Key Points
-
Points out that there is no agreed definition for quality in dentistry.
-
Suggests that without an agreed definition it is difficult to measure quality and therefore difficult to improve quality in a systematic way.
-
Stresses the need for a conceptual understanding of the concept of quality to support the development of a definition and measuring instruments.
Abstract
In the first paper of a series exploring quality in primary dental care a definition for quality in dentistry is sought. There is a little agreement in academic literature as to what quality really means in primary dental care and without a true understanding it is difficult to measure and improve quality in a systematic way. 'Quality' of healthcare in dentistry will mean different things to practitioners, policy makers and patients but a framework could be modelled on other definitions within different healthcare sectors, with focus on access, equity and overall healthcare experience.
Similar content being viewed by others
Introduction
The quality of healthcare is a complex concept. Although all stakeholders want to promote, provide or receive quality dental care our understanding of this concept in dentistry is underdeveloped. There is no agreed or unique definition of quality of care in primary care settings.1,2,3,4 This applies more so to dental practice than to medical practice, as most of the literature and evidence base for defining quality of care in primary care settings comes from general medical practice and management of healthcare systems, rather than directly from oral healthcare settings. Dentistry, in the UK or internationally, whether it is provided through state funded-services, privately or via insurance schemes, has no agreed understanding of, or indeed much literature on, what constitutes high quality care.
This paper, the first in a series of three, discusses the notion of quality of care in dentistry, set against the context of existing definitions of quality of care generally in other healthcare services. In so doing it addresses what is known about quality in primary dental care and whether quality, as a concept in dentistry, differs from other healthcare services. The paper will outline the attributes of quality and the different perspectives of stakeholder groups (public, patients, dentists and dental care professionals (DCPs), commissioners, and policy-makers) and comment on the policy implications for a clear agreed definition of quality. It will end by describing how a framework for defining quality for dentistry could be developed and some of the key concepts that it would include. The second paper in this series will discuss how to measure quality and the final paper in the series will look at quality improvement within primary dental care.
The starting point for any attempt to improve quality is to get an agreed understanding of what this concept means, usually through a clearly stated definition. As Donabedian asserted correctly in 1985 'We cannot assess quality until we have decided with what meanings to invest the concept. A clear definition of quality is the foundation upon which everything is built'.5 Any such definition must be grounded in a conceptual framework that describes the totality of quality of primary dental care, this will determine which aspects of care are included in a set of any quality indicators and what they measure. Once you can measure quality of care acceptably, validly and reliably you can start to improve it.
Different perspectives of various stakeholders
There are various definitions of healthcare quality depending on the perspective from which healthcare is viewed.2,6,7 For primary dental care the stakeholders are the public, patients, dentists and DCPs, commissioners and policy makers. Importantly, it may not be possible, or indeed desirable, to find an agreed definition that would satisfy all users of a definition. Moreover, it cannot be presumed that one stakeholder group's perspective necessarily represents, or indeed, takes precedence over another group's views. For example, health professionals may focus on professional standards and technical aspects of care, patients may concentrate on communication skills and continuity of care and managers may prioritise efficiency and, increasingly, the outcomes of care. Even if the same aspects of care are assessed an indicator can be valued differently by different stakeholder groups, for example, health professionals and managers and patients are likely to value efficiency differently.8
The bigger primary care picture
Dentistry is predominantly a primary care service. There are therefore many parallels between general medical practice and general dental practice. The Declaration of Alma Ata in 19789 reaffirmed the World Health Organisation (WHO) definition of health and also defined the meaning of primary care, urging governments to develop primary care and incorporate the primary care approach into their healthcare systems. Worldwide evidence indicates that the primary care approach leads to better health outcomes for lower costs.10 Starfield11 identified four cardinal features of primary care:
-
First contact between the healthcare system and members of the public
-
Ongoing, person-centred care over time
-
Comprehensiveness – addressing all of the commonly encountered needs of the population
-
Co-ordination or integration – referral to specialists for patients who have an unusual or uncommon condition.
