Abstract
This study was undertaken to examine the interaction between the combination of angiogenesis and blood vessel invasion (BVI) and haematogenous metastasis, and to determine the prognostic significance of that combination in predicting 20-year relapse-free survival (RFS) and overall survival (OS) rates in primary breast cancer. Five hundred and nine patients were studied. We investigated 11 factors, including average microvessel count (AMC)/BVI, lymph-node status (n), clinical tumour size (T), histological grade (HG), lymphatic vessel invasion (LVI), p53, proliferating cell nuclear antigen (PCNA), c-erbB-2, mitotic index (MI), apoptotic index, and tumour necrosis (TN). Blood vessel invasion was detected by both factor VIII-related antigen and elastica van Gieson staining. To evaluate the best objective method to quantify microvessel density in angiogenesis, AMC was employed. The rate of AMC-high and BVI-positive tumours was 32.6 and 29.3%, respectively. That of both AMC-high and BVI-positive tumours was 10.1%. Univariate analysis showed that AMC/BVI, n, T, HG, LVI, p53, PCNA, MI, and TN were significantly predictive of RFS and OS. By multivariate analysis, AMC/BVI was the strongest independent prognostic factor for 20-year RFS (relative risk (RR)=5.5; P<0.0001) and for 20-year OS (RR=4.3; P<0.0001). Lymph-node status was still considered a powerful prognostic indicator; however, the combination of AMC and BVI provided more reliable prognostic information than lymph-node status for haematogenous dissemination.
Similar content being viewed by others
Main
There have been many reports about the prognostic factors in breast cancer of which lymph-node status remains a major conventional prognostic factor and has been clinically used as a measure for disseminating the disease, while some investigators have reported that lymph-node metastases have not necessarily been associated with haematogenous dissemination (Fisher et al, 1981; Menard et al, 1994; Braun et al, 2000). Moreover, several additional biologic markers, such as angiogenesis, p53, proliferating cell nuclear antigen (PCNA), c-erbB-2, apoptosis, mitosis, and necrosis have been related to tumour proliferation and development, but their effects on tumour haematogenous metastasis are by no means clear, and there are still controversies regarding the best possible prognostic index for breast cancer patients (Thor et al, 1992; Gilchrist et al, 1993; Zhang et al, 1998; Kato et al, 1999; Beenken et al, 2001; Sirvent et al, 2001).
Some studies have suggested that microvessel density indicated representative angiogenesis of the tumour and was an independent and highly significant prognostic factor for both node-negative and node-positive patients (Weidner et al, 1991; Gasparini et al, 1994; Simpson et al, 1996; Heimann et al, 1996; Kato et al, 2001). However, other authors reported that angiogenesis did not predict recurrence in patients with primary breast cancer (Van Hoef et al, 1993; Goulding et al, 1995). The significance of angiogenesis remains controversial because of studies that varied in patient selection, length of time of patient follow-up, antibody used to detect endothelial cells, sample size, method of counting microvessels, and the patients' race.
Recent reports have suggested that peritumour lymphatic and blood vessel invasion (BVI) (vascular invasion) (Lee et al, 1990; Mansi et al, 1991; Fox et al, 1997) or peritumour lymphatic vessel invasion (LVI) (Clemente et al, 1992; Gasparini et al, 1994; Lauria et al, 1996) are significant prognostic factors. However, there are a few recent studies of the prognostic significance of peritumour BVI (Gasparini et al, 1994; Lauria et al, 1996; Kato et al, 2000, 2002). It has been more difficult to identify invasion of small vessels and capillaries and in the larger vessels surrounded by elastic tissue in breast cancer in routine haematoxylin and eosin (H&E)-stained tissue sections than in gastric or colorectal cancer. A wide range of frequencies has been reported for BVI among patients with breast cancer and the prognostic significance of BVI has not yet been made clear (Weigand et al, 1982; van de Velde et al, 1986; Gasparini et al, 1994; Lauria et al, 1996; Kato et al, 2000, 2002).
Tumours that have acquired the ability of high neovascularisation are likely to involve blood vessels. However, all tumours with high neovascularisation do not have the ability to invade vessels. Gould et al (1983) reported that bronchial carcinoid tumours are highly vascular, but they do not spread beyond the lung. Angiogenesis is necessary for a tumour to grow but not sufficient for it to metastasise. Thus, there are definitely biological differences between the ability of tumours to form high neovascularisation and their ability to invade blood vessels. And both the growth of tumours dependent on angiogenesis and the tumours spreading beyond the primary site are dependent on access to the vasculature and are important for haematogenous metastasis.
