Abstract
We present the long-term results of 18 chemotherapy relapsed indolent (N=12) or transformed (N=6) NHL patients of a phase II anti-CD20 131I-tositumomab (Bexxar®) therapy study. The biphasic therapy included two injections of 450 mg unlabelled antibody combined with 131I-tositumomab once as dosimetric and once as therapeutic activity delivering 75 or 65 cGy whole-body radiation dose to patients with normal or reduced platelet counts, respectively. Two patients were not treated due to disease progression during dosimetry. The overall response rate was 81% in the 16 patients treated, including 50% CR/CRu and 31% PR. Median progression free survival of the 16 patients was 22.5 months. Median overall survival has not been reached after a median observation of 48 months. Median PFS of complete responders (CR/CRu) has not been reached and will be greater than 51 months. Short-term side effects were mainly haematological and transient. Among the relevant long-term side effects, one patient previously treated with CHOP chemotherapy died from secondary myelodysplasia. Four patients developed HAMA. In conclusion, 131I-tositumomab RIT demonstrated durable responses especially in those patients who achieved a complete response. Six of eight CR/CRu are ongoing after 46–70 months.
Similar content being viewed by others
Main
Advanced stage follicular non-Hodgkin's lymphoma (NHL) is considered incurable by conventional therapy, while localized stage 1 or 2 NHL may be cured with external beam radiation therapy of involved sites (Mac Manus and Hoppe, 1996). Current radioimmunotherapy (RIT) is to be considered a combination of systemic radiation therapy and antibody-based immunotherapy. Both treatments reach tumour sites after i.v. application. Each of the two modalities, the unlabelled anti-CD20 antibody therapy and the corresponding RIT have been shown to be effective in follicular NHL (Buchsbaum et al, 1992; Kaminski et al, 1993; McLaughlin et al, 1998; Kaminski et al, 2005). The optimal combination of the two therapy strategies might have the potential to cure even advanced stage disease.
Recently, two radiolabelled antibodies targeting the CD20 antigen have been shown to lead to high percentages of complete remissions (Kaminski et al, 2000; Witzig et al, 2002b). Long lasting durable responses were reported for patients treated with 131I-tositumomab either upfront (Press et al, 2003; Kaminski et al, 2005; Leonard et al, 2005) or at recurrence after chemotherapy (Kaminski et al, 2000, 2001; Vose et al, 2000; Davies et al, 2004; Horning et al, 2005). A recent pooled analysis of studies in the relapsed/refractory disease setting has demonstrated long-term durable responses lasting 4 years or more associated with a single treatment of 131I-tositumomab (Fisher et al, 2005). Similar response rates including durable responses were reported for RIT with 90Y-ibritumomab tiuxetan (Zevalin®) (Gordon et al, 2004b).
Compared with RIT based on 131I-labelled antibodies that has to be performed in specially equipped radioprotection units in Europe, using 90Y as the label allows outpatient treatment. In the US, 131I-tositumomab is administered as an outpatient treatment. The use of 131I also has clinical advantages. The low energy electrons are well adapted for treatment of small or minimal disease (Sharkey et al, 1991; Vogel et al, 1997) and the long experience with 131I-therapy of thyroid disease has shown excellent tolerance (Hall et al, 1992; Schlumberger and De Vathaire, 1996). Labelling with 131I can be performed while completely maintaining antibody immunoreactivity (Schaffland et al, 2004). The use of dosimetry for 131I-tositumomab allows for patient specific dosing.
Recently, a particularly high percentage of long lasting complete responses was reported by Davies et al (2004) in 41 relapsed patients treated in England with 131I-tositumomab. As the second European centre participating in this multicentre study, we report here the experience from Switzerland with the particular focus on the long-term efficacy of this 131I-RIT.
Patients and methods
This single arm, open-label phase II study of Corixa Corp., South San Francisco, CA and GlaxoSmithKline, Philadelphia, PA, USA aimed to establish the response rate to 131I-tositumomab in patients after first or multiple recurrences of indolent or transformed B-cell lymphoma. Duration of response, safety and survival were secondary end points. The study was conducted in two centres in Switzerland. Patients gave their written informed consent to the study protocol that had been approved by the local Ethics Committees of the University Hospitals of Lausanne and Geneva as well as the Radioprotection Section of the Swiss Federal Office of Public Health.
Patient eligibility
Patients had to present a histologically confirmed, CD20 positive follicular, small lymphocytic or MALT non-Hodgkin's B-cell lymphoma, in relapse after at least one full regimen of chemotherapy. Patients with transformed NHL were also eligible. Measurable minimal two-dimensional tumour diameter was ⩾2 cm. A HAMA (human anti-mouse antibody) test had to be negative at study entry. Adequate bone marrow function was to be documented with neutrophils ⩾1.5 × 109 l−1 and platelets ⩾100 × 109 l−1. Maximal acceptable lymphoma infiltration of bone marrow was 25%, as determined with trephine biopsy.
A minimal waiting period of 4 weeks was required after cytotoxic chemotherapy, radiotherapy or cytokine therapy. Patients having had high-dose chemotherapy or radiation therapy including stem cell rescue were excluded from the study as well as patients with known HIV infection, active hydronephrosis, and those treated previously with RIT.
