Abstract
Study design:
Retrospective cohort study, using linked, population-based health-care data.
Objectives:
To describe the incidence, management and outcomes of surgically treated kidney stones after spinal cord injury (SCI). To evaluate the impact of a past history of kidney stones on the occurrence of kidney stones.
Setting:
Ontario, Canada.
Methods:
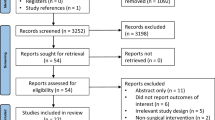
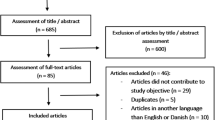
A total of 5121 patients were followed a median of 4 years after an incident SCI (occurring between 2002 and 2011). The primary outcome was surgical intervention for upper tract kidney stones.
Results:
In follow-up, 66 patients (1.3%) had 89 episodes of surgically treated kidney stones. Treatments included: ureteroscopic lithotripsy (34%), ureteral stent/percutaneous nephrostomy (30%), shockwave lithotripsy (19%) or percutaneous nephrolithotripsy (17%). Following stone treatment, the 30-day mortality rate was low, and the 30-day admission rate to an intensive care unit was 12%. A history of surgically treated kidney stones before SCI (compared with no such history) was associated with a higher risk of kidney stones after SCI (27 vs 3 per 1000 person-years; adjusted hazard ratio 14.74, 95% confidence interval 5.69–38.22).
Conclusion:
During intermediate follow-up after SCI, surgically treated upper tract kidney stones occur in 1.3% of patients. Ureteroscopy with lithotripsy is the most common treatment. A history of surgically managed kidney stones before SCI portends a higher risk of stones after SCI.
Similar content being viewed by others
Introduction
Patients with spinal cord injuries (SCIs) are at increased risk for kidney stones (including calculi within the kidney or ureter). Previous studies have estimated that up to 40% of SCI patients may develop kidney stones.1 The incidence of kidney stones after SCI in one American cohort was 8 per 1000 person-years,2 which is at least six times greater than the general population.3
Upper tract stone disease among SCI patients has significant complications because of an atypical clinical presentation, obstructive urosepsis and treatment-related complications.4 Percutaneous nephrolithotomy (PNL) maybe more common among SCI patients, and has been reported to be associated with significant perioperative morbidity and mortality.5, 6, 7 The use of ureteroscopy was traditionally limited by the inability to position many SCI patients in the lithotomy position; however, the contemporary use of flexible ureteroscopy in this population has not been formally studied.
Risk factors for stone disease among SCI patients include specific metabolic changes, and urinary infection; the impact of other injury-specific variables, such as lesion level and functional status, is not clearly defined.8
The objectives of study were: (1) to measure the incidence of surgical intervention for kidney stones among SCI patients; (2) to describe the treatment modalities used in this population; (3) to examine the relationships between kidney stones before SCI, and the level of the SCI and the subsequent risk of surgical intervention for kidney stones; (4) to describe the mortality, morbidity and prior renal imaging patterns of patients with surgically treated kidney stones.
Materials and methods
Study design
We conducted a retrospective cohort study based on population level, administrative data from Ontario, Canada. Ontario has a population of >13 million, and a universally accessible, publicly funded health-care system, which does not allow billing outside of the Ontario Health Insurance Plan (OHIP). As such, this data can be considered population based. We obtained institutional ethics approval for this study.
Data sources and validity
All rehabilitation centers in Ontario have been required to submit standardized reports to the National Rehabilitation System (NRS) since 2002. All hospitals in Canada are required to submit hospitalization details to the Canadian Institutes for Health Information Discharge Abstract Database (CIHI-DAD). The data quality of these data sources is maintained through variable verification, and audit-feedback; reabstraction studies have shown >80% agreement with coding elements.9 OHIP surgical fee claims are expected to have a high sensitivity and positive predictive value, as shown with other service payments.10 The databases were essentially complete for all study variables.
