Abstract
Study design:
Retrospective chart review.
Objective:
To evaluate the clinical outcomes and factors influencing patient satisfaction with Malone antegrade continence enema (MACE) in patients with spina bifida.
Setting:
Japan.
Methods:
We performed retrospective analysis of 21 patients with spina bifida who underwent surgical creation of an MACE stoma. Clinical outcomes were evaluated by medical records, operative notes and mailed questionnaires. Patient satisfaction scores (SSs) were measured on a modified visual analog scale (VAS) from 1 to 10, and the factors influencing the SS were analyzed.
Results:
A 100% return rate for the mailed questionnaires was achieved. All patients underwent in situ appendicocecostomy with cecal plication. There was only one complication that required surgical revision. Regarding fecal continence, the overall success rate was 90%. Although 4 patients (19%) had severe irrigation pain and 4 patients (19%) found the washout time intolerably long, 18 (85%) of them were satisfied with the MACE procedure. Age at operation, experience of retrograde colonic enema (RCE), experience of stomal leakage, increased comfort at school or workplace and increased comfort at sleepovers significantly influenced SSs.
Conclusion:
MACE is a valuable option in achieving fecal continence in patients with spina bifida, with most patients being satisfied with the procedure. In our analysis, younger age at operation, previous experience of RCE, no stomal leakage and improvement of quality of life (enhanced comfort at school, workplace and sleepovers) significantly influenced the high satisfaction after MACE.
Similar content being viewed by others
Introduction
The Malone antegrade continence enema (MACE) procedure, which was first described in 1990 by Malone et al.,1 has revolutionized the management and improved the quality of life (QOL) of patients with spina bifida who suffer from refractory constipation and fecal incontinence. However, it has been reported in a long-term follow-up study that a considerable number of patients have ceased the MACE procedure.2 To select good candidates for the MACE procedure among patients with spina bifida, it is important to evaluate not only the status of the bowel, but also the overall patient satisfaction after the procedure. The aim of this study was to evaluate the factors that influence overall satisfaction after the MACE procedure in patients with spina bifida.
Materials and methods
An institutional review board-approved retrospective chart review was performed of patients with spina bifida who underwent the MACE procedure between June 2004 and February 2012, performed by a single surgeon at our institution. We collected demographic information on the patients and their families, surgical techniques and complications, from medical records and operative notes. The onymous questionnaire was mailed to all patients to evaluate the MACE procedure, its complications, clinical outcomes, comparison with prior retrograde colonic enema (RCE), influence on the QOL, impact on social confidence, satisfaction score (SS) and patients’ recommendations to other patients. In addition, we asked the patients’ caregivers to assess the changes in their daily life after the MACE procedure. In case of no response, the patient or caregiver was kindly reminded by telephone.
The patients’ SS was evaluated on a modified visual analog scale (VAS) from 1 to 10 (Figure 1). In this scale, a higher score represents a higher level of satisfaction. To evaluate the factors influencing patient satisfaction, we analyzed the relationship between SS and 17 factors selected from the onymous questionnaire and demographic data. Data were analyzed using a two-tailed unpaired t test or Wilcoxon rank-sum test, as appropriate. For all statistical analyses, P<0.05 was considered as statistically significant. All statistical analysis was performed using JMP 9 (SAS Institute Inc., Cary, NC, USA).
Results
During the study period, 22 patients with spina bifida underwent the MACE procedure at our institution. All patients suffered from intractable constipation and/or fecal incontinence before surgery. All the patients returned completed questionnaires (response rate, 100%). One female patient who refused to use MACE from the outset was excluded from the study. Hence, a total of 21 patients were included in this study. Their demographic data are shown in Table 1. There were 10 males (47%) and 11 females (52%), with a mean age of 19.5 years (range, 7.9–29.5 years). The median follow-up time was 75 months (range, 23–104 months). Clean intermittent catheterization of the bladder was performed in all patients and social urinary continence was achieved in 20 (95%) of them.
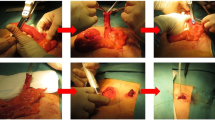
In terms of the surgical procedure, all patients underwent in situ appendicocecostomy with cecal plication around the appendiceal base. Of the patients, 20 underwent umbilical anastomosis using the V-V appendicoplasty technique. Only one patient underwent skin anastomosis using VR skinplasty at the right lower quadrant of the abdomen due to the simultaneous performance of umbilical Mitrofanoff procedures.3 The Malone stoma was created by laparotomy in all patients, and 17 patients underwent simultaneous urinary tract reconstruction, including bladder augmentation, bladder neck reconstruction, ureterocystostomy and Mitrofanoff procedures.