Primary care is greater therefore than merely the clinical treatment of patients and quality is not confined to clinical outcomes but also encompasses how a service is organised and delivered according to such pivotal features. When definitions of quality have been considered in the literature there is an underlying assumption that clinical care and the broader features of a service are delivered by qualified, competent and up-to-date practitioners who recognise their own limitations and draw appropriately on the strengths of others.1 These assumptions are important as they set minimum standards and conceptually separate out quality from individual professional under-performance and misconduct.
Defining quality of care: generic, dimensional, individual, population
Attempts to define quality of healthcare basically fall in to two camps: generic and disaggregated.2 The former seek to define all aspects of quality in a single all encompassing (hopefully succinct) statement, whereas the latter disaggregated definitions seek to define separate and multiple dimensions of quality.
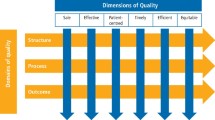
Some definitions of quality have embraced simplistic or generic statements; for example, relating to the care healthcare professionals would want to receive if they themselves became sick.12 However, generic definitions are often of limited practical value in terms of identifying key processes and outcomes and trade both sensitivity and specificity for generalisability. Attempts to develop all-embracing definitions of quality lead to the production of meaningless and blunt measures vulnerable to contamination by a wide range of factors at both the individual (patient) and environmental (society) levels: 'There is a danger of enlarging the definition of quality so much that it loses distinctiveness and analytic utility, becoming almost a slogan which means nearly anything anyone chooses it to mean'.6 Generating an all-encompassing definition is also difficult because of the contextual nature of quality – different stakeholder groups and even people within the same stakeholder group often disagree about the essence of quality. The concept of quality is therefore most frequently proposed and defined as a multidimensional one.7,13,14 Maxwell suggested six dimensions of quality (access, effectiveness, efficiency, equity, relevance and social acceptability) and Donabedian suggested seven dimensions (acceptability, effectiveness, efficacy, efficiency, equity, legitimacy and optimality). Such dimensions or attributes, in whatever combination or taken in isolation, constitute a definition of quality of care.15 Most frequently these dimensions or attributes are placed within the structure-process-outcome model advocated by Donabedian (Fig 1).6,13
The triad of structure, process and outcome was intended to be 'approaches to the acquisition of information about the presence or absence of the attributes that constitute or define quality'.6 In other words, it facilitates the measurement of quality and will be considered with some of the technical issues concerning measurement such as validity and reliability in second paper of this series. However, simply listing attributes or dimensions does not provide an adequate definition of quality in itself, as simple listing can describe properties without inherent value.16 As such, a multi-dimensional approach within a generic definition has been proposed.2 In addition, initial generic definitions have evolved into multidimensional definitions. For example the Institute of Medicine defined quality in 1990 as 'The degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge”,17 which later evolved into identifying dimensions of safety, effectiveness, patient-centeredness, timeliness, efficiency and equity.18
There is significant overlap in the dimensions within published definitions of quality of healthcare, with a prominent focus on integration, access, effectiveness, equity and efficiency as key attributes of health care quality.2 Patients may trade off one attribute for another depending on their needs at any one time; for example, trading continuity of care (a patient seeing their regular dentist for a routine check-up) and speed of access (the patient wanting to see any available dentist if they are in pain). This trade-off between access and continuity has been found in other studies19 and can be positive when patients receive timely and effective care20 but negative if they 'accept a decreased value of one attribute for an increase in another',21 for example persistent unavailability of the dentist a patient usually sees in return for walk-in pain relief.
