Key Points
-
Raises awareness of osteoporosis among general dental practitioners.
-
Highlights the impact of osteoporosis upon oral health must be considered by general dental practitioners.
-
Demonstrates greater molar tooth loss in osteoporotic patients.
-
Suggests practitioners should warn osteoporotic patients of this and instigate more intensive preventive regimens.
Abstract
Background Osteopenia and osteoporosis are conditions characterised by a reduction in bone mineral density. There is contradictory evidence whether osteoporotic patients have greater tooth loss than non-osteoporotic patients.
Objective To investigate the association between tooth number and osteoporotic status, taking into account the effect of other confounding variables such as age, smoking status, alcohol consumption and the use of hormone replacement therapy.
Setting Three hundred and fifty-nine patients were recruited from the Manchester region between March 2008 and June 2010.
Subjects and methods Data were collected on osteoporotic status, smoking status, alcohol consumption, age and the use of hormone replacement therapy. Dental panoramic tomographs were taken for each patient and the teeth present were charted and counted. Data were analysed using SPSS software (version 19).
Results Complete data was available for 333 patients. Twenty-seven percent of individuals (90) were classified as osteoporotic. There was a significant relationship between molar tooth number and osteoporotic status (p = 0.017, 95% CI −1.339 to −0.137).
Conclusion Clinicians should inform osteoporotic patients they may be at greater risk of tooth loss and instigate more intensive preventive regimens for these individuals.
Similar content being viewed by others
Introduction
Osteopenia is a condition caused by a progressive reduction in bone mineral density (BMD). There is an alteration of the bone micro-architecture. When a patient's BMD decreases to or below 2.5 standard deviations under the mean peak bone mass that person is classified as osteoporotic. The condition affects one in three post-menopausal women and one in five men over the age of 50. Across both sexes there is a decline in BMD over the age of about 50 years.1 In females this is more pronounced with a reduction of circulating oestrogen following the menopause. The result of this reduction in BMD is a greater likelihood of bone fracture. Though common sites include ribs, spine and wrist, the most notable consequence is fracture of the hip. This is associated with an increased mortality of 30% over the year following injury2 commonly due to increased risk of DVT and pulmonary embolism. The financial burden is also high with average treatment cost for hip fractures approaching £12,163 per patient.3 It is thought 2% of men and 3% of women will have suffered a hip fracture by the age of 75.4
Changes in BMD also have an impact upon oral health. There is considerable variation in the BMD of trabecular and cortical bone of the mandible among individuals.5,6 Osteoporosis may have an impact upon this variation. Using a variety of methodologies, a number of studies have demonstrated significant relationships between jaw measurements (bone mass, bone mineral content, BMD) and those at other skeletal sites.6,7,8,9,10,11,12,13 Thus there is a strong argument that osteoporosis and osteopenic states may have a negative influence upon the bone quantity and quality of the mandible and maxilla.14 Indeed it is possible to use mandibular cortical width measurements on dental panoramic radiographs as a screening tool for skeletal osteoporosis.15,16
If osteopenic and osteoporotic conditions influence the bone mineral content of the mandible and maxilla then this may be most obvious in those who are edentulous.17,18 Kribbs et al. failed to demonstrate a correlation with skeletal osteopenia and residual ridge reduction but there was a relationship demonstrated between osteopenia and residual ridge density, particularly in the edentulous mandible.19 Other authors13,20 have found a reduction in the alveolar ridge height in patients with reduced BMD but periosteal resorption and a change in the external dimensions of bone are not a characteristic features of osteoporosis.