Assessment of surgical complications indicated that there were only two complications related to the MACE stoma. One patient with stomal mucosal prolapse underwent operative revision, while another one with minor stomal infection was treated with antibiotics. The remaining 19 patients had no postoperative complications requiring medical treatment. Of the 21 patients, 13 (62%) were completely independent following the MACE procedure. In only two patients, aged 14 and 16 years, the entire enema was performed by caregivers. The mean irrigation volume using tap water was 1150 ml (range, 700–2000 ml). The mean washout time was 60.4 min (range, 30–120 min). Four (19%) of the patients found the washout time intolerably long. Further, four of the patients (19%) felt intolerable irrigation pain.
The criteria for determination of fecal continence were based on the Malone criteria.4 Full success (totally clean, experiencing only minor leakage of the washout at night), partial success (clean but with occasional major leakage) and failure (regular fecal incontinence episodes) were recognized in 11 (52.4%), 8 (38.1%) and 2 (9.5%) of the patients, respectively. However, all patients except one expressed definite improvement of fecal continence after MACE. Of the 21 patients, 1 male patient stopped use of the MACE 6 years after the operation due to prolonged washout time. However, after use of the MACE for such a long time, he became able to defecate by himself regularly.
Patient satisfaction
Of the 21 patients, 18 (85%) indicated SS of 6 or more. The mean SS was 7.8 (range, 5–10). Table 2 shows the relationship between SS and 17 factors, including demographics and several QOL data. Demographic data had no relationship with patient satisfaction, except for age at the time of the operation and experience of RCE. Figure 2 shows the SS of the patients in terms of age at the time of the operation. Comparison of the group that had surgery at a younger age (⩽10 years) with those that had surgery at an older age (>10 years) indicated significantly higher SS in the younger age group. The SS of patients with RCE experience was significantly higher than patients without RCE experience (P=0.02). Duration of MACE usage had no effect on SS, there being no significant difference in SS between short usage (⩽5 years) and long usage (>5 years) groups. Regarding the MACE procedure and clinical outcomes, independence in performing the procedure, status of fecal continence, severity of irrigation pain and tolerability of washout time did not significantly influence SS. However, patients with occasional stomal leakage reported significantly lower SS than patients without it (P=0.02). In the questions about QOL, there were no significant differences in SS between patients who wore and those who did not wear diapers during the daytime. Patients who felt enhanced comfort at school or the workplace and enhanced comfort at sleepovers after MACE indicated significantly higher SS. Of the 21 patients, 81% said they would recommend this procedure to other patients with spina bifida.
Answers from caregivers
Eighteen caregivers answered the questionnaire about the change in their daily life after MACE. Twelve of the eighteen (66%) caregivers reported that MACE relieved the burden of their daily life. All four caregivers of the patients who indicated the highest SS answered that MACE relieved their burden.
Discussion
The MACE procedure, which was first described in 1990 by Malone et al.,1 has revolutionized the management and improved the QOL of children with neuropathic bowel, refractory constipation and fecal incontinence.5, 6 In a systematic review of 24 studies, overall fecal continence was achieved in 93% of the patients.7 However, it is difficult to compare success rates in patients at different centers and with different underlying diseases. Acceptance of the MACE procedure by patients with spina bifida at a special reference center may be different from that by children with anorectal malformations at a clinic of pediatric surgery. In addition, despite the high success rates of the MACE procedure, Yardley et al.2 reported in a long-term follow-up study that a considerable number of patients had ceased MACE procedures. On the other hand, they described that satisfaction rates were very high in patients who continued to use MACE over a long period of time. From this point on, to evaluate the MACE procedure, it is essential to investigate the success rate not only in terms of fecal continence, but also the degree of patient satisfaction after the procedure. If there are, indeed, several predictive factors influencing patient satisfaction after the MACE procedure, then knowledge of these factors will be useful to both physicians and patients when considering the indications of MACE.
Although this series was small, it included only spina bifida patients with intermittent catheterization. Furthermore, a 100% return rate for the mailed questionnaires and low dropout rate of MACE made this study quite adequate for evaluating SS following MACE. The reason for the low dropout rate (1 out of 21) is unknown. However, one possible explanation for this could be the continuing support of our nursing specialists at every patient visit.