Dosimetric and therapeutic antibody administrations
Unlabelled and radiolabelled antibody tositumomab was provided by Corixa Corp., South San Francisco, CA and GlaxoSmithKline, Philadelphia, PA, USA. Dosimetric and therapeutic 131I-labelling of tositumomab was performed centrally (MDS Nordion Inc., Kanata, Canada) and the labelled compound was shipped frozen on a per patient basis. Two arbitrarily selected therapeutic batches of 131I-tositumomab were analysed for immunoreactivity using the Lindmo approach (Lindmo et al, 1984). Immunoreactivity was measured immediately after upfreezing the batches for injection of patients. About 6 ng 131I-tositumomab were incubated for 2 h at 37°C with five serial dilutions of 1–10 × 106 fresh, exponentially grown Raji or Daudi B lymphoma cells in duplicates. Cell-bound activity was determined and expressed in % of incubated activity, specific binding, after subtraction of nonspecific binding, was determined and expressed as percent of incubated activity and immunoractivity determined using double inverse plot (Lindmo et al, 1984) with extrapolation at infinite antigen excess.
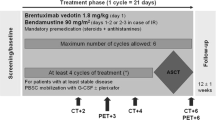
Patient preparation included thyroid blocking with 2 × 100 mg KI per day orally and premedication with 500 mg paracetamol and 2 mg clemastine, taken orally. Unlabelled and radiolabelled tositumomab regimen consisted of two steps as described previously (Kaminski et al, 1993; Kaminski et al, 2005). Shortly, in the first dosimetry step, patients received 450 mg unlabelled tositumomab in a 1 h infusion followed immediately by that of 35 mg 131I-tositumomab (185 MBq). The second, therapeutic step consisted again of the infusion of 450 mg unlabelled tositumomab over 1 h followed by that of 35 mg 131I-tositumomab labelled with the activity calculated to deliver 75 cGy total body dose for patients with normal, and 65 cGy for patients with reduced platelet counts (100–150 G l−1).
For dosimetry, patients were scanned with a large field of view dual head gamma camera (BIAD, Trionix, Twinsburg, Ohio, or Prism 2000, Picker) equipped with high-energy parallel collimators and using a matrix of 1024 × 256. Camera uniformity, background and energy peaks were checked daily. Scanning was performed as described by Wahl et al (1998). Patients were scanned under identical conditions, on day 0 immediately after antibody perfusion (referred to as 100% reference scan), on day 2, 3 or 4 and on day 6 or 7. The background corrected activities of days 2, 3 or 4 and day 6 or 7 were expressed in % of activity measured on day 0 and fitted to a semi-logarithmic scale allowing to directly read, from the exponential curve-fit, the whole-body effective half-life and retention time of 131I-labelled tositumomab. Using the published tabulated whole-body dosimetry data (Wahl et al, 1998), the 131I-tositumomab activity was extrapolated that delivered 75 cGy to patients with normal BM function or 65 cGy to patients with reduced platelet counts.
Response evaluation
Tumour response evaluation, including physical examination, computed tomography (CT) of the neck, chest, abdomen and pelvis and bone marrow biopsy if involved before treatment, was performed at weeks 13 and 26 and every 6 months thereafter until disease progression or death. A complete response (CR) was defined as complete resolution of all disease-related radiologic abnormalities and clinical symptoms. An unconfirmed CR (CRu) was defined as complete resolution of clinical disease symptoms and residual focal stable radiologic abnormalities of ⩽2 cm diameter according to the International Workshop criteria (Cheson et al, 1999). A partial response (PR) was defined as >50% reduction of two-dimensional tumour size and progressive disease as ⩾25% increase of the two-dimensional tumour size. Progression free survival (PFS) was defined as time from treatment initiation to first documentation of progression or death and overall survival (OS) as time from treatment start to death.
Evaluation of toxicity and safety
All adverse events from study entry through to week 13 were graded according to the National Cancer Institute Common toxicity criteria. Adverse events after this period considered to be possibly or probably related with study drug were also recorded. Detailed blood analysis was performed weekly from study week 3–9 or until recovery and repeated at 13 and 26 weeks and every 6 months thereafter until 2 years. Other toxicity evaluations included blood chemistry and TSH assays for all patients basically all 6 months up to 2 years. Long-term evaluations after 2 years from treatment were performed every 6 months.
HAMA assay
The HAMA assay (HAMA Elisa, Medac, Hamburg, Germany) was performed for all patients and had to be negative at inclusion. The HAMA assay was repeated at 7, 13 and 26 weeks after therapy and every 6 months thereafter.
Statistical analysis
Statistical analysis was performed for patients who had received the therapeutic activity of radiolabelled antibody. PFS and OS were analysed using the Kaplan Meier analysis of the UNISTAT 5.5® statistical package for Windows (2002 edition, Unistat Ltd, London, England, run on Windows XP). Survival differences among patients subgroups were analysed using the Wilcoxon χ2 statistics (Gehan evaluation). P-values <0.05 were considered significant.