In dentate patients there have been further studies that indicate osteoporosis may be linked to tooth loss. Astrom et al. demonstrated a correlation between tooth loss and hip fracture incidence.21 This retrospective study was based on the known correlation between hip fracture and osteoporosis. In this study no formal examination was made of patient's BMD or osteoporotic status and their dental status was arbitrarily classified into many teeth, moderate tooth loss and considerable tooth loss. Drozdzowska et al.22 also demonstrated a correlation with tooth count and hip BMD though the numbers recruited were small. May et al.23 performed a study on 1,482 patients. All patients were sent a questionnaire and brought in for skeletal BMD assessment. An association was shown between tooth loss and BMD in men but the results of this study are undermined by the self-reported nature of the questionnaire format. In a large multi-centre study of 650 patients, of whom 140 were classified as osteoporotic, a significant correlation was demonstrated between tooth number and osteoporotic status after accounting for age and smoking status.24
The primary aim of this study was to assess whether there is a relationship between the osteoporotic status of patients and the number of their teeth. Age, smoking status, alcohol consumption and the use of hormone replacement therapy are known in the literature to affect tooth number and were also included as explanatory variables in the regression model. The secondary aim was to assess whether molar teeth are disproportionately affected in the osteoporotic patients.
Materials and methods
The study lasted two years and three months, with patient recruitment commencing in March 2008 and ending in June 2010. The patients' examinations were performed within two months of recruitment so that the data collection period was completed in August 2010. This was a cross-sectional study of volunteer subjects recruited from Manchester (UK) and the surrounding regions.
Participants
The eligibility criteria for the study were: female, aged between 45-68 years inclusive and who had undergone a dual energy X-ray absorptiometry (DXA) scan of the proximal femur and lumbar spine in the previous three months at one of two hospital sites. Patients were initially identified from the databases held at both hospitals. The exclusion criteria were: individuals who had a medical condition that made it impossible for them to brush their own teeth (as in stroke, paralysis etc), leukaemia, diabetes, chemotherapy and those taking intravenous bisphosphonates. If patients fulfilled the inclusion and exclusion criteria they were sent an information leaflet and were invited to participate in the study. Ethical approval was granted (Number 07/Q1402/58) and informed consent obtained.
DXA scans of the lumbar spine and proximal femur were performed on one of three scanners located in two hospitals: two Hologic Discovery scanners (Hologic Inc., Bedford MA, USA) or a GE Lunar Prodigy (GE Healthcare, Waukesha WI, USA). Measurements of BMD and T scores were recorded for L1-L4, femoral neck and total hip. As the patients were measured on three different scanners it was necessary to cross-calibrate the patient data. To allow cross-calibration the European Spine Phantom (ESP) was used on each scanner at the start and end of the study period. Measurements from the ESP were used to standardise measurements between different manufacturers' scanners using the method described by Pearson et al.25 T and Z scores were calculated using Hologic reference data for the lumbar spine and NHANES reference data for the proximal femur.26 Subjects were defined as having osteoporosis when they had a T-score of −2.5 or lower at any one of the sites measured.
The patients were allocated a unique patient identifier to remove all patient identifiable information. Information was gathered on patients' age, smoking status, alcohol consumption and whether they were on hormone replacement therapy or not. The FRAX system for risk analysis of exposure status for alcohol consumption and smoking status was used. Using the FRAX system, patients are categorised as either smokers or non-smokers and alcohol consumption is classified as 3 or more units of alcohol per day or alternatively less than this.27 All patients received a dental panoramic radiographic examination using a Planmeca PM2002CC (Planmeca Oy, Helsinki, Finland), Kodak GP Storage Phosphor Screens (Carestream Health Inc, New York, USA) and a Direct View CR850 digital processor (Carestream Health Inc, New York, USA). The radiographs were stored on an encrypted hard drive. Each radiograph was reviewed by an experienced clinician blind to the osteoporotic status of the patients. The clinician (JD) had been calibrated with another member of the study design team (HD). The following information was gathered.
-
Total number of teeth
-
Total number of maxillary teeth
-
Total number of maxillary incisors, canines, premolars and molars
-
Total number of mandibular teeth
-
Total number of mandibular incisors, canines, premolars and molars.
The presence of implants was recorded. Impacted teeth were not included in the analysis. Retained roots were included in the analysis.