This study was undertaken to examine the interaction between the combination of angiogenesis and BVI and haematogenous dissemination, and to determine the absolute and relative values of that combination using both Factor VIII-related antigen and elastica van Gieson staining, as we detected by our method published previously (Kato et al, 2001, 2002). Moreover, the clinicopathological significance of p53, PCNA, c-erbB-2, and apoptosis, relatively new prognostic factors, and conventional prognostic factors, especially lymph-node status was evaluated in predicting relapse-free survival (RFS) and overall survival (OS) rates with a long-term follow-up in Japanese patients with breast cancer.
Patients and methods
Patients
Data for this study were collected from 509 breast cancer patients selected from those operated on between 1971 and 1990 at Tokyo Women's Medical University Hospital for whom we had sufficient clinical and pathologic material to determine all the biological markers. The distribution of the main clinicopathologic data for the entire 509-patient population is given in Table 1. Two hundred and sixty-four of these patients (51.9%) were treated with radical mastectomy, 153 patients (30.0%) with modified radical mastectomy, and 92 patients (18.1%) with extended radical mastectomy. Although we had no formal protocol for adjuvant therapy, adjuvant chemotherapy was administered to patients with T2, T3 or lymph-node positive tumours. Two hundred and ninety-two of those patients (57.3%) received adjuvant chemotherapy including mitomycin C (given intravenously after mastectomy; total doses ranged from 20 to 40 mg for 4–6 weeks) and/or 5-fluorouracil (or its derivatives) were taken orally for 5 years. Postmenopausal patients with positive oestrogen receptors were treated with adjuvant hormone therapy from 1983. Ninety-eight patients (19.3%) received adjuvant chemotherapy and hormone therapy, and 25 patients (4.9%) received adjuvant hormone therapy. No adjuvant treatment was given to 94 patients (18.5%). The median follow-up duration of the patients was 9 years (range, 1–20).
Pathological studies
The original histologic sections of biopsy and mastectomy specimens were reviewed. Paraffin-embedded tissue samples of 4.5 μm thick sections stained with H&E were histopathologically assessed. The pathologic specimens were reviewed without any knowledge of the eventual clinical outcome. Conventional clinicopathologic features were observed and recorded, including the clinical tumour size, histological grade, LVI, and tumour necrosis (TN). The clinical tumour size was determined based on the TNM classification, the histological grade was decided based on the Bloom–Richardson grade (Bloom and Richardson, 1957), and LVI was determined based on H&E staining. Sections of the breast tumour that were stained with H&E were used to select the maximal area of all the cut surfaces of the tumour that included the invasive component.
Apoptotic cells were assessed in (H&E) stained sections. The apoptotic cells were defined as cells showing marked condensation of chromatin and cytoplasm, cytoplasmic fragments containing condensed chromatin, and intra- and extracellular chromatin fragments with a diameter of approximately 2 μm (Wyllie et al, 1981). Apoptotic cells were counted using a standard light microscope at a 400 magnification (× 40 objective, 0.152 mm2 per field) in 10 randomised fields. Apoptotic index (AI) was scored as negative (<10 apoptotic cells per 10 fields) and positive (⩾10 apoptotic cells per 10 fields). The mitotic index (MI) was determined by a method described in a previous report (Baak et al, 1985). The nuclear membrane and the clear zone in the centre had to be absent, and clear, hairy extensions of nuclear material had to be present for them to be counted. Two parallels, and each of the two clearly separate chromosome clumps, were both counted as two mitotic figures. The number of mitotic figures was identified in 10 high-power microscopic fields (objective magnification × 40). The MI were scored as negative (<10 mitotic figures per 10 fields) and positive (⩾10 mitotic figures per 10 fields). The necrosis was divided into two categories. Coagulation necrosis in the centre area of cancer nests was defined as central necrosis, and necrosis in the intraductal component was defined as comedo necrosis (Kato et al, 1997).