Quality from the perspective of the individual patient should be considered separately from the perspective of the general public or the practice-population. Campbell and colleagues summarised quality for individual patients as; 'whether individuals can access the effective care they need with a patient-centred focus on maximising health outcomes', but that this has to be set against a population context that feeds in the concepts of equity and efficiency.2 This has been described as simplistic,22 but others have emphasised the dual foci of holistic, personalised care for individuals that is provided equitably at a population level.1,23 There is also a difference between horizontal equity: care that is equally accessible and equally effective for patients with the same degree of illness; and vertical equity: care that provides better access for patients with greater need.2,24
Trust and accountability
All patients presenting to any dental practice anywhere in Europe or worldwide have a right to safe, quality care. This requires a transparent definition of the attributes and measures to enable quality assurance, that is to objectively demonstrate that high quality, safe care is being provided.25 To do this requires a focus on population level measures using quality control (a process to maintain standards) but this provides values for the average patient rather than individual patients. In order to provide personalised, patient-centred care at the individual level, there is also a need for clinical autonomy and trust within a practitioner-patient therapeutic relationship.26 This is because there is no such thing as an 'average' patient.4,25,27,28 As such, maximising quality of care for populations should not be at the expense of jeopardising the therapeutic relationship between individual patients and health practitioners.2,25
Heath has described how 'biomedical science has made prodigious advances by viewing the body as a standardised object' and while 'this works relatively well in some aspects of specialist practice, it works much less so in general practice' because of 'the limitations of treating human individuals as interchangeable units'.28 General medical practitioners are often presented with 'unexplained symptoms and the complex mess',4 which is the day-to-day reality of the immensely diverse problems presented by successive individual patients, often with multiple morbidity.25 Therefore, within general medical practice quality of care as a concept has most meaning and is at its purest as a patient-centred approach related to individual patients; although this must be placed in the context of providing healthcare for populations.2 However, the measurement of quality is most often reported as 'average' patients within a population.2,25 How do these features apply to quality in primary dental care? Is it about personalised individual care or is it more concerned with the biomedical treatment of standardised problems using predetermined care pathways? Is it more about access and efficiency?
What is not known about quality in dentistry and how does quality in dentistry differ from other healthcare services?
There is a traditional, poorly articulated notion that quality in dentistry is exemplified by complex, expensive care with a significant cosmetic component for example, crown and bridgework or implant-retained prostheses. This perception was reinforced when the House of Commons select committee29 raised concerns about the quality of care delivered as a result in the drop in the number of complex courses of treatment following introduction of the 2006 NHS contract.30 This simplistic view of quality reflects the underdeveloped academic literature on the subject in dentistry.
There is no agreed definition of quality in dentistry22,31 although this hasn't prevented measures of different aspects being developed and used.32,33,34 These measures have largely focused on clinical aspects of care, but have also drawn on some of the work undertaken in the wider medical literature; naturally primary medical care is seen as the most comparable field to primary dental care. However, dentistry differs from primary medical care in a number of specific and significant ways, which will influence the views of stakeholder groups on how quality in dentistry is perceived.
In general medical practice a large proportion of patients seek care sporadically as a result of experiencing symptoms, and in dentistry a majority of patients attend asymptomatically and on a regular basis. Continuity of care is therefore important as well as customer satisfaction to encourage repeat attendance.
Dentistry is primarily a surgical discipline, whereas general (medical) practitioners (GPs) are predominately diagnosticians, coordinators of care for long-term conditions and gatekeepers to specialist care. This has consequences; dental care is frequently associated with pain and anxiety in popular consciousness and therefore how pain and anxiety are managed will have a significant influence on patients' views of the quality of care provided.
Dentistry is predominantly concerned with just two diseases, whereas general medical practice is confronted with a much wider range of physical and psychological conditions and often multiple co-morbidities. Also many of the diseases general medical practice is concerned with are potentially more serious in nature. Misdiagnosis, poor patient management and clinical errors can therefore have serious or even fatal consequences. Therefore, patient safety has a comparatively greater significance within the overarching concept of quality in medical practice than in dental practice.
In the UK, care provided by general medical practices is free at the point of delivery whereas primary dental care, whether in the public or private sector, levies significant charges that are directly linked to the care provided. The clinician as part of the informed consent process engages in a discussion with the patient not only about clinical care but also about treatment charges and this produces a different dynamic between patient and dentist than between patient and GP.