Results
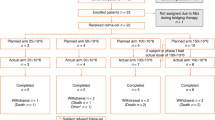
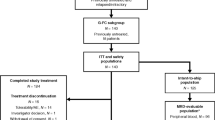
In all, 18 patients were included in the study. Their characteristics and their lymphoma history are shown in Table 1. Two patients with transformed disease did not receive the administration of therapeutic 131I-tositumomab activity because of rapid disease progression during the dosimetry phase.
As concerning chemotherapy regimens, the eight patients experiencing CR after RIT had a mean of 2.5 chemo/rituximab treatments and one patient had RT before inclusion. In detail, 88% of these patients had received anthracyclines, 75% alkylating agents and 63% rituximab. The eight patients experiencing PR or PD after RIT had a mean of 3.4 chemo/rituximab treatments and two patients had RT before inclusion. In detail, all of these patients had been treated with both anthracyclines and alkylating agents and 75% with rituximab.
Pharmacokinetics
After the injection of the dosimetric activity of 185 MBq 131I-tositumomab, the whole-body scintigraphies revealed a single exponential radioactivity decrease in all patients with a mean effective half-life of 64.2±8.7 h was observed (range 47.9–77.8 h). An average therapeutic activity of 2.9±0.6 GBq (range 1.9–3.9 GBq) 131I-tositumomab was administered after a mean delay of 8 days after dosimetry (Figure 1). Immunoreactivity of two arbitrarily selected therapeutic batches of 131I-tositumomab revealed as very high at extrapolation to infinite antigen excess with results ranging between 95.2 and 100%.
Anterior and posterior whole-body scans of patient Corixa Nr. 721 are shown recorded 6 days after injection of therapeutic 131I-tositumomab activity (3.0 GBq). Antibody uptake is clearly visualized (arrows) in the left jugular, right axillar, left mediastinal, right iliac and right inguinal adenopathies. R=right, L=left. Thyroid uptake of 131I was significant in this patient despite thyroid blockade with oral KI. Six days after injection, blood pool activity remains high.
Response and survival
The overall response rate was 81% in the 16 patients treated, including 50% CR/CRu and 31% PR. Median PFS of the 16 treated patients was 22.5 months. Median overall survival has not been reached after a median observation time of 48 months (Figure 2).
All 12 patients with indolent lymphoma responded, eight with CR or CRu and four with PR. After a median follow-up of 45.5 months, the median PFS of the 12 indolent lymphoma patients has not been reached. The PFS of the four patients in PR ranged from 6 to 17 months. Median PFS of complete responders (CR and CRu) has not been reached but will be greater than 51 months (Figure 3). In fact, only one of the eight CR/CRu patients presented a relapse at 28 months. Another patient in CRu died from secondary myelodysplastic syndrome (MDS) and leukaemia 45 months after RIT, as described below. Six patients remain currently in ongoing CR/CRu, two of them being disease free 4 years after therapy and three others after more than 5 years. These six patients had previously been treated with a mean of 2.7 chemo-immunotherapy regimens (range 1–5), two of them had also received radiotherapy.
Kaplan–Meier plots show PFS of 13 responding patients, 12 presenting with relapsed indolent lymphoma and one with transformed disease. Results are shown according to the response, PR or CR/CRu. Note that of the eight patients with CR/CRu, one patient has relapsed at 28 months and one patient died at 45 months from secondary leukaemia, the other six patients are in ongoing CR/CRu.
Of the five patients treated with transformed disease, one had a partial response that lasted 10 months. The three other patients progressed and required further treatment before treatment-related haematological toxicity was resolved.
χ2 Wilcoxon analysis indicated a highly significant difference (P<0.005) of PFS in patients with non-transformed (N=12) compared with transformed disease (N=4). However, given the very low number of patients with transformed disease who actually received the RIT, this statistical comparison must be considered with caution. Other parameters were evaluated for patients with non-transformed disease (N=12). The analysis indicated that stage of disease, bone marrow involvement, tumour size, age, gender, number of previous chemotherapies, platelet counts, LDH level, and time from initial diagnosis were not significantly linked with treatment outcome (P>0.25).
Toxicity
During first perfusion of unlabelled tositumomab, one patient had a fall of blood pressure that required adjustment of the infusion rate and another patient developed grade 2 abdominal pain requiring opioid treatment.
All 16 treated patients showed either enhanced pre-existing or newly developing bone marrow depression in at least two cell lineages (Table 2). Bone marrow depression was minor (grade 1 or 2) in four patients. The other 12 patients showed grade 3 (five patients) or 4 (seven patients) toxicity in one or more lineages. The median degree of PMN, leukocyte and platelet depression after RIT was grade 3, that of haemoglobin grade 1. The median duration of toxicity greater than grade 2 was 21–27 (Table 2). One patient had the leukocyte and PMN nadir particularly late and was recovering from these grade 3 and 4 toxicities, respectively, after week 13. Another patient with transformed disease required further treatment 7 weeks after RIT because of disease progression while still in grade 3 haematological toxicity. Some minor toxicities grade 1 or 2 were still observed in the other 14 patients 13 weeks post-treatment.
