought to determine the preoperative key imaging features, which would influence surgical resectability. The secondary goal of this study was to determine the long-term survival and neurological disability associated with surgical resection of MPE. Our series is the first to correlate MPE involvement of the conus medullaris on preoperative MRI with intraoperative findings and examine its significance on surgical resectability. This information could guide clinicians in preoperative planning and advising patients on treatment options and potential risks/benefits.
Materials and methods
Patient selection and follow-up
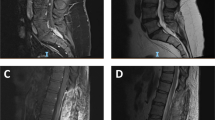
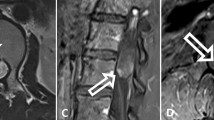
Approval from the Research Ethics Board at the University Health Network was obtained. We screened Toronto Western Hospital surgical pathology reports from 1972 to 2005, and identified 68 cases diagnosed with spinal ependymoma. The original pathology slides were reexamined by a single neuropathologist (PS). Only 15 cases (22%) with confirmed histopathological characteristics of MPE, according to the 2000 WHO nervous system tumor classification, were included in the study. Both inpatient and outpatient medical records were retrospectively reviewed. Postoperative follow-up was classified as early (before hospital discharge) or late (latest hospital follow-up and a telephone questionnaire). Frankel's classification (A=complete motor and sensory loss, B=preserved sensation only, C=motor and sensory incomplete function, D=useful motor function, E=no motor or sensory function disorder) was used to evaluate neurological function preoperatively and at each stage of follow-up.9 Sphincter involvement was defined as any disturbance of bladder or bowel function ranging from hesitancy or frequency (not explained on the basis of infection or urological disorder) to incontinence. As MRI was used as the principal imaging modality in 14 out of 18 operations performed, the earlier 4 surgeries were preceded by myelography (2 with post-myelographic computed tomography). MRI studies have routinely included T1 and T2-weighted images and contrast-enhanced T1 axial and sagittal images. Findings on the MRI were determined based on the radiology report, independent of knowledge of the pathology or intraoperative surgical findings. Both preoperative imaging studies and intraoperative findings were used to determine whether the tumor involved (that is, was in anatomical continuity with) the conus and/or cauda (for example, Figure 1), as well as the number of levels affected. The median duration of direct clinical follow-up was 30 months. With telephone follow-up, this increased to 56 months (range: 31–79.6 months). All patients had a long-term follow-up MRI with the exception of one patient.
Surgical treatment
Micro-neurosurgical techniques were used for tumor resection in all cases. The extent of surgical resection was based on careful review of the operative reports. The resection was described as gross total (GTR) if the surgeon did not see or leave any residual tumor at the end of the resection, and if this was confirmed by postoperative MRI. Intraoperative neurophysiological monitoring techniques were used in 13 out of 15 procedures as described in previous reports from our unit;10 information was missing on the remaining three surgeries. Modalities utilized included nerve root stimulation, electromyography, urinary and anal sphincter activity monitoring, and somatosensory evoked potentials. Adjuvant postoperative radiotherapy was used in four cases for recurrent or residual disease.
Tumor progression/recurrence
Progression was defined as tumor regrowth on follow-up imaging studies following an incomplete resection, which were either done as part of routine postoperative assessment or initiated by a change in the patient's clinical status. Tumor regrowth following complete resection was considered as a recurrence.
Statistical analysis
Continuous variables were described as median, 25th and 75th percentiles. Categorical variables were described as frequencies. Fisher's exact test was used to determine significant associations. P-values <0.05 were considered statistically significant. Survival free of progression/recurrence was analyzed with Kaplan–Meier method. Log–rank test was used to determine significant differences between cohorts. All analyses were conducted with R statistical package (www.R-project.org).
Results
Patient population
There were 15 patients identified (8 females, 7 males) with a median age of 43.5 years (range: 18–71). Table 2 summarizes the clinical features of the patient population.