Many of the treatments provided by general dental practitioners (GDPs), especially in the private sector, are primarily cosmetic in nature and secondarily associated with treatment of disease, whereas GPs have a prime focus on treatment and management of disease. This difference in emphasis again changes the relationship between clinician and patient, with the dental patient more likely to adopt attitudes associated with a customer rather than a patient.
In the NHS the way GPs and GDPs are paid is also very different. Like dentists, NHS funding of GPs is largely practice-based. Medical practices receive weighted capitation payments, which generally make up about half of their funding. In addition they receive payments for providing evidence-based care primarily for patients with chronic conditions such as hypertension and diabetes through the Quality Outcomes Framework. They receive additional funding for providing optional enhanced services. Critically they receive premises payments, which vary according to the value of the premises as determined by the district valuer; their information technology costs are also covered by the local NHS. Contrast this with the way English GDP practices are currently remunerated, in which all costs (staff, premises and consumables) are met from 12 fixed monthly payments dependent on hitting activity targets. Remuneration arrangements have an important influence on quality and are critically important if quality improvement is to be incentivised.35,36
Skill mix is more widely developed and used in general medical practice compared to general dental practice. There have been recent calls to expand skill mix and the GDC has recently removed its barrier to direct access to some dental care professionals (DCPs).37 We have little understanding of the impact of such developments on the various domains of quality.
Although these differences will perhaps not change the relevance of the fundamental domains of quality to dentistry, they will influence the relative importance of each domain as viewed by the different stakeholder groups. It is therefore important that dentistry does not just 'lift and shift' the approach to quality developed by primary medical care, rather something bespoke and fit for purpose is required.
The Steele review38 advocated a standardised assessment of patients; categorisation of their disease risk and the care they receive delivered according to evidence-based care pathways. This approach to care is currently being piloted. In such a system can personalised individual care be maintained as a key component of quality or will a more prescribed, biomedical approach to treatment of standardised problems result in more effective care and improved quality? Will a new capitation-based remuneration system deliver equitable access and value for money? Policy makers will need to weigh up the relative merits of these potentially competing attributes to shape a service that is focused on quality.
Policy perspective
Following the Darzi39 report of the last government, which called for quality to be a key organising principle of the NHS, the current government's NHS white paper40 seeks to promote a patient-focused, clinically-led, outcomes-driven NHS. The NHS constitution41 published by the previous government and supported and updated by the current government lists as one of its seven guiding principles; 'The NHS aspires to the highest standards of excellence and professionalism – in the provision of high-quality care that is safe, effective and focused on patient experience'. So quality is not going to go away and will touch every service provided by the NHS and by extension patient expectations will rise and have an impact on care provided in the private sector. In England the first steps have been taken to incentivise quality in the pilots for a new dental contract and the development of a Dental Quality Outcomes Framework (DQOF).34 The DQOF is a start to the process of incentivising quality, we don't know if it reflects all of the important elements of quality or, importantly, if the indicators included are valid and reliable measures of quality. It will need to be refined through rigorous academic input. It is well accepted that policy and research move at different paces and there has been pressure to rapidly produce quality outcome measures for dentistry for the new contract pilots. However, this does not preclude the commissioning high quality research to inform the evolution of the DQOF to provide confidence to all stakeholders that it actually does what is expected of it.
Developing a framework for defining quality for dentistry
The general practice QOF was first produced and introduced in 2004.42 In some ways dentistry is currently in a similar position to primary medical care at that time. However, the GP QOF has since been refined and validated through a high quality, rigorous research and testing programme.8 Dentistry must follow the same approach from the start; this issue is too fundamental and too important to be based on opinion, anecdote and expedience. A conceptual model for quality in dentistry needs to be built based on the dental literature and drawing on the wider healthcare literature. No doubt domains such as service organisation, including access, clinical effectiveness, patient safety and patient experience will be included but we need to start with principles and supplement the review literature by collecting empirical data to fill in the considerable gaps. Only when we have this strong theoretical base with a well-defined typology specific to dentistry will we be in a position to develop valid measuring instruments.