In all, 29 nonhaematologic side effects, mostly mild (grade 1 or 2) possibly or probably linked with RIT, were reported for nine patients. They included pain, fatigue, fever, chills, sweating, rash, arthralgia, erythaema and oedema, a pneumonia and a thyroiditis. One febrile lymphadenitis during pancytopenia and one febrile neutropenia, both grade 3, were observed at 7 and 8 weeks post RIT and resolved both rapidly under antibiotic therapy. One patient developed elevated TSH without requiring hormone replacement.
Four patients developed HAMA. Interestingly, all positive HAMA results were observed among the patients who responded with CR/CRu, suggestive of a significant association (P< 0.05) in a multigroup comparison according to Tukey-HSD. The four HAMA positive patients are still alive without relapse.
The most serious adverse event was a myelodysplastic syndrome (MDS) that appeared 34 months after RIT in one patient who eventually died from secondary leukæmia. However, this patient was previously treated with five cycles of chemotherapy (CHOP), with which he reached a PR. At progression of disease, 19 months later, he was treated with rituximab, but a major para-aortic mass showed continued growth. He was included in the RIT study 40 months after initial diagnosis and initial CHOP chemotherapy and he presented a bulky abdominal mass. RIT with 3.6 GBq 131I-tositumomab resulted in CRu without further change over the rest of follow-up (stable CT over more than 2 years). MDS was diagnosed 34 months after RIT and 74 months after initial chemotherapy. It evolved into secondary leukaemia with fatal outcome 11 months later.
Discussion
Results of 16 patients treated with 131I-tositumomab RIT for relapsed indolent or transformed lymphoma are presented. The long-term results in low-grade disease are very encouraging, considering that 6 out of 12 patients are disease free after 46 to 70 months.
The initial phase I-II studies with 131I-tositumomab reported CR in approximately one third of the patients, with half of them relapsing within 20 months (Kaminski et al, 2000). The CR rate was 20% in the pivotal study, and half of these complete responders remained disease free for more than 4 years (Kaminski et al, 2001). A more recent report (Davies et al, 2004) showed 20 CR/CRu (49%) out of 41 patients treated, with a median duration of the CR/CRu not yet reached, but will exceed 2.5 years. Our results compare well with these previous studies, showing 50% CR/CRu, the median PFS for these patients being not reached after a median follow-up of >4 years. Such an outcome is unusual in this population of largely pretreated patients, considering that the natural history of indolent lymphomas is typically characterized by continuous relapses with remissions becoming shorter after each progression (Gallagher et al, 1986). It is impressive to note that two of the patients who were in relapse after 4 or 5 lines of chemo-immunotherapy remain in CR 61 and 67 months following RIT.
The impressive efficacy of 131I-tositumomab in some patients with chemotherapy resistant disease, would suggest that RIT should be used earlier in the treatment course of indolent lymphoma for optimal clinical benefit. To explore this hypothesis, a recent analysis of more than 1000 patients was conducted to examine the efficacy of 131I-tositumomab by line of therapy. This analysis revealed that both the frequency of long-term durable responders and the rate of CR was higher when 131I-tositumomab was used earlier in the treatment sequence (Gregory et al, 2005). Interesting results have also been reported for follicular lymphoma treated upfront with a single treatment of 131I-tositumomab (Kaminski et al, 2005). In this latter study, CR were observed in 75% of patients, relapse free survival of these patients was 77% at 5 years. Impressive results have also been observed when 131I-tositumomab has been combined with chemotherapy in the upfront setting (Press et al, 2003; Leonard et al, 2005). Rituximab has been shown to improve the outcome of patients with previously untreated follicular lymphoma when associated with chemotherapy (Marcus et al, 2005). Several other reports suggest that first line combination of rituximab and anthracycline-containing chemotherapy is able to induce very high response rates and prolonged remission, including molecular remission (Hiddemann et al, 2003; Salles et al, 2004; Zinzani et al, 2004; Czuczman et al, 2005). Both chemo-immunotherapy and RIT appear as attractive options for treatment of indolent lymphoma, but the best long-term strategy still needs to be determined. A randomized phase III study by the SWOG comparing R-CHOP to 131I-tositumomab-CHOP is currently ongoing and will address the question of the optimal treatment in the front-line setting.
The results published by Davies et al (2004) and our data suggest that 131I-tositumomab RIT is at least equivalent to 90Y-ibritumomab tiuxetan (Zevalin®) (Gordon et al, 2004b). Indeed, in the rituximab refractory setting, efficacy may be more favourable for 131I-tositumomab when reviewing two separate phase II studies of both these agents. The PFS for responders treated with 131I-tositumomab was 24.5 months vs 8.7 months for similar patients treated with 90Y-ibritumomab tiuxetan (Witzig et al, 2002a; Horning et al, 2005). This observation may be explained by the fact that the unlabelled antibody used with ibritumomab tiuxetan is rituximab, which was being administered to patients who were already resistant to rituximab. The efficacy results of 131I-tositumomab also compared favourably with 90Y-ibritumomab tiuxetan in two separate recent analyses of the long-term durable responder patient populations (defined as time to progression of ⩾12 months) treated with both these agents (Fisher et al, 2005; Wiseman and Witzig, 2005). Compared with rituximab in a randomized phase III study, 90Y-ibritumomab tiuxetan was shown to induce 34% of CR/CRu vs 20% for rituximab and a median time to progression (TTP) of 15 versus 10.2 months. In patients who achieved CR/CRu TTP was 24.7 months for RIT and 13.2 months for rituximab alone (Gordon et al, 2004b). Other phase II trials with 90Y-ibritumomab tiuxetan reported CR/Cru rates between 15 and 51% (Wiseman et al, 2002; Witzig et al, 2002a; Gordon et al, 2004a) the follow-up being frequently shorter compared with the present study or that of Davies (Davies et al, 2004). Therefore, it is clear that both agents have demonstrated high levels of efficacy in patients with relapsed/refractory disease.