Sample size calculation
The study reported here formed a part of a larger research project focused on the impact of osteoporosis on periodontal health. The prevalence of severe periodontal disease in those aged 40-70 years in the general community is about 10-20%.28,29 A sample size of 540 patients was calculated to detect a difference of 10% in periodontal disease prevalence between osteoporotic and control groups with 80% power and a 5% significance level. This 10% represents the difference in the prevalence of severe periodontal disease of 15% in the non-osteoporotic group and 25% in the osteoporotic group.
Statistical analysis
Once the data was captured the osteoporotic status of the patients was recorded and the data inputted into the Statistical Package for Social Sciences (SPSS Inc, Chicago, Ill, USA). Multiple linear regression analysis was undertaken for both primary and secondary outcome measures (tooth number and molar number, respectively) with the predictors being osteoporotic status, age, smoking status, alcohol consumption and the use of hormone replacement therapy (analysis including all potential covariates). Statistical significance was set at 0.05. Casewise diagnostics were performed on outliers.
Results
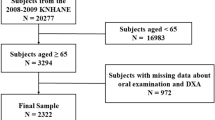
Recruitment of 398 subjects was achieved during the course of the study. Of these, DXA data were accessible for 380. Dental radiographic and clinical information was available for 359 patients but, of these, radiographs of two subjects were non-diagnostic and thus discarded. A complete set of DXA data, clinical information and dental radiographs were available for 333 subjects, of whom 90 (27%) were classified in the osteoporosis group and 243 (73%) as having normal BMD. Table 1 shows the characteristics of the two groups.
Tooth number and osteoporotic status
The total number of patients for analysis was 333. Significant negative correlations were found between: osteoporosis and tooth number (Pearson correlation coefficient −0.112: p = 0.02), tooth number and smoking status (Pearson correlation coefficient −0.109: p = 0.023) and age and tooth number (Pearson correlation coefficient −0.243: p = 0.0001). The R square value was 0.082. The R square change value was 0.005. This was not significant (F change = 0.852: p = 0.427). The F-ratio was stronger when smoking and age were included in the regression. When assessing the unstandardised coefficients osteoporotic status alone was not a significant predictor of tooth number (unstandardised coefficient −0.740: p = 0.171, 95% confidence interval (CI) for the regression coefficient (RC) −1.801 to 0.321). In all analyses collinearity indicated no significant bias (eigenvalue 0.470, condition index 2.566). Six cases were highlighted as outliers. Cooks distance, centered leverage values and Mahalanobis distance did not demonstrate any significance to these anomalous outliers. See Figure 1 for a box plot of tooth number and osteoporosis status.
Molar number and osteoporotic status:
The total number of patients equalled 333. Significant negative correlations were found between: age and molar number (Pearson correlation coefficient −0.264: p = 0.0001), osteoporosis and tooth number (Pearson correlation coefficient −0.170: p = 0.001), smoking status and tooth number (Pearson correlation coefficient −0.156: p = 0.002). The R square value was 0.123. The F-ratio was 9.125 and this was significant (p = 0.0001). When assessing the unstandardised coefficients age, smoking status and osteoporotic status were all predictive of tooth loss (age unstandardised coefficient −0.124: p = 0.0001, 95% CI RC −0.175 to −0.074; smoking status unstandardised coefficient −1.225: p = 0.001, 95% CI RC −1.975 to −0.474 and osteoporotic status unstandardised coefficient −0.751: p = 0.017, 95% CI RC −1.339 to −0.137). In all analyses collinearity indicated no significant bias (eigenvalue: 0.470, condition index: 2.566). One case was highlighted as an outlier. Cooks distance, centered leverage values and Mahalanobis distance did not demonstrate any significance to this anomaly.
Summary of the data:
When analysing the total number of teeth and osteoporotic status, positive osteoporotic status, increasing age and positive smoking status were all shown to be significantly correlated with reduced tooth number. When the regression technique was used osteoporosis was no longer a significant predictor of tooth loss. When analysing the total number of molars, a positive osteoporotic status, increasing age and positive smoking status were all shown to be correlated with reduced molar number. When the regression technique was used osteoporotic status remained a significant predictor of molar tooth loss. In this analysis the influence of osteoporosis status, though significant, remained small: there are other more influential factors associated with molar tooth loss that were not accounted for in this study. In both analyses the data was demonstrated to be normally distributed and free of significant bias.
