Abstract
We investigated relations between measured body mass index (BMI) and stature and thyroid cancer (3046 cases) in a large Norwegian cohort of more than two million individuals. The risk of thyroid cancer, especially of the papillary and follicular types, increased moderately with increasing BMI and height in both sexes.
Similar content being viewed by others
Main
Several types of malignancies have been associated with increased weight, as summarised recently (IARC Working Group on the Evaluation of Cancer-Preventive Strategies, 2002). As thyroid cancer is relatively rare, with only a few studies of its association with obesity, the working group did not include it in its review.
In 1993–1997, thyroid cancer comprised 0.5 and 1.4% of all male and female cancer cases, respectively, in the Nordic countries (Møller et al, 2002). In Norway, the (world) age-adjusted incidence rates in 2004 were 1.5 and 5.1 per 100 000 persons per year in men and women, respectively (The Cancer Registry of Norway, 2006), the higher rates among women being typical (Parkin et al, 2005). In the US, the rates of thyroid cancer are significantly higher and increasing. In 2001, the age-adjusted incidence rates were 4.2 and 12 per 100 000 persons per year in males and females (National Cancer Institute, 2005).
In the present study, we used measurements from Norwegian health surveys to examine the relations between body mass index (BMI) and stature and the risk of thyroid cancer. We have recently published similar analyses for a range of cancers (Engeland et al, 2003a, 2003b and 2003c, 2004, 2005; Bjørge et al, 2004).
Materials and methods
The study population and the methods have been described elsewhere (Bjørge et al, 2004). In a number of Norwegian health surveys during 1963–2001, height and weight were measured in 2 001 727 persons (963 709 men and 1 038 018 women) aged 20–74 years in a standardised way by a trained staff. A major part of the health surveys in the period 1963–1975 was included in a nationwide tuberculosis screening programme (Waaler, 1984), which was compulsory for all Norwegians aged 15 years and above; attendance was about 85%. In 1963–1964 and in 1972–2001, height and weight were also measured in other health surveys connected with coronary heart disease in different parts of Norway (Bjartveit et al, 1979; Bjartveit, 1997). The attendance in these surveys in the mid-1970s was 85–90% and about 75% in the mid-1990s (Bjartveit, 1997).
Deaths, emigrations and cases of thyroid cancer (International Classification of Diseases, seventh revision (ICD-7): 194) in this cohort were identified by linkage to the Death Registry at Statistics Norway (Statistics Norway, 2006) and to the Cancer Registry of Norway (The Cancer Registry of Norway, 2006). Both these registries are population based and cover the entire Norwegian population. A unique 11-digit identification number assigned to all individuals living in Norway after 1960 facilitated the linkages.
The present study included only histologically verified thyroid cancers. Persons with a diagnosis of thyroid cancer before the height and weight measurements were excluded (n=709). In the analyses, the persons in the cohort were followed from the date of measurement until the date of cancer diagnosis, emigration, age 100 years, death or until 31 December 2003. Altogether, 2 001 018 persons were eligible for the study. A small number of these (39 men and 32 women) were lost to follow-up.
Statistical methods
Cox's proportional hazards regression models (Cox and Oakes, 1984), with time since measurement as the time variable, were fitted to obtain relative risk estimates of cancer. In the analyses, categorised variables for age at measurement, year of birth, BMI ((weight in kilograms)/(height in metres)2) and height were included. Body mass index was categorised using the WHO categorisation (World Health Organization Consultation on Obesity, 1998): BMI <18.5 (underweight), 18.5–24.9 (normal), 25.0–29.9 (preobese/overweight) and ⩾30.0 kg/m2 (obese).
