Key Points
-
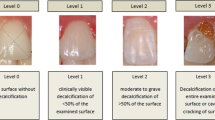
Idiopathic enamel hypomineralisation (IEH), also known as molar incisors hypomineralisation (MIH) is a condition of unknown aetiology in which enamel defects are seen in one or more first permanent molars usually with one or more incisors affected.
-
Laboratory studies were carried out on 2 affected and 2 apparently normal first permanent molars extracted from the same patient with IEH.
-
Hypomineralised enamel was randomly distributed throughout the crowns of the affected teeth with a mineral concentration up to 20% lower than normal and a gradient form ADJ to surface reverse that of normal enamel.
-
Post-eruptive breakdown of hypomineralised enamel did not occur in the fissure sealed tooth.
Abstract
Objective To measure mineral concentration distributions within teeth with idiopathic enamel hypomineralisation, a condition in which developmental defects are seen in first permanent molars, and/or incisors.
Design X-ray microtomographic and 3D x-ray microscopy.
Setting UK University, 2001.
Materials and methods X-ray microtomographic measurements of the extent of hypomineralisation in two affected molars and two contralateral controls extracted from the same patient.
Results The control molars were visibly normal. The affected molars showed hypomineralised yellow opaque enamel with regions of breakdown. X-ray microtomographic images showed; a 20% reduction in mineral concentration of affected enamel (most cases involved full enamel thickness); hypomineralised enamel had a mineral concentration gradient opposite to that of normal enamel; regions of hypomineralisation distributed randomly throughout affected teeth, (apart from cervical region which was less severely affected).
Conclusions The pattern of mineral concentration suggests a disturbance during the maturation process. Differences in susceptibility of the ameloblasts during different stages of dental development may explain the asymmetric distribution of the defects. Topical fluoride applications may help promote post eruption maturation of the surface layer in these teeth. The use of fissure sealants and adhesive materials appears to prevent further breakdown.
Similar content being viewed by others
Main
Developmental defects of enamel may be classified as either hypoplasia or hypomineralisation. Hypoplasia occurs as a result of a disturbance to the ameloblasts during matrix secretion. This may appear clinically as pits, grooves or areas of missing enamel. Hypomineralisation occurs once the full thickness of enamel matrix is laid down, either as a result of a disturbance during initial calcification or during maturation. In some cases both exist together and it may be difficult to distinguish between true hypoplasia and posteruptive breakdown of hypomineralised enamel.
The common causes of enamel defects include: inherited (as in amelogenesis imperfecta1); excess fluoride intake2; and a systemic upset during amelogenesis.2,3 However, in some cases, the aetiology is unknown and the condition is termed 'idiopathic enamel hypoplasia (IEH)'. IEH usually manifests as hypomineralisation or hypoplasia of one or more permanent molars with or without opacities of one or more permanent incisors. The term molar-incisor hypomineralisation (MIH) is preferred by some authors.4
IEH was first reported in Sweden in the late seventies with a peak incidence in children born in 1970 (reviewed in Koch et al.5). More recently, Jalevik et al.6 reported that 15% of Swedish children had this condition, and Leppaniemi et al.7 reported that 19% of Finnish children were affected. Although the distribution of the defect suggests a chronological disturbance during the first few years of childhood, in most cases there is no obvious medical history to support this. Beentjes et al.4 suggested that affected children may have suffered more episodes of illnesses such as otitis media or high fever, but more research is needed to confirm this.
Child patients with IEH provide a challenge for both the clinician and the scientist. The teeth are often very sensitive and may show rapid breakdown. In some cases early extraction of these teeth is the treatment of choice.
Little is known of the microscopic structure of teeth with developmental defects. Microscopic studies of teeth from the hypoplastic type of amelogenesis imperfecta and the hypomineralised types have shown that both hypomineralisation and hypoplasia often occurred simultaneously.8 Fearne et al.9 showed that some primary teeth with chronological hypoplasia extracted from children with neonatal illness have reduced mineral concentrations of up to 10%.