Population, exposures and outcomes
Study subjects were identified using the NRS. We included adult patients (>18 years) admitted to a rehabilitation facility in the province of Ontario (Canada) following an incident SCI (traumatic or non-traumatic) between 1 April 2002 and 31 March 2011. We examined the following potential risk factors: lesion level (a binary variable specified in the NRS as either high (C1–C8), or low (⩽T1) SCI), previous history of a surgical procedures for kidney stones (a binary variable representing any surgical intervention for stone disease in the 5 years before SCI based on OHIP codes) and the ability of a patient to manage their own bladder care (functional independence measure score for bladder self-care, from the NRS).11 The functional independence measure-bladder care score was used as a binary variable: independent (regular toileting, or complete self-care with a catheter, and no incontinence) or dependent (some level of assistance from a care aid required, incontinence possible). The functional independence measure does not provide detailed information about the actual method of bladder management (for example, whether a catheter is used), only the degree with which a SCI patient can manage these activities themselves.
Outcome measures were identified by linking our cohort to OHIP, (1 April 2002–20 September 2011) and CIHI-DAD (1 April 2002–30 March 2011) records. The primary outcome was surgically treated upper tract stone disease. This was a composite of OHIP procedure fee codes for the placement of a ureteral stent or percutaneous nephrostomy tube without lithotripsy or stone extraction, shockwave lithotripsy (SWL), ureteroscopic lithotripsy and PNL. Events within 90 days of each other were considered retreatment of the same stone, and were not counted as unique events. If multiple modalities were used within 90 days, then the most invasive treatment modality was considered the primary intervention (nephrostomy tube/ureteral stent<SWL<ureteroscopy<PNL). We also examined the 30-day all-cause mortality rate, the 30-day all-cause admission rate to an intensive care unit (ICU) after stone treatment, bladder stone treatment and the frequency of outpatient renal imaging (all based on OHIP fee codes).
Statistical analysis
We have reported medians (interquartile range, IQR) and percentages (proportion) for continuous and categorical variables. Privacy regulations do not allow reporting of any groups of <6 patients; these are indicated by n<6*. Patients were censored at the end of the follow-up period (30 September 2011), or death. Patients were considered at risk for an event from the time of admission to rehabilitation to the time of censoring.
We used multivariable Cox proportional hazard regression analysis to evaluate the primary outcome of first surgical treatment of renal stone disease between patients with high versus low SCI, whereas controlling for relevant covariates (age, gender, Charlson comorbidity index,12 and previous stone disease. Hazard ratios (HRs), odds ratios (ORs), 95% confidence intervals (CIs) and P-values are reported. SAS 9.2 (SAS Institute, Cary, NC, USA) was used for statistical analysis.
Results
The cohort contained 5121 patients with an incident SCI between April 2002 and March 2011 (Table 1). The majority (62%) were admitted to a rehabilitation unit within 4 weeks of their initial SCI. Each calendar year within the study period contributed a median of 562 (505–612) patients. SCI patients had a median observation time of 3.8 (IQR 1.7–6.2) years after their rehabilitation admission.
A total of 66 patients (1.3%) underwent 89 separate surgical procedures related to stone disease (Table 2). There was a similar proportion of patients with stone disease among traumatic (1.1%) and non-traumatic (1.3%) SCI patients. The incidence rate was 3.4 upper tract stone procedures per 1000 person-years. The cumulative incidence rate for surgical treatment of renal stone disease peaked in the second year after SCI (Figure 1). The most commonly used modality was ureteroscopy with lithotripsy (34%, 30/89 procedures). Multiple PNL procedures (median 2, IQR 2–3) were necessary for most patients who underwent an initial PNL. Of the 66 patients, 6 (9%) had a prior history of stone disease procedures a median of 2 years (IQR 1–4) before their SCI.