Analyses were also performed treating BMI and height, respectively, as continuous variables to test for trend in thyroid cancer risk. Separate analyses were performed for papillary, follicular, medullary, anaplastic, other carcinomas and other malignant tumours. All these analyses were performed with the statistical program package SPSS (SPSS Inc., SPSS for Windows, Release 12.0.2.2004). The results were presented as relative risks (RR) of cancer with 95% confidence intervals (CI). The hazard functions of thyroid cancer by BMI and height in the Cox model were estimated using spline functions in S-plus (Insightful Corporation, 2002), with 4 d.f.
Results
The 2 000 947 persons (963 523 men and 1 037 424 women) included in this study were followed for on average 23 years (maximum 41 years), constituting 47 million person-years (Table 1). The mean age at measurement was 44 years, and the proportions of obesity were 6 and 13% in men and women, respectively. During follow-up, 3046 thyroid cancer cases were diagnosed among the study subjects on average 15 years after the measurements. The mean age at diagnosis was 62.2 and 57.7 years in men and women, respectively.
The risk of thyroid cancer increased moderately by increasing BMI in both sexes (Table 2). The RR of thyroid cancer per unit increase in BMI was 1.03 (95% CI: 1.00–1.05) in men and 1.02 (95% CI: 1.01–1.03) in women. Excluding the first 5 years of follow-up did not change these results. Splitting the upper BMI category in women gave RRs of 1.27 (95% CI: 1.11–1.47), 1.33 (95% CI: 1.03–1.73) and 1.38 (95% CI: 0.83–2.30) with BMI of 30.0–34.9, 35.0–39.9 and 40 or above, respectively, compared with normal-weighted women.
Histology-specific analyses revealed that the relative risk of follicular carcinoma increased more than the risk of papillary carcinoma with increasing BMI. Further, the risk of medullary carcinoma tended to decrease with increasing BMI in both sexes, being significant among females only. The RR of medullary carcinoma per unit increase in BMI was 0.94 (95% CI: 0.85–1.04) in men and 0.91 (95% CI: 0.86–0.97) in women. The number of cases was low (52 and 107 medullary carcinomas in men and women, respectively). The anaplastic carcinomas showed a strong positive association with BMI in men.
The risk of thyroid cancer increased with increasing height in both sexes (Table 2). The RR of thyroid cancer associated with 10 cm increase in height was 1.18 (95% CI: 1.05–1.32) in men and 1.22 (95% CI: 1.13–1.31) in women.
Among males, the elevated risk associated with increased BMI was confined to those measured at the age of 50–74 years (Table 3).
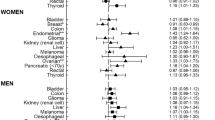
The associations between BMI and stature and the risk of thyroid cancer in women are illustrated in Figure 1. The risk of thyroid cancer increased with increasing height and BMI above 25kg/m2.
Discussion
In this large cohort, including more than two million individuals, we explored the associations between BMI and height and the occurrence of thyroid cancer. The risk was found to be moderately elevated with increasing BMI and height in both sexes among the follicle-cell derived (papillary and follicular) carcinomas. In medullary carcinomas, an opposite trend was present for BMI, pointing to a different pathogenetic influence.
The associations between BMI and height with thyroid cancer have been difficult to explore in previous small studies owing to the low incidence of this disease. In addition to the large size of the present cohort, we also had an almost complete follow-up with regard to thyroid cancer incidence and deaths. This was made possible by linkages to population-based registries of high quality. Only 0.04% of the study cohort (71 persons) was lost to follow-up, and 0.6% was censored by emigration from Norway.
After a pooled analysis of 12 case–control studies, including 2473 cases, Dal Maso et al (2000) previously found a moderately increased risk of thyroid cancer related to height and weight at diagnosis. Dal Maso et al (2000) used self-reported values for height and weight during the late teens and at diagnosis. In the present study, we relied on height and weight measurements performed on average 15 years before the diagnosis of thyroid cancer. Hence, our estimates were not diluted by a possible influence of individuals weight on the disease.