Immunohistochemical determinations
Immunostains for PCNA, p53, c-erbB-2, and factor VIII-related antigen were performed on the paraffin sections using the streptavidin–biotin–immunoperoxidase method as previously described (Kato et al, 1999). Briefly, the primary antibodies employed were an affinity-purified monoclonal anti-human-PCNA antibody (PC10, Novocastra Laboratories, Newcastle, UK) at a 1 : 100 dilution, polyclonal anti-p53 antibody (CM1, Novocastra Laboratories, UK) diluted at a 1 : 100, polyclonal anti-human c-erbB-2 protein antibody (Dako, Copenhagen, Denmark) at a 1 : 100 dilution, and monoclonal antibody (von Willebrand factor F8/86, Dako, Copenhagen, Denmark) applied at 1 : 200. After immunostaining, the sections were counterstained with haematoxylin. The growth fraction by PCNA staining was evaluated by counting 500 consecutive cells on one slide for each tumour with a × 400 magnification and an index of positive cells to the total number of cells (labeling index (LI)) was made. Labelling index was evaluated and scored as negative (
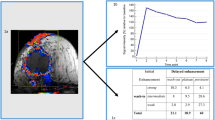
Representative examples of BVI and LVI. (1) Blood vessels directly infiltrated by cancer cells (Type I, A: factor VIII-related antigen staining, haematoxylin counter stain, original magnification: × 100). (2) Blood vessels filled with tumour cell emboli and lymphatic vessel invasion (Type II, B: H&E staining, C: elastica van Gieson staining, D: factor VIII-related antigen staining, haematoxylin counter stain, original magnification: B–D × 50). The arrowhead indicates a BVI and arrows indicate LVI with floating tumour cells. The endothelium of lymphatic vessels by factor VIII-related antigen staining was not stained. (3) Blood vessels with growth of cancer cells between endothelium and lamina elastica interna (Type III, E: H&E staining, F: elastica van Gieson staining, G: factor VIII-related antigen staining, haematoxylin counter stain, original magnification: E–G × 50). (4) Blood vessels with floating tumour cells (Type IV, H: factor VIII-related antigen staining, haematoxylin counter stain, original magnification: × 200). (5) The arrowhead indicates a lymphatic vessel with floating tumour cells and arrows indicate blood vessels. The pattern of staining in the lymphatic vessel by factor VIII-related antigen staining was very faint, discontinuous, and inconsistent in contrast to the intense and continuous staining observed in the vascular endothelium (I: factor VIII-related antigen staining, haematoxylin counter stain, original magnification: × 100). (6) Dilated normal ducts were identified by a zone of acidophilic non-elastic tissue inside the elastic ring surrounding the ducts. The arrowhead indicates the elastic ring and the arrow indicates acidophilic nonelastic tissue. (J: elastica van Gieson staining, original magnification: × 50). (7) In non-BVI, the pattern is similar to type III. There is no growth of cancer cells between the endothelium and the lamina elastica interna, while some cancer cells invaded the lamina elastica externa. The arrow indicates cancer cells invading the lamina elastica externa (K: HE staining, L: elastica van Gieson staining, M: factor VIII-related antigen staining, haematoxylin counter stain, original magnification: K–M × 50).
Statistical analysis
Statistical analysis of the data was performed with the Survival Tools for Statview-J 4.5 package (Abacus Concepts, Berkeley, CA, USA) on an Apple Power Macintosh 8100/100AV. The association between each parameter was assessed by Pearson's correlation coefficient. We examined the univariate relation between prognostic indicators and 20-year RFS and OS by fitting Kaplan–Meier survival curves (Kaplan and Meier, 1958) to various levels of the prognostic indicators. We then looked for differences among the curves using the log-rank test (Mantel, 1966). The Cox proportional hazards regression model was also used for the multivariate analysis (Cox, 1972).
Results
Clinical outcome
Among the 509 patients, there were 103 tumour-related recurrences and 83 tumour-related deaths (Table 1). In addition, there were 23 patients who were lost in the follow-up, 389 patients who are alive, and 14 patients who died of unrelated causes without recurrent tumours, with follow-up examinations of up to 20 years (median, 9 years).
Pearson's correlation between each parameter
The rate of AMC-high and BVI-positive tumours was 158 of 485 (32.6%), 148 of 505 (29.3%), respectively. That of both AMC-high and BVI-positive tumours was 49 of 483 (10.1%) (Table 1). Table 2 shows the association between each parameter. When comparing BVI and clinical tumour size, lymphnode status, histological grade, LVI, p53, PCNA, and MI, there were significant correlations among them. On the other hand, AMC weakly correlated with PCNA and c-erbB-2, but AMC/BVI correlated with lymph-node status, LVI, and PCNA (Table 2).