The overall success rate in this study, which included partial success with occasional fecal leakage, was 90%, although only 52% achieved complete success. The mean age of patients at the time of evaluation in this study was higher than in previous studies (19.5 versus 10.7 years).7 Vande Velde et al. described that the continent group of patients with spina bifida tended to be younger. In their study of MACE in patients with spina bifida, fecal continence was achieved in 6 of 7 children (86%) and 7 of 11 adults (64%).8 In terms of surgical complications, our study showed very few complications. There were no serious complications, such as shunt infection, ileus and severe stomal stenosis requiring operative revision. Infection of the catheterizable stoma that developed in one patient was cured with medical management. Only one patient underwent stomal revision due to mucosal prolapse. Although occasional minimal stomal leakage and painful catheterization were recognized in a few patients, no patient needed additional surgery to fix these problems. The possible reason for this low complication rate was that we performed in situ appendicostomy with a cecal plication. With almost the same techniques, Herndon et al. reported that stomal revisions were required in 11 (8.7%) patients, which was lower than other previous reports.7, 9 They suggested that the reason for their low stomal revision rate was preservation of cecal blood supply at the base of the appendix, thereby limiting its dependence on an isolated appendiceal mesentery.
In terms of overall patient satisfaction, our study showed a satisfaction rate (SS⩾6) of 85% with a mean SS of 7.8 (range, 5–10). Hoekstra et al.6 reported relatively similar results of SS on almost the same scale from 1 to 10 in children with intractable defecation disorders. In their study, 86% of the patients were satisfied, with a median score of 8 (range, 6–10). In this study, we analyzed the factors influencing patient satisfaction. To our knowledge, there has been no study that determined which patient variables have an impact on patient satisfaction after the MACE procedure, particularly in patients with spina bifida. Yerkes et al.5 used satisfaction and QOL questions based on a 5-point Likert scale in 65 patients (including 57 with myelodysplasia), and found that responses for overall satisfaction were very satisfied, satisfied and very dissatisfied in 89, 9 and 1.5%, respectively.5 They opined that it was not possible to stratify patients to determine the factors influencing patient satisfaction due to the large percentage of positive responses. To make a detailed analysis of patient satisfaction, we used a modified VAS from 1 to 10 to assess SS, instead of the 5-point Likert scale. Although measurement of patient satisfaction with VAS has not received wide acceptance particularly in children <10 years of age, it has previously been used in other subjects and has been shown to be valid in previous reports.10, 11 The overall satisfaction rate in this study was 85.7%, however, only four patients (19%) scored 10.
Many questions about the MACE procedure and QOL after the procedure were asked in this cohort, in an attempt to define the variables predicting patient satisfaction. In our analysis, there were five factors, including age at operation, experience of RCE, experience of minimal stomal leakage, enhanced comfort at school or workplace and enhanced comfort at sleepovers, that significantly influenced SS. When divided into younger (10 years and younger) and older age (11 years and older) groups, patients with MACE introduction at a younger age showed significantly higher SS, as demonstrated by the fact that four of the six patients in the younger age group scored 10 on the VAS in this study. Although the questionnaires were mailed to the patient and the present age of most patients was above 10 years, we assume that a parent completed the questionnaire in many of the younger age group patients. Therefore, their responses may reflect the opinions of the parent rather than the patient. In fact, the caregivers of all the four younger age patients who scored 10 on SS answered that MACE relieved their burden. On the other hand, older age group patients, particularly adolescents, tended not to be highly satisfied with the procedure.
In our cohort, previous experience of RCE was significantly related to the SS. This finding definitely supports stepwise and individually tailored bowel management programs by a multidisciplinary team starting in childhood.12 It can be easily imagined that patients and their caregivers would appreciate the ease of MACE procedures and its high success rate compared with their previous bowel management strategy, particularly RCE. Patients who have not previously experienced problematic bowel management strategies seem to be not highly satisfied with MACE, regardless of their bowel condition. In our study, the perfection of continence was not significantly related to SS. However, the occasional experience of even minimal stomal leakage significantly decreased SS. This indicates that patients strongly fear even a small stain on their shirts.
In our previous study, procedure independence was significantly better in the MACE group compared with the RCE group in children with spina bifida.13 However, the level of independence was not significantly related to SS. Furthermore, SS had no relation to whether or not the patients wore diapers during the daytime. These findings may reflect the overall limit of independence, complete urinary continence and fecal continence in these patients. Finally, significantly higher SS was recognized in patients who felt enhanced comfort at school, their workplace and at sleepovers after MACE. Thus, we should not only be concerned about the patients’ bowel condition, but also strongly encourage and support patients in their daily life after MACE.