A multivariable Cox proportional hazard model demonstrated that a previous history of stone disease requiring surgical treatment in the 5 years before SCI onset was highly associated with a stone-related intervention after SCI (HR of 15, 95% CI 7–38, Table 3). There was no significant association between the level of the SCI and need for surgical treatment of upper tract stone disease (3.4 vs 3.9 per 1000 person-years, HR 0.90, 95% CI 0.49–1.61). Secondary analysis demonstrated that SCI patients with independent bladder function (based on their discharge functional independence measure score) had a significantly reduced hazard of surgically treated stone disease (adjusted HR 0.39, 95% CI 0.23–0.66, P<0.01) compared with those with incontinence or dependent on their caregivers for some aspect of voiding.
The 30-day mortality rates after any stone-related procedure was low (n<6*). Fifty-three percent of stone procedures required subsequent hospital admission for a median of 5 (IQR 3–8) days. Subsequent ICU admission was required in 12% (11/89) of cases; none occurred after SWL. Acute kidney injury with the need for dialysis was a rare event (n<6*) after stone treatment. Renal imaging in the form of either renal ultrasound or computed tomography scan was carried out in patients a median of 36 (IQR 2–112) days before their stone surgery. Before this preoperative imaging, renal imaging was carried out at least once over 5 years in 94% of patients, twice over 5 years in 76% of patients and three times over 5 years times in 58% of SCI patients; only 24% of patients had yearly imaging tests over the 5-year period before their first stone episode. In all, 94 individuals required treatment for bladder stones during the study period (1.8% of the cohort). In univariable analysis, bladder stones were significantly associated with renal stone disease (OR 15.1, 95% CI 7.9–28.7), and tended to occur before the renal stone disease.
Discussion
The need for surgical intervention for upper tract stone disease was an uncommon occurrence in this cohort of SCI patients. Our incidence rate (3.4 upper tract stone procedures per 1000 person-years) and frequency (1.3%) are in keeping with other studies.2, 13 Our results underestimate the overall incidence of upper tract stone disease, as we did not measure stone disease managed without operative intervention (for example, with medical expulsive therapy). This is a safe, and effective option often used for kidney stones in the general population.14 Chen et al.’s15 prior case series demonstrated that approximately 2/3 of stones in the SCI population may be managed without surgical intervention. In the general population, it is estimated that about 17% of asymptomatic stones will require surgical intervention.16
There was an appreciable increase in the incidence rate of upper tract stone interventions in the second year after SCI; previous studies have suggested an even earlier increase within the first 6–12 months.1, 2 This difference may be because stones in this cohort were not diagnosed until later in follow-up, or because this study’s primary outcome was surgically treated stone disease, which would occur later than incidental stone disease.
The majority of SCI patients did not require a PNL. This suggests few were staghorn calculi. This finding is contrary to two previous series that suggested that the majority of stones requiring intervention among SCI patients require a PNL.15, 17 As staghorn calculi may grow slowly over time, the lower proportion of PNLs may represent the intermediate term follow-up of this cohort. Alternatively, SCI patients may be more likely to be managed with ureteroscopy and SWL because of technical advances in these modalities, or the patient’s stone disease may be detected and treated sooner in this contemporary series compared with older case series. In addition, the changing metabolic composition of SCI patients (with a reduction in struvite stones) has been reported by others,18 and may be related to the reduction in staghorn calculi (and therefore PNLs) in this population. Multiple PNL procedures were necessary for at least 75% of patients undergoing this procedure, similar to other PNL series of SCI patients.8 The morbidity associated with PNLs among SCI patients is significant, with major complication, (such as abscess, pneumothorax, sepsis, fistula, respiratory arrest and death) occurring in 6–20% of patients.4 This is consistent with our results, which demonstrated that 12% of SCI patients required ICU consultation after stone treatment.
Ureteral stents or percutaneous nephrostomy tubes (without stone removal or lithotripsy) were the initial treatment modality in 30% of SCI patients. These patients may have presented with complications of stone disease (such as obstructed urosepsis) that required a temporizing measure, or the physician may not have been able to access to the stone.