Univariate analysis
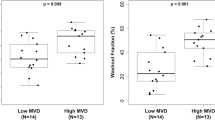
The prognostic factors found to be significantly associated with 20-year RFS were AMC/BVI (P<0.0001, Figure 2A), clinical tumour size, lymph-node status, histological grade, LVI, p53, PCNA, MI, and TN (Table 3). Moreover, AMC/BVI (P<0.0001, Figure 2B), clinical tumour size, lymph-node status, histological grade, LVI, p53, PCNA, c-erbB-2, MI, and TN were associated with 20-year OS. However, AI was not associated with either 20-year RFS or OS (Table 3).
Multivariate analysis
Table 4 shows that AMC/BVI was the strongest independent prognostic factor for 20-year RFS (relative risk (RR)=5.5; P<0.0001) and for 20-year OS (RR=4.3; P<0.0001) by multivariate analysis.
Stratification by lymph-node status
When stratified by lymph-node status, a significant impact of AMC/BVI on 20-year RFS or OS was seen in patients with node-negative and -positive carcinomas by univariate analysis (P<0.0001 or P<0.0001, and P<0.0001 or P<0.0001, respectively). We fitted a model with four factors: AMC/BVI, clinical tumour size, histological grade, and p53, in patients with node-negative carcinoma, and compared them by multivariate analysis. AMC/BVI was a significant independent factor for 20-year RFS or OS (RR=19.1; 95% confident interval (95% CI) =4.6–79.5; P<0.0001, or RR=20.3; 95% CI=3.3–127.1; P=0.0013, respectively). Moreover, AMC/BVI was a significant independent factor for 20-year RFS or OS in patients with node-positive carcinoma on multivariate analysis (RR=3.4; 95% CI=1.7–6.7; P=0.0005, or RR=2.9; 95% CI=1.4–6.2; P=0.0049, respectively). Patients with node-positive carcinoma who had AMC-high and BVI-positive tumours had a higher risk of cancer-related death than the patients with node-negative carcinoma who had AMC-low and BVI-negative tumours on RFS or OS (RR=54.9; 95% CI=16.1–186.4; P<0.0001, RR=61.0; 95% CI=14.0–266.6; P<0.0001, respectively, Figures 2A and B). There was no significant difference in 20-year RFS or OS between patients with node-negative carcinoma who had AMC-high and BVI-positive tumours, and patients with node-positive carcinoma who had AMC-low and BVI-negative tumours (P=0.9522 and P=0.6867, respectively, Figures 3A and B).
Characteristics of the treatment
We examined the effect of treatment in all patients for RFS and OS. The modality of operation was not associated with RFS or OS. However, adjuvant chemotherapy was significantly associated with OS but not with RFS (RR=1.6; 95% CI=1.0–2.5; P=0.0428, or RR=1.2; 95% CI=0.8–1.8; P=0.4927, respectively). Using interaction terms in the Cox proportional hazards model, we examined variations in the importance of AMC/BVI across treatment subgroups. In the subgroup of 94 patients without adjuvant therapy, the relative risk of both RFS and OS also associated with AMC/BVI was significant (RR=4.7; 95% CI=1.5–14.9; P=0.0085, and RR=4.3; 95% CI=1.4–13.8; P=0.0126, respectively). On the other hand, in the subgroup of 283 patients with chemotherapy, the relative risk of both RFS and OS associated with AMC/BVI remained significantly elevated (RR=6.8; 95% CI=3.0–15.4; P<0.0001, and RR=6.7; 95% CI=2.6–16.8; P<0.0001, respectively).
Discussion
Results of the present study confirm AMC/BVI as the strongest independent prognostic factor for 20-year RFS and OS in Japanese patients with breast cancer. AMC/BVI was also a significant independent factor for 20-year RFS or OS in patients with both node-negative and positive carcinomas; especially, the effect of the presence of AMC/BVI was clearer in patients with node-negative carcinomas than in those with node-positive carcinomas.