In the present study, we observed a single patient who developed secondary myelodysplasia 34 months after RIT and 74 months after first-line chemotherapy. The standard CHOP chemotherapy or/and 131I-tositumomab RIT may have contributed to this evolution. Both the alkylating agents and doxorubicin, constituents of CHOP, are known to induce increased risk of myelodysplasia and secondary leukaemia, as does also total body irradiation (Armitage et al, 2003). The risk of MDS seems to be particularly increased when radiotherapy (RT) is associated with alkylating agents. It is globally estimated that 10% of patients treated for lymphoma will develop secondary MDS/AML within 10 years of primary therapy (Armitage et al, 2003). Thus, the myelodysplasia developing 74 months after initial therapy in a single patient does not allow to conclude on the role of RIT in the course of the illness of this patient. It is also noted that no secondary myelodysplasia was observed in the other report from the English group using the same treatment protocol (Davies et al, 2004), and that large cohort studies analysing patients treated with RIT did not show any obvious increase in the incidence of secondary MDS/AML, compared with similar patients treated with conventional therapies (Witzig et al, 2003; Bennett et al, 2005). In addition, when 131I-tositumomab was administered as a single agent in the front-line setting, no cases of MDS/AML were observed after 5 years of follow-up (Kaminski et al, 2005).
Both 131I-tositumomab and 90Y-ibritumomab tiuxetan RIT consist of a combination of radiolabelled with unlabelled antibody. The unlabelled antibody, however, might not be used optimally. A randomized study performed in patients with follicular lymphoma has shown that different schedules using rituximab in maintenance following the standard 4 weeks treatment were significantly improving the event free survival of responders (Ghielmini et al, 2004). As RIT is given in a similar patient population, higher overall and complete response rates and longer event-free survival might possibly be achieved by using prolonged treatment with unlabelled antibody following RIT administration.
Another remark concerns the half-life of 131I-tositumomab. It has been argued that a long-lived radiolabelled antibody might induce bone marrow and normal tissue toxicity, whereby limiting the amount of activity that can be administered, but there have never been any published clinical data reported to support this theory, to our knowledge. In the 16 patients treated here, 131I-tositumomab showed a mean whole-body half-live of 64.2 h. In comparison, 90Y-Zevalin was reported to have a median blood effective half-live of 27 h (Wiseman et al, 2003). The observed efficacy of 131I-tositumomab rather argues against the hypothesis that antibodies labelled with longer-lived radionuclides are potentially more harmful than those with shorter-lived radionuclides. Instead, one might argue that the observed efficacy of 131I-tositumomab could be linked with the prolongation of therapeutic radiation delivery over several days, allowing therefore repair, repopulation, redistribution and reoxygenation processes to occur in tumour and normal tissues, as it is the case in standard fractionation radiotherapy (Thames and Hendry, 1987).
A final comment concerns the observation of HAMA in the group of CR patients with long-term survival. Indeed, appearance of HAMA could potentially also induce anti-HAMA antibodies, which could in turn be anti-idiotype antibodies and therefore directed against CD20. Since anti-CD20 antibodies are efficient as lymphoma therapy, anti-idiotype antibodies developed by the patient could represent a long-term treatment to lymphoma provided by the patient himself. However, since tositumomab is a mouse antibody, the HAMA response most probably represents an anti-constant domain antibody and not an anti-idiotype. The correlation of positive HAMA in connection with long-term tumour-free survival might, therefore, rather reflect a preserved immune competence of these patients. Preserved immune competence could be decisive in connection with the use of the unlabelled antibodies that develop efficacy based probably on ADCC and CDC as shown by different studies. Interestingly, a recent report, published while this article was reviewed (Azinovic et al, 2006), also described a survival benefit associated with HAMA.