Ureteroscopy with lithotripsy seems to be associated with a higher proportion of repeat procedures, unlike the general population.19 In the general population, ureteroscopy for stone disease is usually an outpatient procedure and leads to unplanned admissions or emergency room (ER) visits in <5% of patients.19 However, in our SCI patient cohort, 2/3 of SCI patients required hospital admission, with a median hospital stay of 5 days. This may represent the morbidity of a general anesthetic in this population, or the occurrence of complications related to ureteroscopy.
Small case series from the 1980s to mid 1990s suggested that the overall stone-free rate after SWL in SCI patients is 50–70%; reported hospital stays ranged from 2 to 17 days, and most patients could be treated with 1–2 procedures.4 Complications were rare, and generally related to sepsis or intraoperative cardiovascular changes. Similarly, our cohort tolerated SWL well, with patients rarely requiring hospital admission or ICU consultation, and typically requiring a median of two procedures.
Previous investigators have suggested that SCI patients with higher level lesions have an increased risk of renal stone disease.13 In this contemporary series, we did not demonstrate a significant association between lesion level and stone disease. However, we were not able to control for bladder management method, which may have an important role in renal stone risk.13 The most significant risk factor for these patients was a past history of renal stone disease (with a HR of 15) or bladder stone disease (OR 15), which is in keeping with reports of first time stone formers having a 50% risk of a recurrence within 5–10 years.3 This data seems to suggest renal imaging to detect stone disease is especially important during the first few years after SCI, and among patients with a past history of renal or bladder stones; however, the optimal imaging interval is unknown. At this point, however, it is unknown if screening and treatment of asymptomatic stone disease is appropriate in this population. Yearly renal imaging is recommended for a variety of reasons,20 one of which is for the detection of asymptomatic stone disease. As the majority of these patients did not receive annual renal imaging, this is an area that requires further study and possible evaluation as a target for best practice guidelines. It is interesting to note that self management of bladder function with good continence significantly reduced the risk of renal stone disease. This may be surrogate for a less severe SCI, or reduced urinary tract infection (UTI) risk.
The advantages of this administrative data study include a large patient cohort with population-based sampling across all hospitals in the province of Ontario, and good ascertainment of SCI patients and surgically treated kidney stones. Limitations of our data include the assumption that repeat procedures within 90 days represent a single stone (when they may actually be the treatment of bilateral stones), an intermediate term follow-up period, and the inability to measure potential confounders such as urinary infection, and specific bladder management strategies.8 We could not determine how much of the potential morbidity was actually attributable to the kidney stone procedure itself, or the difficulty of the operative cases. Finally, we were unable to assess the overall incidence of upper tract stones (not just those requiring surgical treatment) because of the variety of clinical presentations and operative, medical and conservative management strategies.
Conclusion
Surgical management of upper tract stone disease was necessary in 3.4 SCI patients/1000 person-years. Ureteroscopy with lithotripsy was the most commonly used modality, and PNL was necessary in only 17% of patients with stone disease.
The past history of either renal or bladder stones significantly increase the risk of renal stone disease after SCI. This should be taken into account in the urologic follow-up and evaluation of SCI patients.
Data archiving
There were no data to deposit.
References
Hansen RB, Biering-Sørensen F, Kristensen JK . Urinary calculi following traumatic spinal cord injury. Scand J Urol Nephrol 2007; 41: 115–119.
Chen Y, DeVivo MJ, Roseman JM . Current trend and risk factors for kidney stones in persons with spinal cord injury: a longitudinal study. Spinal Cord 2000; 38: 346–353.
Ljunghall S . Incidence of upper urinary tract stones. Miner Electrolyte Metab 1987; 13: 220–227.
Ramsey S, McIlhenny C . Evidence-based management of upper tract urolithiasis in the spinal cord-injured patient. Spinal Cord 2011; 49: 948–954.
Rubenstein JN, Gonzalez CM, Blunt LW, Clemens JQ, Nadler RB . Safety and efficacy of percutaneous nephrolithotomy in patients with neurogenic bladder dysfunction. Urology 2004; 63: 636–640.