Discussion
Osteoporotic status, smoking status and age have significant correlations with mean tooth number. Further significant correlations were found between molar number and osteoporosis and age and smoking status. All the correlations were negative indicating an inverse relationship. This analysis does not prove causality but simply observed association.
The regression model demonstrated a significant association between osteoporotic status, age, smoking and molar tooth number. However, R square for the multiple linear regression indicates this model of variables (age, smoking status, osteoporotic status, HRT and alcohol consumption) accounts for only 12% of molar tooth loss variance. Again, the magnitude of these correlations demonstrates other variables exist to explain tooth loss.
There are limitations within this study that should be recognised. Firstly the study was known to be underpowered. Recruitment was less than the original power calculation recommended. This was a single centre study so extrapolation to a wider population must acknowledge this. Similar studies have used a multi-centre approach with data collection from multiple countries.24,30 Furthermore, cross sectional studies with this design only show prevalence data regarding exposures and disease. As osteoporosis is a chronic disease it is likely that those with the condition in this cohort may have had it for some time. Conversely, others may not. It is thus more difficult to establish and assess the impact of disease history upon the outcome measures. Prospective longitudinal studies would allow a more accurate assessment of causality accounting for known covariates. Such studies are often prohibitively complex in both design and cost.
A further criticism pertains to completeness of data. Regression analysis did not, however, pick up any significant bias in the data. Histograms, normal P-P plots and scatterplots all indicated the data to be normally distributed, a prerequisite for multiple linear regression. Outlying data were analysed to determine if they had an influential effect on the results. Casewise diagnostics allowed the researchers to go back to the data and assess these cases individually. No anomalies were detected. Several cases also had incomplete data. There were two radiographs that were non-diagnostic and missing data on osteoporosis exposure status for 22 patients. A further two patients had incomplete data on HRT status. The regression modelling does not account for missing data and thus we must acknowledge this when considering the outcomes as it may weaken the resultant significance. The total number of subjects for the regression analysis was 333.
The data on exposure status is subject to limitations. The FRAX system uses a categorical measure of smoking status and alcohol consumption.27 Both these risk factors have been demonstrated to be dose dependent in their effect upon osteoporotic disease patterns.31,32 It could therefore be argued that such simple categorical data capture may not carry sufficient information for meaningful calculation of effect size. It is, however, important to realise that self reported information upon smoking status and alcohol consumption are invariably open to responder bias, often underestimating the true value. Simple closed categorical questions may be more likely to encourage truthful responses.
The influence of osteoporosis upon the micro-architecture of bone in the mandible and maxilla is well supported in the literature6,7,8,9,33 but the precise pathophysiology of this relationship has not, however, been ascertained. The relationship is difficult to establish owing to the influence of confounding factors such as age, smoking status, race, menopausal age, oral hygiene and hormone intake.34
Several studies have indicated that reduced skeletal BMD is associated with premature tooth loss.24,33,35,36,37,38,39,40 Such patterns of tooth loss may be correlated with periodontal attachment loss/disease and osteoporotic status.6,33,40,41,42,43,44,45,46,47,48,49,50 Osteopenic conditions may predispose to clinical attachment loss. The model, as proposed by Genco and Grossi51 is based upon the elevated levels of cytokines associated with postmenopausal oestrogen deficiency. A deficiency in oestrogen leads to an upregulation of macrophages and osteoblasts, which in turn produces inflammatory mediators such as interleukins, TNF alpha and granulocyte-macrophage colony stimulating factor. This results in a generalised increased bone collagen destruction and bone resorption. Interleukin 1B has been demonstrated to be integral to the resorption of periapical and periodontal dental hard tissues.52 Yoshihara et al., however, found a weak correlation between BMD and periodontal disease.43 This has been supported by other studies.6,53
A second explanatory model addresses the influence of oestrogen upon bony remodelling and osteoclast function. Oestrogen has been shown to upregulate osteoprotegrin. Osteoprotegrin inhibits receptor activator of nuclear factor kappa B ligand (RANKL) and this is known to reduce alveolar bone breakdown.54 RANKL is liberated from osteoblasts and stromal cells and interacts with receptors in macrophages and monocytes inducing fusion of these cells to become osteoclasts. RANKL expression can be stimulated by interleukin 1B.55,56 As noted previously interleukin 1B has an established role in periodontal alveolar breakdown.52,57 Thus it could be postulated that accelerated periodontal breakdown in osteoporotic patients possibly arises from a combination of elevated inflammatory responses and locally increased resorptive potential.