Suga10 described four types of hypomineralisation and related them to the developmental stages of the ameloblasts listed below:
Type 1: Hypomineralisation associated with hypoplasia (ie reduced amount of enamel matrix). Ameloblasts damaged during matrix secretion but cannot recover maturation potential.
Type 2: Slight hypomineralisation in the matrix in the interior layer. Disturbance of matrix degredation process.
Type 3: Hypomineralisation of entire width except innermost layer. Disturbance during early maturation (transitional stage).
Type 4: Hypomineralisation mainly in the outer layer. Damage during middle or late stage of maturation.
It was proposed that the most vulnerable cell is the transitional ameloblast as it changes from a secretory ameloblast to a maturation ameloblast. These cells may not recover full maturation potential, leading to full thickness hypomineralisation. However, less vulnerable cells affected at an earlier or later stage may recover some maturation properties leading to further mineralisation in certain regions.
The aim of this study was to measure the extent and the distribution of mineral concentration in four first permanent molars which had been extracted from a child with IEH/MIH. This was carried out using x-ray microtomography (XMT), a non-destructive x-ray absorption microscopic technique for 3-D visualisation of specimens, as well as direct quantitative linear and densitometric measurements within the images.
Materials and methods
Four first permanent molars were extracted from a 9-year-old girl as part of an orthodontic treatment plan. The teeth were stored in plastic containers containing tap water prior to imaging. Detailed descriptions of all four teeth studied are shown in Table 1.
X-ray microtomography (XMT) is a miniaturised version of the well-known technique of whole body scanning which is now being used extensively in hard tissue dental research (examples have appeared in this journal11,12). Transmission x-ray images of the specimen are recorded using a scintillation screen coupled to a CCD camera. Images are repeatedly taken as the specimen is rotated through 360 degrees (1,201 in total). The response of the transmitted X-ray image capture system is precalibrated with a 10-step aluminium step wedge. The data are collected whilst the specimen is immersed in fluid, so there are no drying artefacts. The time taken for data collection of the molars used in this study was 18 h. The data were then reconstructed and processed for quantification as previously described.13
During data collection, each tooth was located inside a plastic syringe and kept firmly in place by depressing the syringe plunger lightly in contact with the top of the tooth in order to prevent motion of the specimen. The syringe tube was filled with deionised water and then mounted onto the rotation axis of the XMT stage. XMT images were taken of all the specimens. Typical size of the raw data sets was 2.5 Gbytes. After reconstruction, the image dataset was 0.5 Gbyte. The image datasets were visualised and analysed using Amira 2.3 (TGS Inc. San Diego, Ca).
In this study, 3D data sets of mineral concentration values within the whole uncut tooth specimens were obtained at a resolution of 15.221 μm. Image slice data, cut at orientations selected by the user can be obtained of sections 1 voxel thick (thickness 15.221 μm) which appear similar to contact microradiographs. These XMT sections are maps of mineral concentrations values at each voxel in the image. Mineral concentration profiles along selected lines can then be obtained from these sections. Other mathematical operations can be performed on the 3D image datasets, for example, surface rendering, in which all adjacent voxels with the same mineral concentration are joined by a surface. Surface rendered images can be 'rotated' for viewing using computer display and visualisation packages.
Results
Study tooth
Colour photographs and a surface rendered XMT image of the study tooth are shown in Figure 1. The similarity of the XMT image (d) to the photograph (b) is readily apparent.
A pseudo-colour XMT section (axially cut) through the mid-crown region of the study tooth is shown in Fig. 2a. This shows areas of lower mineral concentration in all but the mesial region. In the most severely affected regions, as along line CD, there is lower mineral concentration across the full thickness of the enamel, but in other regions, only the innermost enamel is affected (E). Mineral concentration line profiles through the apparently normal enamel in the mesial region (line AB) and through a hypomoineralised region (line CD) are shown in Figure 2b. These show reduced mineral concentration of up to 20% in the enamel region along line CD compared with the apparently normal enamel along line AB. Also, there is a demonstrable gradient in the mineral concentration in the hypomineralised region from ∼2.3 g cm−3 at the ADJ, reducing to ∼1.9 g cm−3 in the subsurface enamel, but with a more mineralised surface layer (although the surface enamel is still not quite as mineralised as the apparently normal enamel). Note the direction of the gradient is reversed compared with that seen in normal enamel which increases from the ADJ to the surface.14 There was no difference in the mineral concentration of the dentine underlying affected enamel compared with that underlying the apparently normal enamel.