Conclusion
Our data have shown high overall and complete response rates combined with the observation of long-term progression free survivals of CR/CRu in recurrent indolent NHL. Toxicity was mild except in one patient who developed a secondary myelodysplastic syndrome that evolved into secondary leukaemia. However, this observation does not allow any particular deduction at this time on the part of RIT in the cause of this disease. Overall, these data confirm and extend the previously reported results with 131I-tositumomab, a treatment shown to be able to bring a significant number of indolent, relapsed NHL into long-lasting complete responses. Our findings in patients at first or second relapse, along with other published reports, also suggest that 131I-tositumomab should be administered early in the course of relapsed disease for optimal clinical benefit.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Armitage JO, Carbone PP, Connors JM, Levine A, Bennett JM, Kroll S (2003) Treatment-related myelodysplasia and acute leukemia in non-Hodgkin's lymphoma patients. J Clin Oncol 21: 897–906
Azinovic I, DeNardo GL, Lamborn KR, Mirick G, Goldstein D, Bradt BM, DeNardo SJ (2006) Survival benefit associated with human anti-mouse antibody (HAMA) in patients with B-cell malignancies. Cancer Immunol Immunother (online)
Bennett JM, Kaminski MS, Leonard JP, Vose JM, Zelenetz AD, Knox SJ, Horning S, Press OW, Radford JA, Kroll SM, Capizzi RL (2005) Assessment of treatment-related myelodysplastic syndromes and acute myeloid leukemia in patients with non-Hodgkin lymphoma treated with tositumomab and iodine I131 tositumomab. Blood 105: 4576–4582
Buchsbaum DJ, Wahl RL, Normolle DP, Kaminski MS (1992) Therapy with unlabeled and 131I-labeled pan-B-cell monoclonal antibodies in nude mice bearing Raji Burkitt's lymphoma xenografts. Cancer Res 52: 6476–6481
Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-Lopez A, Hagenbeek A, Cabanillas F, Klippensten D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP (1999) Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. NCI Sponsored International Working Group. J Clin Oncol 17: 1244
Czuczman MS, Koryzna A, Mohr A, Stewart C, Donohue K, Blumenson L, Bernstein ZP, McCarthy P, Alam A, Hernandez-Ilizaliturri F, Skipper M, Brown K, Chanan-Khan A, Klippenstein D, Loud P, Rock MK, Benyunes M, Grillo-Lopez A, Bernstein SH (2005) Rituximab in combination with fludarabine chemotherapy in low-grade or follicular lymphoma. J Clin Oncol 23: 694–704
Davies AJ, Rohatiner AZ, Howell S, Britton KE, Owens SE, Micallef IN, Deakin DP, Carrington BM, Lawrance JA, Vinnicombe S, Mather SJ, Clayton J, Foley R, Jan H, Kroll S, Harris M, Amess J, Norton AJ, Lister TA, Radford JA (2004) Tositumomab and iodine I 131 tositumomab for recurrent indolent and transformed B-cell non-Hodgkin's lymphoma. J Clin Oncol 22: 1469–1479
Fisher RI, Kaminski MS, Wahl RL, Knox SJ, Zelenetz AD, Vose JM, Leonard JP, Kroll S, Goldsmith SJ, Coleman M (2005) Tositumomab and Iodine-131 Tositumomab Produces Durable Complete Remissions in a Subset of Heavily Pretreated Patients With Low-Grade and Transformed Non-Hodgkin's Lymphomas. J Clin Oncol 23: 7565–7573
Gallagher CJ, Gregory WM, Jones AE, Stansfeld AG, Richards MA, Dhaliwal HS, Malpas JS, Lister TA (1986) Follicular lymphoma: prognostic factors for response and survival. J Clin Oncol 4: 1470–1480
Ghielmini M, Schmitz SF, Cogliatti SB, Pichert G, Hummerjohann J, Waltzer U, Fey MF, Betticher DC, Martinelli G, Peccatori F, Hess U, Zucca E, Stupp R, Kovacsovics T, Helg C, Lohri A, Bargetzi M, Vorobiof D, Cerny T (2004) Prolonged treatment with rituximab in patients with follicular lymphoma significantly increases event-free survival and response duration compared with the standard weekly x 4 schedule. Blood 103: 4416–4423
Gordon LI, Molina A, Witzig T, Emmanouilides C, Raubitschek A, Darif M, Schilder RJ, Wiseman G, White CA (2004a) Durable responses after ibritumomab tiuxetan radioimmunotherapy for CD20+ B-cell lymphoma: long-term follow-up of a phase I/II study. Blood 103: 4429–4431
Gordon LI, Witzig T, Molina A, Czuczman M, Emmanouilides C, Joyce R, Vo K, Theuer C, Pohlman B, Bartlett N, Wiseman G, Darif M, White C (2004b) Yttrium 90-labeled ibritumomab tiuxetan radioimmunotherapy produces high response rates and durable remissions in patients with previously treated B-cell lymphoma. Clin Lymphoma 5: 98–101