Clinical outcome
Pre and postoperative Frankel grades, for the available data, are summarized in Figure 2. Clinical follow-up showed a pattern of improvement over time: for instance, no patients deteriorated to grade A or B, and the proportion of patients with Grade E status increased from 25% preoperatively to 50% at late follow-up. Only one patient, whose recurrent tumor was resected from the conus, significantly deteriorated (from Frankel grade D to C) during early postoperative period. Sphincter disturbances in the early postoperative period were worse in 29%, same in 7%, better in 21% and normal in 43% of cases. At late follow-up (median 56 months), 56% of patients reported normal sphincter function. Back pain was more difficult to accurately assess given the lack of standardized scale; however, only 18% of patients reported an improvement in their back pain before hospital discharge, and 75% of patients had some degree of back pain at late follow-up. Postoperative cerebrospinal leaks were observed in two patients and were managed successfully with lumbar subarachnoid drains.
Imaging characteristics
The involvement of the conus medullaris with tumor on preoperative MRI, which was found in 70% of our patients, was significantly associated with intraoperative determination of conus involvement (P=0.02). The sensitivity of a preoperative MRI to detect conus involvement with tumor was 100% with a specificity of 67%. The conus was likely to be involved with tumor, if the MRI was suggestive of that in 77.8% (PPV 0.778). During operative exposure, tumor involved conus in 58%, and adhered to cauda equina nerve roots in 71% of cases.
The upper extent of tumor was found at T12 and L1, 31% each. In only one case, the tumor extended up to T8. The lower level of tumor was at L2 in 50% of patients, and L5 in one case. In 38% of cases, the tumor spanned two segments of the spinal column, whereas 31% of cases had a tumor spanning three segments. Involved levels ranged from 1 to 10 (mean=3, median=2.5). Follow-up MRI duration ranged from 3 to 173 months (mean=47, median=30 months).
Treatment
The 15 patients in this study had 18 operations for resection of MPE. Three patients had a second procedure (17.6%) for recurrent disease. Only one patient was reported to have a significant intraoperative monitoring change. It improved following modification of the surgical technique.
Regarding the 18 surgical procedures done for MPE, GTR was accomplished in only 1 out of 10 procedures where the tumor has involved the conus compared with 4 out of 7 procedures where the conus was not involved. The remaining procedure had a subtotal resection, but we could not determine from the records whether the tumor was attached to the conus or not. This tumor had recurred 5 years later where it was not attached to the conus and was totally resected. The difference in the degree of resection between the two groups, whether or not the tumor was attached to the conus, approached significance (P=0.056). There was a trend between the number of levels involved and the degree of resection (odds ratio=5.9, 95% CI (0.75, 47.4), P=0.091). The degree of adherence of the tumor to the nerve roots of the cauda equina was not significantly associated with resectability, although this approached significance (P=0.12). Considering all patients in the series, GTR was accomplished in 28% of patients whereas subtotal resection was achieved in 72%. The operating surgeon determined the degree of surgical resection based on intraoperative findings.
The attending surgeon offered radiation treatment to six patients. Although two patients refused to undergo radiation therapy based on personal considerations, four patients had a dose of 5000 cGy of postoperative radiotherapy, in fractions. The first patient had radiotherapy following a subtotal resection. He subsequently developed tumor progression, upon which he was reoperated. The second patient had radiotherapy following total surgical resection based on concerns by the treating surgeon of the potential for recurrence. He was not reported to have recurrence at 4 years of follow-up. Based on our current experience, we would now not recommend radiation in the treatment of MPEs when complete microsurgical resection had been achieved. The other two patients, who had subtotal resections followed by radiotherapy, did not reported tumor progression at 2 and 5 years, respectively.
Tumor progression/recurrence
Initial GTR was achieved in 4 out of 15 patients, 10 had subtotal resection, and 1 could not be determined. None of the patients who had total resection developed tumor recurrence during the follow-up period. All of the three tumor progression cases occurred in the subtotal resection group. The time intervals between initial surgical resection and tumor progression were 2, 3 and 6 years, respectively.
No distant metastasis was detected; all recurrences occurred locally and were reoperated on. Only one patient had a gross total resection at reoperation.
Postoperative radiation was undertaken in only one of the three tumor progressions we encountered, which did not decrease the likelihood of recurrence (P=1). However, this should be interpreted with caution given both the evolving radiation technology and the low number of patients in our study. None of the patients died during the follow-up period (Figure 3).