Some clinical studies suggested that to use an antibody to CD31 may be superior to using factor VIII-related antigen (Horak et al, 1992; Fox et al, 1994), however, the other study reported that this greater sensitivity of anti-CD31 of vascular endothelium did not yield more discriminating results for predicting survival outcome than results produced with factor VIII-related antigen (Gasparini et al, 1994). At that point, it may lack some acuracy; however, many stromal vessels can be stained very well and be taken in to account by factor VIII-related antigen staining as we published previously (Kato et al, 1999). When the authors compared AMC with the highest microvessel density in one or three fields (the hot spots) in the previous study, AMC was a more reliable factor than that of the hot spots (Kato et al, 1999). Therefore, we used AMC in this study. The results show that AMC was an independent prognostic factor, but its prognostic impact was not as strong as lymph-node status and clinical tumour size.
The rate of BVI fell within the range of 4.2–52.0% as observed in other studies (Teel and Sommers, 1964; Friedell et al, 1965; Sampat et al, 1977; Cooperative Breast Cancer Group, 1978; Martin et al, 1987; Fisher et al, 1993; Kister et al, 1996; Lauria et al, 1996; Kato et al, 2002). In this study, BVI in the breast cancer patients we observed was seen in 148 cases (29.3%). On the other hand, the rate of BVI examined by Lauria et al (1996) was 4.2%. They detected BVI using H&E staining alone, and the prevalence of BVI was particularly low in their study. In the previous study, when we evaluated BVI by H&E staining alone, the rate of BVI presented in 6.5%, which was similar to the study by Lauria et al (Lauria et al, 1996; Kato et al, 2002). By H&E staining alone, it was difficult to detect blood vessels filled with tumour cell emboli, to distinguish BVI from pseudoemboli resulting from shrinkage where cancer cells peeled off from the ducts because of poor fixing, to distinguish between small blood vessel invasion and LVI, to find the blood vessels with cancer cells growing between the endothelium and the lamina elastica interna, and to distinguish BVI from DCIS covered with elastic fibre (Figure 1, Kato et al, 2002). Therefore, there was a possibility of overlooking some kinds of blood vessel invasion using H&E staining alone. When Weigand et al (1982) and others (Sampat et al, 1977) examined the prognostic value of BVI, BVI correlated significantly with a high rate of recurrence. The results of our study suggest that BVI is an adverse prognostic factor among patients with breast cancer as well as lymph-node status. However, when Lauria et al (1996) examined the prognostic value of BVI, it was associated with shorter survival by univariate analysis but not significantly an independent factor by multivariate analysis. These discrepancies may be because of some technical reasons, especially the staining methods of BVI, number of cases studied, the different follow-up period and different races.
Average microvessel count and BVI retained an independent significance in association with RFS or OS by multivariate analysis (Table 4). Independent of lymph-node status, if there were AMC-low and BVI-negative tumours, we observed similar, excellent, long-term survival. Moreover, we used both factors to define a high-risk subset of all the tumours in cases that experienced a 48.1% recurrence or a 57.4% survival probability within 17 years (Figure 1A and B). There are likely to be worse prognoses when carcinomas acquire the ability to form AMC-high and BVI-positive tumours, which then become more important indications of outcome than lymph-node status and clinical tumour size. Our study suggests that even when tumours acquire a high degree of neovascularisation, it is impossible to form distant metastases without BVI and that AMC/BVI might be the most important and strongest predictive factor for tumour haemtogenous metastasis.
In recent studies, it has been suggested that examination for bone marrow micrometastasis using immunocytochemical methods in breast cancer patients would be useful as a prognostic marker (Braun et al, 2000). Moreover, other investigators reported that an assessment of tumour angiogenesis and vascular invasion give a reliable indication of the likelihood of the presence of bone marrow micrometastasis in patients with breast cancer and both processes contribute to metastases (Mansi et al, 1991; Fox et al, 1997). However, as they did not distinguish BVI from LVI, the meaning of the pathway of haematogenous metastastasis remains unclear. Although some investigators have indicated it impractical to distinguish between the blood and lymphatic vessel systems as independent routes of tumour dissemination because they are so interrelated (Fisher and Fisher, 1966), the present authors examined the difference between BVI and LVI in order to distinguish the different pathways to distant metastases. As vascular invasion includes the routes of both lymphatic and haematogenous dissemination, BVI alone may show haematogenous dissemination more accurately than vascular invasion. Haematogenous metastasis can be considered a complex process of cascading interregulated sequential steps. Average microvessel count and BVI include many steps that are necessary for haematogenous dissemination, that is, they are the results of tumour invasion to extracelluar matrices and basement membranes, entering the circulatory system, and activating angiogenesis at both the primary and distant sites. Our results suggest that tumours can spread directly via the blood-vascular system from their initial growth sites, and that biologically the significance of the combination of AMC and BVI is clearly more important than that of either BVI or AMC alone.