Gregory SA, Leonard JP, Vose JM, Zelenetz AD, Horning SJ, Knox SJ, Lister TA, Radford JA, Press OW, Kaminski MS (2005) Superior outcomes associated with earlier use: Experience with tositumomab and iodine I-131 tositumomab in 1177 patients (pts) with low-grade, follicular and transformed non-Hodgkin's lymphoma (NHL). ASCO Meeting Abstracts 23: 6561
Hall P, Boice Jr JD, Berg G, Bjelkengren G, Ericsson UB, Hallquist A, Lidberg M, Lundell G, Mattsson A, Tennvall J (1992) Leukaemia incidence after iodine-131 exposure. Lancet 340: 1–4
Hiddemann W, Dreyling MH, Forstpointer R, Kneba M, Woermann B, Lengfelder E, Schmits R, Reiser M, Metzner B, Schmitz N, Truemper L, Eimermacher H, Parwaresch R (2003) Combined immuno-chemotherapy (R-CHOP) significantly improves time to treatment failure in first line therapy of follicular lymphoma – Results of a prospective randomized trial of the German low grade lymphoma study group (GLSG). Blood 102: 104
Horning SJ, Younes A, Jain V, Kroll S, Lucas J, Podoloff D, Goris M (2005) Efficacy and safety of tositumomab and iodine-131 tositumomab (Bexxar) in B-cell lymphoma, progressive after rituximab. J Clin Oncol 23: 712–719
Kaminski MS, Estes J, Zasadny KR, Francis IR, Ross CW, Tuck M, Regan D, Fisher S, Gutierrez J, Kroll S, Stagg R, Tidmarsh G, Wahl RL (2000) Radioimmunotherapy with iodine (131)I tositumomab for relapsed or refractory B-cell non-Hodgkin lymphoma: updated results and long-term follow-up of the University of Michigan experience. Blood 96: 1259–1266
Kaminski MS, Tuck M, Estes J, Kolstad A, Ross CW, Zasadny K, Regan D, Kison P, Fisher S, Kroll S, Wahl RL (2005) 131I-tositumomab therapy as initial treatment for follicular lymphoma. N Engl J Med 352: 441–449
Kaminski MS, Zasadny KR, Francis IR, Milik AW, Ross CW, Moon SD, Crawford SM, Burgess JM, Petry NA, Butchko GM (1993) Radioimmunotherapy of B-cell lymphoma with [131I]anti-B1 (anti-CD20) antibody. N Engl J Med 329: 459–465
Kaminski MS, Zelenetz AD, Press OW, Saleh M, Leonard J, Fehrenbacher L, Lister TA, Stagg RJ, Tidmarsh GF, Kroll S, Wahl RL, Knox SJ, Vose JM (2001) Pivotal study of iodine I 131 tositumomab for chemotherapy-refractory low-grade or transformed low-grade B-cell non-Hodgkin's lymphomas. J Clin Oncol 19: 3918–3928
Leonard JP, Coleman M, Kostakoglu L, Chadburn A, Cesarman E, Furman RR, Schuster MW, Niesvizky R, Muss D, Fiore J, Kroll S, Tidmarsh G, Vallabhajosula S, Goldsmith SJ (2005) Abbreviated chemotherapy with fludarabine followed by tositumomab and iodine I 131 tositumomab for untreated follicular lymphoma. J Clin Oncol 23: 5696–5704
Lindmo T, Boven E, Cuttitta F, Fedorko J, Bunn Jr PA (1984) Determination of the immunoreactive fraction of radiolabeled monoclonal antibodies by linear extrapolation to binding at infinite antigen excess. J Immunol Methods 72: 77–89
Mac Manus MP, Hoppe RT (1996) Is radiotherapy curative for stage I and II low-grade follicular lymphoma? Results of a long-term follow-up study of patients treated at Stanford University. J Clin Oncol 14: 1282–1290
Marcus R, Imrie K, Belch A, Cunningham D, Flores E, Catalano J, Solal-Celigny P, Offner F, Walewski J, Raposo J, Jack A, Smith P (2005) CVP chemotherapy plus rituximab compared with CVP as first-line treatment for advanced follicular lymphoma. Blood 105: 1417–1423
McLaughlin P, Grillo-Lopez AJ, Link BK, Levy R, Czuczman MS, Williams ME, Heyman MR, Bence-Bruckler I, White CA, Cabanillas F, Jain V, Ho AD, Lister J, Wey K, Shen D, Dallaire BK (1998) Rituximab chimeric anti-CD20 monoclonal antibody therapy for relapsed indolent lymphoma: half of patients respond to a four-dose treatment program. J Clin Oncol 16: 2825–2833
Press OW, Unger JM, Braziel RM, Maloney DG, Miller TP, LeBlanc M, Gaynor ER, Rivkin SE, Fisher RI (2003) A phase 2 trial of CHOP chemotherapy followed by tositumomab/iodine I 131 tositumomab for previously untreated follicular non-Hodgkin lymphoma: Southwest Oncology Group Protocol S9911. Blood 102: 1606–1612
Salles GA, Foussard C, Mounier N, Morschhauser F, Doyen C, Lamy T, Haioun C, Brice P, Bouabdallah R, Rossi J-F, Audhuy B, Fermé C, Mahe B, Feugier P, Sebban C, Colombat P, Xerri L (2004) Rituximab added to aIFN+CHVP improves the outcome of follicular lymphoma patients with a high tumor burden: First analysis of the GELA-GOELAMS FL-2000 randomized trial in 359 patients. Blood 104: 48
Schaffland AO, Buchegger F, Kosinski M, Antonescu C, Paschoud C, Grannavel C, Pellika R, Bischof Delaloye A (2004) 131I-Rituximab: relationship of immunoreactivity with specific activity. J Nucl Med 45: 1784–1790