The significance of osteoporotic status upon molar number must also be considered. Taguchi et al. found a significant difference in BMD at the third lumbar vertebrae and posterior tooth loss.38 In this investigation posterior teeth were defined as premolars and molars. The authors speculated this may be correlated with increased occlusal forces rather than periodontal disease. Further studies have demonstrated this correlation in resistance to mechanical loading and BMD.58,59 Thus, reduced bone mass and the greater occlusal forces associated with posterior teeth has been suggested as a possible explanation for increased molar loss.38 Furthermore, teeth with furcational involvement are at a significantly greater risk of premature tooth loss.60,61,62,63 Therefore one may expect more multi-rooted teeth to be lost in patients with osteoporosis if there is a correlation between periodontal disease and osteoporosis.
There have, however, been studies that fail to show correlations between osteoporotic status and tooth number.23,64,65 Bollen et al.66 investigated the association between osteoporotic fracture and tooth loss. Once confounding factors have been accounted for they found no association between either tooth loss or changes in alveolar height and fracture history. This is based on the assumption that osteoporotic status can be derived from a positive fracture history, but a reduced BMD, as a result of osteoporosis, is only one risk factor for fracture. In a larger multi-centre study of early post menopausal women, Earnshaw30 found no association with BMD and tooth loss. Their results were based on Chi Square calculations and not regression analysis; which is known to be a less powerful statistical technique. Furthermore mean tooth number was not used, rather a grouping classification of tooth loss as described by Anstrom et al.21
Conclusion
There is a significant correlation between tooth loss and osteoporosis, but the strength of this correlation is weak. It is more probable that local and other systemic factors exert greater influences upon tooth loss. There is a statistically significant relationship between molar loss and osteoporotic status.
Implications for research
Evidence for a correlation between osteoporosis and tooth loss remains equivocal. Further multi-centre studies are required to investigate the oral impact of osteoporosis.
Implications for practice
Clinicians should inform patients diagnosed as osteoporotic that they may be at greater risk of losing molar teeth in the future. These patients should be reviewed more frequently and their oral hygiene measures reinforced so as to prevent tooth loss.
References
Roberts M, Yuan J, Graham J, Jacobs R, Devlin H . Changes in mandibular cortical width measurements with age in men and women. Osteoporos Int 2011; 22: 1915–1925.
Parker M J, Anand J K . What is the true mortality of hip fractures? Public Health 1991; 105: 443–446.
Lawrence T M, White C T, Wenn R, Moran C G . The current hospital costs of treating hip fracture. Injury 2005; 36: 88–91.
Law M R, Wald N J, Meade T W . Strategies for prevention of osteoporosis and hip fracture. BMJ 1991; 303: 453–459.
von Wowern N, Stoltze K . Sex and age differences in bone morphology of mandible. Scand J Dent Res 1978; 86: 478–485.
von Wowern N, Klausen B, Kollerup G . Osteoporosis: a risk factor in periodontal diease. J Periodontol 1994; 65: 1134–1138.
Jeffcoat M K, Lewis C E, Reddy M S, Wang C Y, Redford M . Post-menopausal bone loss and its relationship to oral bone loss. Perio 2000 2000; 23: 94–102.
Southard K A, Southard T E, Schlechte J A, Meis P A . The relationship between the density of the alveolar processes and that of post-cranial bone. J Dent Res 2000; 79: 964–969.