Conclusions
Caper suggested that efforts to define the term 'quality' should be abandoned in favour of the identification and measurement of its components.43 However, without an agreed conceptual framework underpinning these components they lack value and a link to stakeholder experiences and therefore their credibility can be questioned. Moreover, without a clear understanding of quality, how to measure it and improve it, there is a risk that dental services will not provide value and fail to improve quality.
References
Greenhalgh T . Primary health care: theory and practice. Oxford: Blackwell Publishing, 2007.
Campbell S M, Roland M O, Buetow S A . Defining quality of care. Soc Sci Med 2000; 51: 1611–1625.
Raleigh V S, Foot C . Getting the measure of quality: opportunities and challenges. London: King's Fund, 2010.
Heath I, Rubinstein A, Stange K C, van Driel M L . Quality in primary health care: a multidimensional approach to complexity. BMJ 2009; 338: b1242.
Donabedian A . Explorations in quality assessment and monitoring: Volume 3. The methods and findings of quality assessment and monitoring. Michigan: Health Administration Press, Ann Arbor, 1985.
Donabedian A . Explorations in quality assessment and monitoring: Volume 1. The definition of quality and approaches to its assessment. Michigan: Health Administration Press, Ann Arbor, 1980.
Blumenthal D . Quality of care- what is it? N Engl J Med 1996; 335: 891–894.
Campbell S M, Kontopantelis E, Hannon K L, Barber A, Burke M, Lester H E . Framework and indicator testing protocol for developing and piloting quality indicators for the UK Quality and Outcomes Framework. BMC Fam Pract 2011; 12: 85.
World Health Organization. Primary health care: report of the International Conference on Primary Health Care, Alma-Ata USSR., 6–12 September, 1978. Geneva: WHO, 1978.
Starfield B, Shi L, Macinko J . Contribution of primary care to health systems and health. Milbank Q 2005, 83: 457–502.
Starfield B . Is primary care essential? Lancet 1994; 344: 1129–1133.
Graff L, Stevens C, Spaite D, Footy J . Measuring and improving quality in emergency medicine. Acad Emerg Med 2002; 9: 1091–1107.
Donabedian A . Evaluating the quality of medical care. Millbank Mem Fund 1966; 44: 166–206.
Maxwell R J . Quality assessment in health. Br Med J (Clin Res Ed) 1984; 288: 1470–1472.
Donabedian A . An introduction to quality assurance in health care. Oxford: Oxford University Press, 2003.
Steffen G E . Quality medical care. A definition. JAMA 1988; 260: 56–61.
Lohr K . Medicare. A strategy for quality assurance. Washington D.C: National Academy Press, 1990.
Institute of Medicine. Crossing the quality chasm. A new health system for the 20th century. Washington, D C: National Academy of Sciences, 2003.
Cheraghi-Sohi S, Hole A R, Mead N et al. What patients want from primary care consultations: a discrete choice experiment to identify patients' priorities. Ann Fam Med 2008; 6: 107–115.
Baker R, Boulton M, Windridge K, Tarrant C, Bankart J, Freeman G . Interpersonal continuity of care: a cross sectional survey of patients' preferences and their experiences. Br J Gen Pract 2007; 57: 283–290.
Cheraghi-Sohi S, Bower P, Mead N, McDonald R, Whalley D, Roland M . Making sense of patient priorities: applying discrete choice methods in primary care using 'think aloud' technique. Fam Pract 2007; 24: 276–282.
Mills I, Batchelor P . Quality indicators: the rationale behind their use in NHS dentistry. Br Dent J 2011; 211: 11–15.
Palmer H R, Donabedian A, Povar G J . Striving for quality in health care. An inquiry into policy and practice. Michigan: Ann Arbor, 1991.
Sutton M . Vertical and horizontal aspects of socio-economic inequity in general practitioner contacts in Scotland. Health Econ 2002; 11: 537–549.