Schlumberger M, De Vathaire F (1996) [131 iodine: medical use. Carcinogenic and genetic effects]. Ann Endocrinol (Paris) 57: 166–176
Sharkey RM, Weadock KS, Natale A, Haywood L, Aninipot R, Blumenthal RD, Goldenberg DM (1991) Successful radioimmunotherapy for lung metastasis of human colonic cancer in nude mice. J Natl Cancer Inst 83: 627–632
Thames HD, Hendry JH (1987) Fractionation in radiotherapy. London-New York-Philadelphia: Taylor and Francis
Vogel CA, Galmiche MC, Buchegger F (1997) Radioimmunotherapy and fractionated radiotherapy of human colon cancer liver metastases in nude mice. Cancer Res 57: 447–453
Vose JM, Wahl RL, Saleh M, Rohatiner AZ, Knox SJ, Radford JA, Zelenetz AD, Tidmarsh GF, Stagg RJ, Kaminski MS (2000) Multicenter phase II study of iodine-131 tositumomab for chemotherapy-relapsed/refractory low-grade and transformed low-grade B-cell non-Hodgkin's lymphomas. J Clin Oncol 18: 1316–1323
Wahl RL, Kroll S, Zasadny KR (1998) Patient-specific whole-body dosimetry: principles and a simplified method for clinical implementation. J Nucl Med 39: 14S–20S
Wiseman GA, Gordon LI, Multani PS, Witzig TE, Spies S, Bartlett NL, Schilder RJ, Murray JL, Saleh M, Allen RS, Grillo-Lopez AJ, White CA (2002) Ibritumomab tiuxetan radioimmunotherapy for patients with relapsed or refractory non-Hodgkin lymphoma and mild thrombocytopenia: a phase II multicenter trial. Blood 99: 4336–4342
Wiseman GA, Kornmehl E, Leigh B, Erwin WD, Podoloff DA, Spies S, Sparks RB, Stabin MG, Witzig T, White CA (2003) Radiation dosimetry results and safety correlations from 90Y-ibritumomab tiuxetan radioimmunotherapy for relapsed or refractory non-Hodgkin's lymphoma: combined data from 4 clinical trials. J Nucl Med 44: 465–474
Wiseman GA, Witzig TE (2005) Yttrium-90 (90Y) ibritumomab tiuxetan (Zevalin) induces long-term durable responses in patients with relapsed or refractory B-Cell non-Hodgkin's lymphoma. Cancer Biother Radiopharm 20: 185–188
Witzig TE, Flinn IW, Gordon LI, Emmanouilides C, Czuczman MS, Saleh MN, Cripe L, Wiseman G, Olejnik T, Multani PS, White CA (2002a) Treatment with ibritumomab tiuxetan radioimmunotherapy in patients with rituximab-refractory follicular non-Hodgkin's lymphoma. J Clin Oncol 20: 3262–3269
Witzig TE, Gordon LI, Cabanillas F, Czuczman MS, Emmanouilides C, Joyce R, Pohlman BL, Bartlett NL, Wiseman GA, Padre N, Grillo-Lopez AJ, Multani P, White CA (2002b) Randomized controlled trial of yttrium-90-labeled ibritumomab tiuxetan radioimmunotherapy versus rituximab immunotherapy for patients with relapsed or refractory low-grade, follicular, or transformed B-cell non-Hodgkin's lymphoma. J Clin Oncol 20: 2453–2463
Witzig TE, White CA, Gordon LI, Wiseman GA, Emmanouilides C, Murray JL, Lister J, Multani PS (2003) Safety of yttrium-90 ibritumomab tiuxetan radioimmunotherapy for relapsed low-grade, follicular, or transformed non-hodgkin's lymphoma. J Clin Oncol 21: 1263–1270
Zinzani PL, Pulsoni A, Perrotti A, Soverini S, Zaja F, De RA, Storti S, Lauta VM, Guardigni L, Gentilini P, Tucci A, Molinari AL, Gobbi M, Falini B, Fattori PP, Ciccone F, Alinari L, Martelli M, Pileri S, Tura S, Baccarani M (2004) Fludarabine plus mitoxantrone with and without rituximab versus CHOP with and without rituximab as front-line treatment for patients with follicular lymphoma. J Clin Oncol 22: 2654–2661
Acknowledgements
We thankfully acknowledge support from the Swiss Cancer League No KFS 991-02-2000 and excellent technical and laboratory assistance from the staff of the Departments of Nuclear Medicine and Oncology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Buchegger, F., Antonescu, C., Delaloye, A. et al. Long-term complete responses after 131I-tositumomab therapy for relapsed or refractory indolent non-Hodgkin's lymphoma. Br J Cancer 94, 1770–1776 (2006). https://doi.org/10.1038/sj.bjc.6603166
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603166
Keywords
This article is cited by
-
Tumour targeting and radiation dose of radioimmunotherapy with 90Y-rituximab in CD20+ B-cell lymphoma as predicted by 89Zr-rituximab immuno-PET: impact of preloading with unlabelled rituximab
European Journal of Nuclear Medicine and Molecular Imaging (2015)
-
Challenges and approaches for the development of safer immunomodulatory biologics
Nature Reviews Drug Discovery (2013)
-
Rituximab and new regimens for indolent lymphoma: a brief update from 2012 ASCO Annual Meeting
Cancer Cell International (2012)