Discussion
The extent of surgical resection of MPE is mainly related to involvement of the neural elements (namely conus medullaris and cauda equina) and tumor encapsulation.2, 8 In the present study, only 1 out of 10 patients with tumor involving the conus had a total surgical resection, compared with 4 out of 7 patients with no conus involvement, an association that approached significance (P=0.056). The fear of an adverse neurological outcome, especially with regards to sphincter dysfunction, was the most common rationale for leaving some residual tumor on the conus. As summarized in Table 1, these findings were consistent with previous reports.4
The long-term survival for MPE has been excellent, reported at 10 years as 97% for overall survival, and 62 and 72% for both progression-free survival and local control, respectively.5 The degree of surgical resection has been shown to significantly alter the survival in spinal cord ependymoma.4, 5, 11 However, that is controversial for MPE. In the landmark paper by Sonneland et al.,2 less recurrence (10%) was observed with gross total removal of encapsulated tumors when compared with those removed in piecemeal (34% recurrence) or subtotally resected tumors (41% recurrence). Their survival, however, was more related to total resection, either total or piecemeal (19 years), when compared with those resected subtotally (14 years).2 On the other hand, a recent report from MD Anderson5 did not find that the extent of the initial resection significantly affected either the progression-free survival or the overall survival for MPE patients. In the current study, none of the patients who had total resection developed tumor recurrence during a median hospital follow-up period of 30 months. Also, none of the patients died during the follow-up period. On the other hand, MPE of the pediatric age group was reported to be more aggressive with tendency for more dissemination (up to 80%).8, 12
As reviewed in Table 1, our series of surgically treated MPEs is one of the largest to date in which MRI was the principal imaging modality used. Moreover, our series is the first to examine the association of the preoperative MRI with intraoperative predictors of complete microsurgical respectability. Although intraoperative assessment remains the gold standard in predicting conus involvement with tumor, preoperative MRI was found to be fairly reliable (sensitivity 100%, specificity 67% and PPV of ∼80%). MRI finding of tumor adherence to the conus was also significantly associated with the intraoperative findings (P=0.02). Adherence of the tumor to the cauda-equina nerve roots is another important factor that may interfere with total resection; this factor did not achieve significance in this study (P=0.12).
Total surgical resection is presumed to be the goal for every attempted resection because of its association with longer survival, both in adults and pediatrics.2, 8 However, the intent of our operating surgeons for the degree of resection was not clear from the clinical documents.
Consistent with the literature,3 our study found the most common clinical presentation was back pain (94%). Neurological deficit on presentation tended to be minimal (Frankel grade D 75%, E 25%), probably related to the slow growing nature of MPE. Our study determined the duration of symptoms to be 1.8 years. This is more consistent with recent literature4, 5 than older studies,3 probably reflecting the advancement of imaging modalities, especially MRI. Long-term postoperative follow-up indicated a pattern of clinical improvement over time. Our data suggest that patients who had a total resection were less likely to have sphincter dysfunction, however, this may be a reflection of the fact that most of the totally resected tumors did not involve the conus.
MPEs are intradural extramedullary tumors that can be multiple in 14–43% of patients.7, 13, 14 On MRI, they tend to be hypointense to isointense on T1-weighted images, and hyperintense on proton density and T2-weighted images.7 They can also show hyperintense signal on T1-weighted images and may include areas of cystic changes and hemorrhage.3 Contrast enhancement is essential in differentiating these lesions from the normal surrounding spinal cord and in defining their cystic components.7 MRI features are helpful but not specific8 and correlation with the location and clinical characteristics is required for the diagnosis.
The benefit of postoperative radiotherapy for MPE remains controversial given variable results in the literature.5, 8 Our data did not support a significant reduction in tumor recurrence/progression following postoperative radiation.
Our results must be interpreted within the context of the retrospective nature of the study design. However, the rarity of MPE is mostly suited with such a design. Also, the advancing MRI resolution and intraoperative microscope technology have to be taken into consideration.