Campbell S M, Eriksson T . Multiple strategies for quality improvement and patient safety- money alone is not the answer, nor is trust. Eur J Gen Pract 2011; 17: 238–240.
Checkland K, Marshall M, Harrison S . Re-thinking accountability: trust versus confidence in medical practice. Qual Saf Health Care 2004; 13: 130–135.
Heath I, Hippisley-Cox J, Smeeth L . Measuring performance and missing the point? BMJ 2007; 335: 1075–1076.
Heath I . Divided we fail. The Harveian oration 2011. London: Royal College of Physicians, 2011. Online lecture available at http://www.rcplondon.ac.uk/sites/default/files/harveian-oration-2011-web-navigable.pdf (accessed June 2013).
House of Commons Health Committee. Dental services - fifth report of session 2007–08. London: The Stationery Office Limited, 2008. Online report available at http://www.parliament.the-stationery-office.com/pa/cm200708/cmselect/cmhealth/289/289i.pdf (accessed June 2013).
Tickle M, McDonald R, Franklin J, Aggarwal V R, Milsom K . Reeves D. Paying for the wrong kind of performance? Financial incentives and behaviour changes in NHS dentistry 1992–2009. Community Dent Oral Epidemiol 2011; 39: 465–473.
European Regional Organisation of the Fédération Dentaire Internationale. ERO-FDI WG Quality in Dentistry Report 2007–2010. Online report available at http://www.erodental.org/ddc/ddid97 (accessed 04/10/12).
Ireland R S, Jenner A M, Williams M J, Tickle M . A clinical minimum data set for primary dental care. Br Dent J 2001; 190: 663–667.
Dental Quality Alliance. Quality measurement in dentistry: a guidebook. Chicago: American Dental Association, 2012.
Department of Health. Dental quality and outcomes framework. London: DH, 2011. Online article available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/ file/152039/dh_126627.pdf.pdf (accessed June 2013).
Scott A, Sivey P, Ait Ouakrim D et al. The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database Syst Rev 2011; CD008451.
McDonald R, Roland M . Pay for performance in primary care in England and California: comparison of unintended consequences. Ann Fam Med 2009; 7: 121–127.
General Dental Council. Patient safety at the heart of decision over Direct Access. London: GDC, 2013. Online press release available at http://www.gdc-uk.org/newsandpublications/pressreleases/pages/patient-safety-at-the-heart-of-decision-over-direct-access.aspx (accessed June 2013).
Steele J, Clarke J, Rooney E, Wilson T . NHS dental services in England: An independent review. London: HSMO, 2009.
Professor the Lord Darzi of Denham KBE. High quality care for all. NHS next stage review final report. London: HSMO, 2008.
Department of Health. Equity and excellence: liberating the NHS. London: Crown Copyright, 2010. Online article available at https://www.gov.uk/government/publications/liberating-the-nhs-white-paper (accessed June 2013).
Department of Health. The NHS Constitution for England. London: HMSO, 2013. Online constitution available at https://www.gov.uk/government/publications/the-nhs-constitution-for-england (accessed June 2013).
Roland M . Linking physicians' pay to quality of care — a major experiment in the United Kingdom. N Engl J Med 2004; 351: 1448–1454.
Caper P . Defining quality in medical care. Health Aff (Millwood) 1988; 7: 49–61.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Campbell, S., Tickle, M. What is quality primary dental care?. Br Dent J 215, 135–139 (2013). https://doi.org/10.1038/sj.bdj.2013.740
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.740
This article is cited by
-
Global, regional, and national burden and quality of care index (QCI) of oral disorders: a systematic analysis of the global burden of disease study 1990–2017
BMC Oral Health (2024)
-
A RAND/UCLA appropriateness method study to identify the dimensions of quality in primary dental care and quality measurement indicators
British Dental Journal (2020)
-
Conceptualising a framework for improving quality in primary dental care
British Dental Journal (2019)
-
Clinical and academic recommendations for primary dental care prosthodontics
British Dental Journal (2019)
-
Education and training in craft skills dentistry
British Dental Journal (2019)