Jacobs R, Ghyselen J, Koninckx P, van Steenberghe D . Long-term bone mass evaluation of mandible and lumbar spine in a group of women receiving hormone replacement therapy. Eur J Oral Sci 1996; 104: 10–16.
Kribbs P J, Chesnut C H 3rd, Ott S M, Kilcoyne R F . Relationships between mandibular and skeletal bone in a population of normal women. J Prosthet Dent 1990; 63: 86–89.
Kribbs P J, Chesnut C H 3rd, Ott S M, Kilcoyne R F . Relationships between mandibular and skeletal bone in an osteoporotic population. J Prosthet Dent 1989; 62: 703–707.
Kribbs P J . Comparison of mandibular bone in normal and osteoporotic women. J Prosthet Dent 1990; 63: 218–222.
Klemetti E, Vainio P . Effect of bone mineral density in skeleton and mandible on extraction of teeth and clinical alveolar height. J Prosthet Dent 1993; 70: 21–25.
Bollen A M, Taguchi A, Hujoel P P, Hollender L G . Case-control study on self-reported osteoporotic fractures and mandibular cortical bone. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 518–524.
Horner K, Devlin H, Harvey L . Detecting patients with low skeletal bone mass. J Dent 2002; 30: 171–175.
Karayianni K, Horner K, Mitsea A et al. Accuracy in osteoporosis diagnosis of a combination of mandibular cortical width measurement on dental panoramic radiographs and a clinical risk index (OSIRIS): The OSTEODENT project. Bone 2007; 40: 223–229.
Atwood D . Some clinical factors related to the rate of resorption of residual ridges. J Prosthet Dent 2001; 86: 119–125.
Atwood D A . Reduction of residual ridges: a major oral disease entity. J Prosthet Dent 1971; 26: 266–279.
Kribbs P J, Smith D E, Chesnut C H 3rd. Oral findings in osteoporosis. Part II: relationship between residual ridge and alveolar bone resorption and generalized skeletal osteopenia. J Prosthet Dent 1983; 50: 719–724.
Bays R A, Weinstein R S . Systemic bone disease in patients with mandibular atrophy. J Oral Maxillofac Surg 1982; 40: 270–272.
Aström J, Bäckström C, Thidevall G . Tooth loss and hip fractures in the elderly. J Bone Joint Surg Br 1990; 72: 324–325.
Drozdzowska B, Pluskiewicz W, Michno M . Tooth count in elderly women in relation to their skeletal status. Maturitas 2006; 55: 126–131.
May H, Reader R, Murphy S, Khaw K T . Self-reported tooth loss and bone mineral density in older men and women. Age Ageing 1995; 24: 217–221.
Nicopoulou-Karayianni K, Tzoutzoukos P, Mitsea A et al. Tooth loss and osteoporosis: the OSTEODENT study. J Clin Periodontol 2009; 36: 190–197.
Pearson J, Dequeker J, Reeve J et al. Dual X-ray absorptiometry of the proximal femur- normal European values standardized with the European spine phantom. J Bone Miner Res 1995; 10: 315–324.
Looker A C, Wahner H W, Dunn W L et al. Updated data on proximal femur bone mineral levels of US adults. Osteoporosis Int 1998; 8: 468–489.
Kanis J A, Johnell O, Oden A, Johansson H, McCloskey E . FRAX and the assessment of fracture probability in men and women from the UK. Osteoporosis Int 2008; 19: 385–397.
Locker D, Slade G D, Murray H . Epidemiology of periodontal disease among older adults: a review. Periodontal 2000 1998; 16: 16–33.
Papapanou P . Epidemiology of periodontal diseases: an update. J Int Acad Periodontol 1999; 1: 110–116.
Earnshaw S A, Keating N, Hosking D J et al. Tooth counts do not predict bone mineral density in early postmenopausal Caucasian women. EPIC study group. Int J Epidemiol 1998; 27: 479–483.
Ward K, Klesges R C . A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif Tissue Int 2001; 68: 259–270.