The colour scale shows values of mineral concentration in g cm-3. The image was scaled to show mineral concentrations within the values shown in order to highlight the hypomineralised enamel. (b) Mineral concentration profiles along lines AB and CD shown in Fig. 2a. (c) Grey-scale XMT sagittal section of study tooth
Figure 2c is a grey-level XMT section taken in the sagittal plane which shows that the hypomineralised enamel extends throughout most of the crown except for the cervical region.
Control tooth
Figure 3a is a pseudo-colour XMT axial section taken through the control tooth which showed no obvious hypomineralised enamel. The line profiles ab and cd show a gradient in mineral content increasing from the ADJ towards the surface (Fig. 3b) as expected. Figure 3c is a grey-scale XMT section in the sagittal plane of the control tooth which shows reduced mineral concentration in the fissures, probably associated with carious fissure lesions.
Colour scale shows mineral concentration in g cm−3. The image was scaled to show mineral concentrations within the values shown in order to highlight the hypomineralised enamel. (b) Mineral concentration profiles along lines ab and cd shown in Fig. 3a. (c) Grey-scale XMT sagittal section of control tooth.
Fissure sealed tooth
Figure 4 is a montage of a sagittal and an axial grey-level XMT section through a fissure sealed tooth showing hypomineralised enamel similar to that seen in the study tooth. However, there was no indication of the breakdown of the enamel seen in the study tooth, nor any indication of fissure caries.
Amalgam tooth four
The amalgam restoration was so highly x-ray absorbent that no meaningful information could be obtained.
Discussion
Visual inspection revealed that not all four molars were equally affected, as even within the same tooth there were regions of affected and apparently normal enamel. Where clinically opaque enamel was seen, this seemed to affect all levels of the crown of the tooth but with the cervical region being less susceptible.
The XMT images provided information on the distribution of mineral concentration throughout the crowns of the clinically affected and the apparently normal teeth from the same child with idiopathic enamel hypomineralisation.
There did not appear to be Type 1 hypomineralisation defects. This suggests that the disturbances may occur after the initial stage of enamel formation. Most defects were Type 3 affecting the full thickness of the enamel, but some Type 2 defects affecting only the innermost enamel were also seen.
The apparently random nature of the distribution of hypomineralisation throughout the four teeth and the large amount of the tooth crown involved is difficult to explain considering they develop during the same period. One could speculate that generally growth and development is not completely symmetrical or uniform. Small differences in development within these teeth may affect cells at critical stages.
The findings from this study suggest that the disturbance may be of a more chronic nature over a longer period of time. Differences in the susceptibility of the ameloblasts at different stages of their developmental cycle may explain the random distribution of the defects. Those ameloblasts in the transitional phase are the most susceptible.
The high to low mineral concentration gradient from the ADJ to the subsurface enamel in full thickness defects is opposite to that seen in normal enamel. This suggests that the second phase of maturation is progressively more disturbed.
The more mineralised surface layer can probably be explained by post-eruption maturation.
The XMT images showed that the mineral concentrations in the control tooth were similar to those measured in other XMT studies using the same equipment.15 However, an overall reduction of about 5% was measured in the mineral concentrations of both the apparently normal enamel and dentine within the study tooth compared with those in the control tooth. This suggests that in fact the whole IEH tooth is affected to some extent.
From a clinical perspective, topical fluoride applications may be helpful to encourage further post-eruptive maturation. Further, the obvious protection against breakdown and fissure caries resulting from the use of fissure sealants would suggest that this treatment may be helpful in these cases.