The main limitations of this study include its retrospective design, using a non-validated questionnaire, small size of the cohort, and the use of VAS which is not a validated tool for patient satisfaction in children <10 years of age. Besides these, our study results are also limited by the fact that the majority of our patients underwent simultaneous urinary tract reconstruction. Although there was no significant difference in SS on the basis of status of simultaneous urinary tract reconstruction, and it was stressed that the focus of the questionnaire was the MACE procedure, patients’ SS may have been influenced by their urinary tract condition after surgery. In addition, assessment of bowel condition was based on the self or caregiver reported outcomes, without physiologic evaluation.
Conclusions
In our analysis, younger age at operation, previous experience of RCE, no stomal leakage and improved QOL (greater comfort at school, workplace and sleepovers) significantly contributed to the high satisfaction after the MACE procedure in patients with spina bifida.
Data Archiving
There were no data to deposit.
References
Malone PS, Ransley PG, Kiely EM . Preliminary report: the antegrade continence enema. Lancet 1990; 336: 1217–1218.
Yardley IE, Pauniaho SL, Baillie CT, Turnock RR, Coldicutt P, Lamont GL et al. After the honeymoon comes divorce: long-term use of the antegrade continence enema procedure. J Pediatr Surg 2009; 44: 1274–1276.
Franc-Guimond J, González R . Simplified technique to create a concealed catheterizable stoma: the VR flap. J Urol 2006; 175: 1088–1091.
Curry JI, Osborne A, Malone PS . How to achieve a successful Malone antegrade continence enema. J Pediatr Surg 1998; 33: 138–141.
Yerkes EB, Cain MP, King S, Brei T, Kaefer M, Casale AJ et al. The Malone antegrade continence enema procedure: quality of life and family perspective. J Urol 2003; 169: 320–323.
Hoekstra LT, Kuijper CF, Bakx R, Heij HA, Aronson DC, Benninga MA . The Malone antegrade continence enema procedure: the Amsterdam experience. J Pediatr Surg 2011; 46: 1603–1608.
Sinha CK, Grewal A, Ward HC . Antegrade continence enema (ACE): current practice. Pediatr Surg Int 2008; 24: 685–688.
Vande Velde S, Van Biervliet S, Van Laecke E, De Bruyne R, Verhelst H, Hoebeke P et al. Colon enemas for fecal incontinence in patients with spina bifida. J Urol 2013; 189: 300–304.
Herndon CD, Rink RC, Cain MP, Lerner M, Kaefer M, Yerkes E et al. In situ Malone antegrade continence enema in 127 patients: a 6-year experience. J Urol 2004; 172: 1689–1691.
Singer AJ, Thode HC Jr . Determination of the minimal clinically significant difference on a patient visual analog satisfaction scale. Acad Emerg Med 1998; 5: 1007–1011.
Brokelman RB, Haverkamp D, van Loon C, Hol A, van Kampen A, Veth R . The validation of the visual analogue scale for patient satisfaction after total hip arthroplasty. Eur Orthop Traumatol 2012; 3: 101–105.
Choi EK, Shin SH, Im YJ, Kim MJ, Han SW . The effects of transanal irrigation as a stepwise bowel management program on the quality of life of children with spina bifida and their caregivers. Spinal Cord 2013; 51: 384–388.
Matsuno D, Yamazaki Y, Shiroyanagi Y, Ueda N, Suzuki M, Nishi M et al. The role of the retrograde colonic enema in children with spina bifida: is it inferior to the antegrade continence enema? Pediatr Surg Int 2010; 26: 529–533.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Imai, K., Shiroyanagi, Y., Kim, W. et al. Satisfaction after the Malone antegrade continence enema procedure in patients with spina bifida. Spinal Cord 52, 54–57 (2014). https://doi.org/10.1038/sc.2013.111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.111
Keywords
This article is cited by
-
Impact of Neurogenic Lower Urinary Tract Dysfunction on Bowel Symptoms
Current Bladder Dysfunction Reports (2023)
-
Der querschnittgelähmte Patient – Besonderheiten der viszeralchirurgischen Diagnostik und Therapie
Der Chirurg (2021)
-
Leitlinie: Neurogene Darmfunktionsstörung bei Querschnittlähmung (Langfassung)
coloproctology (2020)
-
Long-term outcomes of a Malone antegrade continence enema (MACE) for the treatment of fecal incontinence or constipation in adults
International Journal of Colorectal Disease (2018)
-
Neurogenic Bowel Dysfunction in Patients with Neurogenic Bladder
Current Bladder Dysfunction Reports (2016)