Nielsen H K, Lundby L, Rasmussen K, Charles P, Hansen C . Alcohol decreases serum osteocalcin in a dose-dependent way in normal subjects. Calcif Tissue Int 1990; 46: 173–178.
Streckfus C F, Johnson R B, Nick T, Tsao A, Tucci M . Comparison of alveolar bone loss, alveolar bone density and second metacarpal bone density, salivary and gingival crevicular fluid interleukin-6 concentrations in healthy premenopausal and postmenopausal women on estrogen therapy. J Gerontol A Biol Sci Med Sci 1997; 52: M343–M351.
Von Wowern N . General and oral aspects of osteoporosis: a review. Clin Oral Investigations 2001; 5: 71–82.
Daniell H W . Postmenopausal tooth loss. Contributions to edentulism by osteoporosis and cigarette smoking. Arch Intern Med 1983; 143: 1678–1682.
Jeffcoat M K . Osteoporosis: a possible modifying factor in oral bone loss. Ann Periodontol 1998; 3: 312–321.
Krall E A, Dawson-Hughes B, Papas A, Garcia R I . Tooth loss and skeletal bone density in healthy postmenopausal women. Osteoporosis Int 1994; 4: 104–109.
Taguchi A, Suei Y, Ohtsuka M, Otani K, Tanimoto K, Hollender L G . Relationship between bone mineral density and tooth loss in elderly Japanese women. Dentomaxillofacial Radiol 1999; 28: 219–223.
Taguchi A, Tanimoto K, Suei Y, Otani K, Wada T . Oral signs as indicators of possible osteoporosis in elderly women. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 80: 612–616.
Inagaki K, Kurosu Y, Kamiya T et al. Low metacarpal bone density, tooth loss, and periodontal disease in Japanese women. J Dent Res 2001; 80: 1818–1222.
Tezal M, Wactawski-Wende J, Grossi S G, Ho A W, Dunford R, Genco R J . The relationship between bone mineral density and periodontitis in postmenopausal women. J Periodontol 2000; 71: 1492–1498.
Mohammad A R, Hooper D A, Vermilyea S G, Mariotti A, Preshaw P M . An investigation of the relationship between systemic bone density and clinical periodontal status in post-menopausal Asian-American women. Int Dent J 2003; 53: 121–125.
Yoshihara A, Seida Y, Hanada N, Miyazaki H . A longitudinal study of the relationship between periodontal disease and bone mineral density in community-dwelling older adults. J Clin Periodontol 2004; 31: 680–684.
Hildebolt C, Pilgram T K, Yokoyama-Crothers N et al. The pattern of alveolar crest height change in healthy postmenopausal women after 3 years of hormone/estrogen replacement therapy. J Periodontol 2002; 73: 1279–1284.
Brennan R M, Genco R J, Hovey K M, Trevisan M, Wactawski-Wende J . Clinical attachment loss, systemic bone density, and subgingival calculus in postmenopausal women. J Periodontol 2007; 78: 2104–2111.
Payne J B, Reinhardt R A, Nummikoski P V, Patil K D . Longitudinal alveolar bone loss in postmenopausal osteoporotic/osteopenic women. Osteoporosis Int 1999; 10: 34–40.
Reinhardt R A, Payne J B, Maze C A, Patil K D, Gallaher S J, Mattson J S . Influence of estrogen and osteopenia/osteoporosis on clinical periodontitis in postmenopausal women. J Periodontol 1999; 70: 823–828.
Klemetti E, Collin H L, Forss H, Markkanen H, Lassila V . Mineral status of skeletal and advanced periodontal disease. J Clin Periodontol 1994; 21: 184–188.
Genco R, Löe H . The role of systemic conditions in periodontal disease. Perio 2000 1993; 2: 98–116.
Offenbacher S . Periodontal diseases: pathogenesis. Ann Periodontol 1996; 10: 821–828.
Genco R J, Grossi S G . Is estrogen deficiency a risk factor for periodontal disease? Compend Contin Educ Dent Suppl 1998; S23–S29.