References
Sundell S, Koch G . Hereditary amelogenesis imperfecta 1: epidemiology and clinical classification in a Swedish child population. Swed Dent J 1985; 9: 157–169.
Pindborg JJ . Aetiology of developmental enamel defects not related to fluorosis. Int Dent J 1982; 32: 123–134.
Brook AH, Fearne JM, Smith JM . Dental enamel: environmental causes of enamel defects. In Chadwick D, Cardew G. (eds) Dent Enamel. Chichester: Wiley, 1997. pp 212–223.
Beentjes VEVM, Weerheijm KL, Groen HJ . Factors involved in the aetiology of molar-incisor hypomineralisation(MIH). Eur J Paediatr Dent 2002; 3: 9–13.
Koch G, Hallonsten AL, Ludvigsson N, Hansson BO, Holst A, Ulbro C . Epidemiological study of idiopathic enamel hypomineralisation in permanent teeth of Swedish children. Community Dent Oral Epidemiol 1987; 15: 279–285.
Jalevik B, Noren JG . Enamel hypomineralisation of permanent first molars. A morphological study and survey of possible etiological factors. Int J Paed Dent 2000; 10: 278–289
Leppaniemi A, Lukinmaa PL, Alaluusua S . Nonfluoride hypomineralizations in first permanent molars and their impact on the treatment need. Caries Res 2001; 35: 36–40.
Backman B, Anneroth G . Microradiographic study of amelogenesis imperfecta. Scand J Dent 1989; 97: 316–329.
Fearne JM, Elliott JC, Wong FSL, Davis GR, Boyde A, Jones SJ . Deciduous enamel defects in low birthweight children: correlated x-ray microtomographic and backscattered electron imaging study of hypoplasia and hypomineralisation. Anat Embryol 1994; 189: 375–381.
Suga S . Enamel hypomineralisation viewed from the pattern of progressive mineralization of human and monkey developing enamel. Adv Dent Res 1989; 3: 188–198.
Mercer CE, Anderson P . X-ray microtomography: a novel technique for the quantification of effects in enamel following CO2 laser application. Br Dent J 1996; 180: 451–455.
Mercer CE, Anderson P, Davis GR . Sequential 3D X-ray microtomographic measurement of enamel and dentine ablation by an Er:YAG laser. Br Dent J 2003; 194: 99–104.
Davis GR, Elliott JC . X-ray microtomography scanner using time-delay integration for elimination of ring artefacts in the reconstructed image. Nucl Instr Meth Phys Res 1997; 394: 157–162.
Anderson P, Elliott JC, Bose U, Jones SJ . A comparison of the mineral content of enamel and dentine in human premolars and enamel pearls measured by X-ray microtomography. Archs oral Biol 1996; 41: 281–290.
Dowker SEP, Elliott JC, Davis GR, Wassif HS . Longitudinal study of the three-dimensional development of subsurface lesions during in vitro demineralisation. Caries Res 2003; 37: 237–245.
Acknowledgements
This work was supported in part by EPSRC grant no. GR/R28911/01.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Fearne, J., Anderson, P. & Davis, G. 3D X-ray microscopic study of the extent of variations in enamel density in first permanent molars with idiopathic enamel hypomineralisation. Br Dent J 196, 634–638 (2004). https://doi.org/10.1038/sj.bdj.4811282
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4811282
This article is cited by
-
Is there a rise of prevalence for Molar Incisor Hypomineralization? A meta-analysis of published data
BMC Oral Health (2024)
-
Clinical evaluation of resin infiltration treatment masking effect on hypomineralised enamel surfaces
BMC Oral Health (2023)
-
An evaluation of remineralised MIH using CPP-ACP and fluoride varnish: An in-situ and in-vitro study
European Archives of Paediatric Dentistry (2022)
-
Effects of different remineralization agents on MIH defects: a randomized clinical study
Clinical Oral Investigations (2022)
-
Label-free quantitative proteomics reveals molecular correlates of altered biomechanical properties in molar incisor hypomineralization (MIH): an in vitro study
European Archives of Paediatric Dentistry (2022)