Symons S, Biyani CS, Bhargava S, Irvine HC, Ellingham J, Cartledge J et al Challenge of percutaneous nephrolithotomy in patients with spinal neuropathy. Int J Urol 2006; 13: 874–879.
Lawrentschuk N, Pan D, Grills R, Rogerson J, Angus D, Webb DR et al Outcome from percutaneous nephrolithotomy in patients with spinal cord injury, using a single-stage dilator for access. BJU Int 2005; 96: 379–384.
Welk B, Fuller A, Razvi H, Denstedt J . Renal stone disease in spinal-cord-injured patients. J Endourol 2012; 26: 954–959.
Roos LL, Gupta S, Soodeen R-A, Jebamani L . Data quality in an information-rich environment: Canada as an example. Can J Aging 2005; 24 (Suppl 1): 153–170.
Raina P, Torrance Rynard V, Wong M, Woodward C . Agreement between self-reported and routinely collected health-care utilization data among seniors. Health Services Res 2002; 37: 751–774.
Stineman MG, Shea JA, Jette A, Tassoni CJ, Ottenbacher KJ, Fiedler R et al The functional independence measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehab 1996; 77: 1101–1108.
Deyo R, Cherkin D, Ciol M . Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992; 45: 613–619.
McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ . Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehab 1999; 80: 1402–1410.
Hollingsworth JM, Wolf JS, Faerber GJ, Roberts WW, Dunn RL, Hollenbeck BK . Understanding the barriers to the dissemination of medical expulsive therapy. J Urol 2010; 184: 2368–2372.
Chen Y, DeVivo MJ, Stover SL, Lloyd LK . Recurrent kidney stone: a 25-year follow-up study in persons with spinal cord injury. Urology 2002; 60: 228–232.
Collins JW, Keeley FX . Is there a role for prophylactic shock wave lithotripsy for asymptomatic calyceal stones? Curr Opin Urol 2002; 12: 281–286.
Donnellan SM, Bolton DM . The impact of contemporary bladder management techniques on struvite calculi associated with spinal cord injury. BJU Int 1999; 84: 280–285.
Matlaga BR, Kim SC, Watkins SL, Kuo RL, Munch LC, Lingeman JE . Changing composition of renal calculi in patients with neurogenic bladder. J Urol 2006; 175: 1716–1719 discussion 1719.
Tang L, Gao X, Xu B, Hou J, Zhang Z, Xu C et al Placement of ureteral stent after uncomplicated ureteroscopy: do we really need it? Urology 2011; 78: 1248–1256.
Consortium for Spinal Cord Medicine. Outcomes following traumatic spinal cord injury: clinical practice guidelines for health-care professionals. J Spinal Cord Med 2000; 23: 289–316.
Acknowledgements
This research was funded by a grant from the Physicians’ Services Inc. Foundation. Dr Welk is supported by a Canadian Urologic Association Scholarship. This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The study was conducted through ICES@Western, which is funded by an operating grant from the Academic Medical Organization of Southwestern Ontario (AMOSO).
Disclaimer
The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES, the Ontario MOHLTC or AMOSO is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Welk, B., Shariff, S., Ordon, M. et al. The surgical management of upper tract stone disease among spinal cord-injured patients. Spinal Cord 51, 457–460 (2013). https://doi.org/10.1038/sc.2013.15
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.15
Keywords
This article is cited by
-
Squamous cell carcinoma of the renal pelvis in a patient with long-term spinal cord injury—a case report
Spinal Cord Series and Cases (2021)
-
Mortality from kidney stone disease (KSD) as reported in the literature over the last two decades: a systematic review
World Journal of Urology (2019)
-
Outcomes of percutaneous nephrolithotomy in spinal cord injury patients as compared to a matched cohort
Urolithiasis (2017)
-
Flexible ureteroscopic laser lithotripsy for upper urinary tract stone disease in patients with spinal cord injury
Urolithiasis (2015)