Stashenko P, Jandinski J J, Fujiyoshi P, Rynah J, Socranksy S S . Tissue levels of bone resorptive cytokines in periodontal disease. J Periodontol 1991; 62: 504–509.
Tezal M, Wactawski-Wende J, Grossi S G, Ho A W, Dunford R, Genco R J . The relationship between bone mineral density and periodontitis in postmenopausal women. J Periodontol 2000; 71: 1492–1498.
Teng Y T, Nguyen H, Gao X et al. Functional human T-cell immunity and osteoprotegerin ligand control alveolar bone destruction in periodontal infection. J Clin Invest 2000; 106: R59–R67.
Hofbauer L C, Khosla S, Dunstan C R, Lacey D L, Boyle W J, Riggs B L . The roles of osteoprotegrin and osteoprotegrin ligand in the paracrine regulation of bone resorption. J Bone Min Res 2000; 15: 2–12.
Hofbauer L C, Lacey D L, Dunstan C R, Spelsberg T C, Riggs B L, Khosla S . Interleukin-1-beta and tumour necrosis factor alpha but not interleukin-6, stimulate osteoprotegrin ligand gene expression in human osteoblastic cells. Bone 1999; 25: 255–259.
Stashenko P, Yu S M, Wang C Y . Kinetics of immune cell and bone resorptive responses to endodontic infections. J Endod 1992; 18: 422–426.
Biggemann M, Hilweg D, Seidel S, Horst M, Brinckmann P . Risk of vertebral insufficiency fractures in relation to compressive strength predicted by quantitative computed tomography. Euro J Radiol 1991; 13: 6–10.
Edmondston S J, Singer K P, Day R E, Price R I, Breidahl P D . Ex vivo estimation of thoracolumbar vertebral body compressive strength: the relative contributions of bone densitometry and vertebral morphometry. Osteoporosis Int 1997; 7: 142–148.
Wang H L, Burgett F G, Shyr Y, Ramfjord S . The influence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J Periodontol 1994; 65: 25–29.
Ong G . Periodontal disease and tooth loss. Int Dent J 1998; 48 (Suppl 1): 233–238.
König J, Plagmann H C, Rühling A, Kocker T . Tooth loss and pocket probing in compliant periodontally treated patients: a retrospective analysis. J Clin Periodontol 2002; 29: 1092–1100.
Hirschfeld L, Wasserman B . A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol 1978; 49: 225–237.
Elders P, Habets L L, ƒNetelenbos J C, van der Linden L W, van der Stelt P F . The relation between periodontitis and systemic bone mass in women between 46 and 55 years of age. J Clin Periodontol 1992; 19: 492–496.
Weyant R J, Pearlstein M E, Churak A P, Forrest K, Famili P, Cauley J A . The association between osteopenia and periodontal attachment loss in older women. J Periodontol 1999; 70: 982–991.
Bollen A M, Taguchi A, Hujoel P P, Hollender L G . Number of teeth and residual alveolar ridge height in subjects with a history of self-reported osteoporotic fractures. Osteoporosis Int 2004; 15: 970–974.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Darcey, J., Horner, K., Walsh, T. et al. Tooth loss and osteoporosis: to assess the association between osteoporosis status and tooth number. Br Dent J 214, E10 (2013). https://doi.org/10.1038/sj.bdj.2013.165
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.165
This article is cited by
-
Association between oral health and locomotive syndrome: a cross-sectional study in Japanese adults
BMC Geriatrics (2023)
-
Functional tooth number in the posterior region associated serum ucOC levels
International Journal of Implant Dentistry (2022)
-
Loss of KDM4B impairs osteogenic differentiation of OMSCs and promotes oral bone aging
International Journal of Oral Science (2022)
-
Oral health and emotional well-being in premenopausal and postmenopausal women: a cross-sectional cohort study
BMC Women's Health (2021)
-
Factors associated with having less than 20 natural teeth in rural adults: a cross-sectional study
BMC Oral Health (2015)