Conclusion
MPE has a generally benign clinical course. MRI reliably assesses tumor involvement to the conus medullaris, which can be helpful for directing surgical resection, planning postoperative therapy, and counseling patients and their families. Although the goal of surgery should be to achieve complete resection, this should not be accomplished at the cost of a major neurological deficit. Accordingly, in the setting of significant conus involvement subtotal resection appears to be a reasonable option and associated with good outcomes at a median follow-up in our series of just <5 years.
References
Kernohan J . Primary tumors of the spinal cord and intradural filum terminale. In: Penfield W (ed). Cytology and cellular pathology of the nervous system. Paul B. Hoeber: New York, 1932, pp 993–1025.
Sonneland PR, Scheithauer BW, Onofrio BM . Myxopapillary ependymoma. A clinicopathologic and immunocytochemical study of 77 cases. Cancer 1985; 56: 883–893.
Wiestler OD, Schiffer D, Coons SW, Rosenblum MK, Prayson RA . Ependymal tumours. In: Kleihues P, Cavenee WK (eds). Pathology and genetics of tumours of the nervous system. IARC Press: Lyon, France, 2000, pp 78–79.
Chang UK, Choe WJ, Chung SK, Chung CK, Kim HJ . Surgical outcome and prognostic factors of spinal intramedullary ependymomas in adults. J Neurooncol 2002; 57: 133–139.
Akyurek S, Chang EL, Yu TK, Little D, Allen PK, McCutcheon I et al. Spinal myxopapillary ependymoma outcomes in patients treated with surgery and radiotherapy at M.D. Anderson Cancer Center. J Neurooncol 2006; 80: 177–183.
Celli P, Cervoni L, Cantore G . Ependymoma of the filum terminale: treatment and prognostic factors in a series of 28 cases. Acta Neurochir (Wien) 1993; 124: 99–103.
Wippold II FJ, Smirniotopoulos JG, Moran CJ, Suojanen JN, Vollmer DG . MR imaging of myxopapillary ependymoma: findings and value to determine extent of tumor and its relation to intraspinal structures. AJR Am J Roentgenol 1995; 165: 1263–1267.
Bagley CA, Kothbauer KF, Wilson S, Bookland MJ, Epstein FJ, Jallo GI . Resection of myxopapillary ependymomas in children. J Neurosurg 2007; 106 (4 Suppl): 261–267.
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia 1969; 7: 179–192.
Krassioukov AV, Sarjeant R, Arkia H, Fehlings MG . Multimodality intraoperative monitoring during complex lumbosacral procedures: indications, techniques, and long-term follow-up review of 61 consecutive cases. J Neurosurg 2004; 1: 243–253.
Waldron JN, Laperriere NJ, Jaakkimainen L, Simpson WJ, Payne D, Milosevic M et al. Spinal cord ependymomas: a retrospective analysis of 59 cases. Int J Radiat Oncol Biol Phys 1993; 27: 223–229.
Fassett DR, Pingree J, Kestle JR . The high incidence of tumor dissemination in myxopapillary ependymoma in pediatric patients. Report of five cases and review of the literature. J Neurosurg 2005; 102 (1 Suppl): 59–64.
Chan HS, Becker LE, Hoffman HJ, Humphreys RP, Hendrick EB, Fitz CR et al. Myxopapillary ependymoma of the filum terminale and cauda equina in childhood: report of seven cases and review of the literature. Neurosurgery 1984; 14: 204–210.
Ross DA, McKeever PE, Sandler HM, Muraszko KM . Myxopapillary ependymoma. Results of nucleolar organizing region staining. Cancer 1993; 71: 3114–3118.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Al-Habib, A., Al-Radi, O., Shannon, P. et al. Myxopapillary ependymoma: correlation of clinical and imaging features with surgical resectability in a series with long-term follow-up. Spinal Cord 49, 1073–1078 (2011). https://doi.org/10.1038/sc.2011.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.67
Keywords
This article is cited by
-
Intramedullary spinal cord and filum tumours—long-term outcome: single institution case series
Acta Neurochirurgica (2022)
-
Spinal myxopapillary ependymomas: a retrospective clinical and immunohistochemical study
Acta Neurochirurgica (2016)
-
Pediatric spinal ependymomas: an unpredictable and puzzling disease. Long-term follow-up of a single consecutive institutional series of ten patients
Child's Nervous System (2014)