There are some reports that indicate adequate locoregional treatment for early breast cancer may prevent secondary dissemination (Hellman and Harris, 1987; Arriagada et al, 1995). However, Fisher et al (1981) maintained that breast cancer is a systemic disease and positive lymph nodes are not important instigators of distant disease. Several investigators have found no correlation between nodal metastases and bone-marrow metastases (Harbeck et al, 1994; Menard et al, 1994). Moreover, Menard et al (1994) reported that pathological nodal status was not a more reliable prognostic factor than the primary tumour score, including tumour size, grading, laminin receptor, and c-erbB-2. Our results suggest that tumours can spread directly through the blood-vascular system from their initial growth sites, and that lymph-node status was still considered a powerful prognostic indicator; however, biologically the combination of AMC and BVI is more significant than lymph-node status for tumour haematogenous dissemination.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arriagada R, Rutqvist LE, Mattsson A et al (1995) Adequate locoregional treatment for early breast cancer may prevent secondary dissemination. J Clin Oncol 13: 2869–2878
Baak JPA, van Dop H, Kurver HJ, Hermans JO (1985) The value of morphometry to classic prognosticators in breast cancer. Cancer 56: 374–382
Beenken SW, Grizzle WE, Crowe DR et al (2001) Molecular biomarkers for breast cancer prognosis: coexpression of c-erbB-2 and p53. Ann Surg 233: 630–638
Bloom HIJ, Richardson WW (1957) Histologic grading and prognosis. Br J Cancer 11: 359–377
Braun S, Pantel K, Muller P, Janni W, Hepp F, Kentenich CRM, Gastroph S, Wischnik A, Dimpfl T, Kindermann G, Riethmuller G, Schlimok G (2000) Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. N Engl J Med 342: 525–533
Clemente CG, Boracchi P, Andreola S, Del Vecchio M, Veronesi P, Rilke FO (1992) Peritumoural lymphatic invasion in patients with node-negative mammary duct carcinoma. Cancer 69: 1396–1403
Cooperative Breast Cancer Group (1978) Identification of breast cancer patients with high risk of early reccurence after radical mastectomy. II. Clinical and pathological correlations. Cancer 42: 2809–2826
Cox DR (1972) Regression models and life tables. J Roy Stat Soc B 34: 187–202
Fisher ER, Costantino J, Fisher B, Redmond C, Collaborating national surgical adjuvant breast bowel project investigators (1993) Pathologic findings from the national surgical adjuvant breast project (protocol 4) Discriminants for 15-year survival. Cancer 71: 2141–2150
Fisher B, Fisher ER (1966) The inter-relationship of hematogenous and lymphatic tumour cell dissemination. Surg Gynecol Obstet 122: 791–798
Fisher B, Wolmark N, Redmond C, Deutsch M, Fisher ER (1981) Findings from NSABP protocol No. B-04: comparison of radical mastectomy with alternative treatments. II. The clinical and biologic significance of medial-central breast cancers. Cancer 48: 1863–1872
Fox SB, Leek RD, Bliss J, Mansi JL, Gusterson B, Gatter KC, Harris AL (1997) Association of tumour angiogenesis with bone marrow micrometastases in breast cancer patients. J Natl Cancer Inst 89: 1044–1049
Fox SB, Leek RD, Smith K, Hollyer J, Greenall M, Harris AL (1994) Tumor angiogenesis in node-negative breast carcinomas-relationship with epidermal growth factor receptor, estrogen receptor, and survival. Breast Cancer Res Treat 29: 109–116
Friedell GH, Betts A, Sommers SC (1965) The prognostic value of blood vessel invasion and lymphocytic infiltrates in breast carcinoma. Cancer 18: 164–166
Gasparini G, Weidner N, Bevilacqua P, Maluta S, Palma PD, Caffo O, Barbareschi M, Boracchi P, Marubini E, Pozza F (1994) Tumour microvessel density, p53 expression, tumour size, and peritumoural lymphatic vessel invasion are relevant prognostic markers in node-negative breast carcinoma. J Clin Oncol 12: 454–466
Gilchrist KW, Gray R, Fowble B, Tormey DC, Taylor IV (1993) Tumour necrosis is a prognostic predictor for early recurrence and death in lymph-node positive breast cancer: a 10-year follow-up study of 729 Eastern Cooperative Oncology Group patients. J Clin Oncol 11: 1925–1935
Gould VE, Linnoila RL, Memoli VA, Warren WH (1983) Neuroendocrine components of the bronchopulmonary tract: hyperplasis, dysplasias, and neoplasms. Lab Invest 49: 519–537
Goulding H, Rashid NFNA, Robertson JF, Bell JA, Elston CW, Blamey RW, Ellis IO (1995) Assessment of angiogenesis in breast carcinoma: an important factor in prognosis? Hum Pathol 26: 1196–1200
Harbeck N, Untch M, Pachet l, Eiermann W (1994) Tumour cell detection in the bone marrow of breast cancer patients at primary therapy: results of 3-year median follow-up. Br J Cancer 69: 566–571
Heimann R, Ferguson D, Powers C, Recant WM, Weichselbaum RR, Hellman S (1996) Angiogenesis as a predictor of long-term survival for patients with node-negative breast cancer. J Natl Cancer Inst 88: 1764–1769
Hellman S, Harris J (1987) The appropriate breast carcinoma paradigm. Cancer Res 47: 339–342
Horak ER, Leek R, Klenk N, Lejeune S, Smith K, Stuart N, Greenall M, Stepniewska K, Harris AL (1992) Angiogenesis, assessed by platelet/endothelial cell adhesion molecule antibodies, as indicator of node metastases and survival in breast cancer. Lancet 340: 1120–1124
Kaplan EL, Meier P (1958) Non-parametric estimation from incomplete observations. J Am. Stat Assoc 53: 457–481
Kato T, Kameoka S, Kimura T, Nishikawa T, Kobayashi M (2002) Blood vessel invasion as a predictor of long-term survival for Japanese patients with breast cancer. Breast Cancer Res Treat 73: 1–12
Kato T, Kameoka S, Kimura T, Soga N, Abe Y, Nishikawa T, Kobayashi M (2001) Angiogenesis as a predictor of long-term survival for 377 Japanese patients with breast cancer. Breast Cancer Res Treat 70: 65–74
Kato T, Kimura T, Miyakawa R, Fujii A, Yamamoto K, Kameoka S, Nishikawa T, Kasajima T (2000) Clinicopathological study associated with long-term survival in Japanese patients with node-negative breast cancer. Br J Cancer 82: 404–411
Kato T, Kimura T, Miyakawa R, Nobue I, Fujii A, Yamamoto K, Kameoka S, Toshio N, Kasajima T (1999) The methodology of quantitation of microvessel density and prognostic value of neovascularization associated with long-term survival in Japanese patients with breast cancer. Breast Cancer Res Treat 53: 19–31
Kato T, Kimura T, Miyakawa R, Tanaka S, Fujii A, Yamamoto K, Kameoka S, Hamano K, Kawakami M, Aiba M (1997) Clinicopathologic study of angiogenesis in Japanese patients with breast cancer. World J Surg 21: 49–56
Kister SJ, Sommers SC, Haagensen CD, Cooley E (1996) Reevaluation of blood vessel invasion as a prognostic factor in carcinoma of the breast. Cancer 19: 1213–1216
Lauria R, Perrone F, Carlomagna C, De Laurentis M, Morabit A, Gallo C, Varriale E, Pettinato G, Panico L, Petrella G, Bianco AR, De Placido S (1996) The prognostic value of lymphatic and blood vessel invasion in operable breast cancer. Cancer 76: 1772–1778
Lee AKC, Delellis RA, Silverman ML, Heatley GJ, Wolfe HJ (1990) Prognostic significance of peritumoural lymphatic and blood vessel Invasion in node-negative carcinoma of the breast. J Clin Oncol 18: 1457–1465
Mansi JL, Easton D, Berger U, Gazet J-C, Ford HT, Dearnaley D, Coombes RC (1991) Bone marrow micrometastasis in primary breast cancer: prognostic significance after 6 years' follow-up. Eur J Cancer 27: 1552–1555
Mantel N (1966) Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep 50: 163–170
Martin SA, Perez-Reyes N, Mendelsonhn G (1987) Angiogenesis in breast carcinoma: an immunohistochemical study of factor VIII-related antigen. Cancer 59: 1918–1922
Menard S, Bufalino R, Rilke F, Cascinelli N, Veronesi U, Colnaghi MI (1994) Prognosis based on primary breast carcinoma instead of pathological nodal status. Br J Cancer 70: 709–712
Sampat MB, Sirsat MV, Gangadharan P (1977) Prognostic significance of blood vessel invasion in carcinoma of the breast in women. J Surg Oncol 9: 623–632
Simpson JF, Ahn C, Battifora H, Esteban JM (1996) Endothelial area as a prognostic indicator for invasive breast carcinoma. Cancer 77: 2077–2085
Sirvent JJ, Fortuno-Mar A, Olona M, Orti A (2001) Prognostic value of p53 protein expression and clinicopathological factors in infiltrating ductal carcinoma of the breast. A study of 192 patients. Histol Histopathol 16: 99–106
Teel P, Sommers SC (1964) Vascular invasion as a prognostic factor in breast carcinoma. Surg Gynecol Obstet 118: 1006–1008
Thor AD, Moore II DH, Edgerton SM, Kawasaki ES, Reihsaus E, Lynch HT, Marcus JN, Schwartz L, Chen LC, Mayall BH, Smith HS (1992) Accumulation of p53 tumour suppressor gene protein: an independent marker of prognosis in breast cancers. J Natl Cancer Inst 84: 1845–1855
van de Velde CJH, Gallager HS, Giacco GG (1986) Prognosis in node-negative breast cancer. Breast Cancer Res Treat 8: 189–196
Van Hoef MEHM, Knox WF, Dhesi SS, Howell A, Schor AM (1993) Assessment of tumour vascularity as a prognostic factor in lymph node-negative invasive breast cancer. Eur J Cancer 29: 1141–1145
Weidner N, Semple JP, Welch WR, Folkman J (1991) Tumour angiogenesis and metastasis-correlation in invasive breast carcinoma. N Engl J Med 324: 1–8
Weigand RA, Isenberg WM, Russo J, Brennan MJ, Rich MA (1982) Blood vessel invasion and axillary lymph-node involvement as prognostic indicators for human breast cancer. Cancer 50: 962–969
Wright C, Angus B, Nicholson S, Sainsbury JRC, Cairns J, Gullick WJ, Kelly P, Harris AL, Horne CHW (1989) Expression c-erbB-2 oncoprotein: a prognostic indicator in human breast cancer. Cancer Res 49: 2087–2090
Wyllie AH, Beattie GJ, Hargreaves AD (1981) Chromatin changes in apoptosis. Histochem J 13: 681–692
Zhang GJ, Kimijima I, Abe R, Watanabe T, Kanno M, Hara K, Tsuchiya A (1998) Apoptotic index correlates to bcl-2 and p53 protein expression, histological grade and prognosis in invasive breast cancers. Anticancer Res 18: 1989–1998
Acknowledgements
We thank Mr Minoru Sakurada and his colleagues for their work in the immunohistochemical staining and Mr Robert E Brandt for his help in editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kato, T., Kameoka, S., Kimura, T. et al. The combination of angiogenesis and blood vessel invasion as a prognostic indicator in primary breast cancer. Br J Cancer 88, 1900–1908 (2003). https://doi.org/10.1038/sj.bjc.6600921
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600921
Keywords
This article is cited by
-
Prognostic value of tumor necrosis based on the evaluation of frequency in invasive breast cancer
BMC Cancer (2023)
-
High lymphatic vessel density and presence of lymphovascular invasion both predict poor prognosis in breast cancer
BMC Cancer (2017)
-
Intratumoral and peritumoral lymphatic vessel density both correlate with lymph node metastasis in breast cancer
Scientific Reports (2017)
-
The influences of peritumoral lymphatic invasion and vascular invasion on the survival and recurrence according to the molecular subtypes of breast cancer
Breast Cancer Research and Treatment (2017)
-
Different types of tumor vessels in breast cancer: morphology and clinical value
SpringerPlus (2015)