Iribarren et al (2001) evaluated several potential predictors of thyroid cancer in a large American cohort with long follow-up, including more than 200 000 persons. Despite the large size of the cohort and the long follow-up, only 196 thyroid cancers were observed. In this study, no association between BMI, height or weight gain and thyroid cancer was observed.
Dal Maso et al (2000) hypothesised that an association between BMI and thyroid cancer could be owing to a relationship with steroid hormones or other endocrine factors. However, they observed an association between BMI and thyroid cancer of similar magnitude in older and younger women. Also in the present study, there was no difference in the association between BMI and thyroid cancer in older and younger women.
Like Dal Maso et al (2000), we observed a moderately increasing risk of thyroid cancer with increasing height. This association may be owing to dietary influence during childhood or adolescence and possible interactions with growth factors.
In conclusion, the present study showed that the risk of thyroid cancer increased moderately with increasing BMI and height in both males and females.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bjartveit K (1997) [The National Health Screening Service: from fight against tuberculosis to many-sided epidemiological activities] Fra tuberkulosekamp til mangesidig epidemiologisk virksomhet. Nor Epidemiol 7: 157–174
Bjartveit K, Foss OP, Gjervig T, Lund-Larsen PG (1979) The cardiovascular disease study in Norwegian counties. Background and organization. Acta Med Scand Suppl 634: 1–70
Bjørge T, Tretli S, Engeland A (2004) Relation of height and body mass to renal cell carcinoma in two million Norwegian men and women. Am J Epidemiol 160: 1168–1176
Cox DR, Oakes D (1984) Analysis of Survival Data. London: Chapman & Hall Ltd
Dal Maso L, La Vecchia C, Franceschi S, Preston-Martin S, Ron E, Levi F, Mack W, Mark SD, McTiernan A, Kolonel L, Mabuchi K, Jin F, Wingren G, Galanti MR, Hallquist A, Glattre E, Lund E, Linos D, Negri E (2000) A pooled analysis of thyroid cancer studies. V. Anthropometric factors. Cancer Causes Control 11: 137–144
Engeland A, Bjørge T, Selmer RM, Tverdal A (2003a) Height and body mass index in relation to total mortality. Epidemiology 14: 293–299
Engeland A, Tretli S, Austad G, Bjørge T (2005) Height and body mass index in relation to colorectal and gallbladder cancer in two million Norwegian men and women. Cancer Causes Control 16: 987–996
Engeland A, Tretli S, Bjørge T (2003b) Height, body mass index, and ovarian cancer: a follow-up of 1.1 million Norwegian women. J Natl Cancer Inst 95: 1244–1248
Engeland A, Tretli S, Bjørge T (2003c) Height, body mass index, and prostate cancer: a follow-up of 950 000 Norwegian men. Br J Cancer 89: 1237–1242
Engeland A, Tretli S, Bjørge T (2004) Height and body mass index in relation to esophageal cancer; 23-year follow-up of two million Norwegian men and women. Cancer Causes Control 15: 837–843
IARC Working Group on the Evaluation of Cancer-Preventive Strategies (2002) Weight Control and Physical Activity. Lyon: IARC Press International Agency for Research on Cancer
Insightful Corporation (2002) S-plus 6.1 for windows. Insightful Corporation
Iribarren C, Haselkorn T, Tekawa IS, Friedman GD (2001) Cohort study of thyroid cancer in a San Francisco Bay area population. Int J Cancer 93: 745–750
Møller B, Fekjær H, Hakulinen T, Tryggvadóttir L, Storm HH, Tallbäck M, Haldorsen T (2002) Prediction of cancer incidence in the Nordic countries up to the year 2020. Eur J Cancer Prev 11 (Suppl 1): S1–S96
National Cancer Institute (2005) SEER Cancer Statistics Review, 1975–2001, http://seer.cancer.gov/csr/1975_2001/ Ries LAG, Eisner MP, Kosary CL, Hankey BF, Miller AB, Clegg L, Mariotto A, Feuer EJ, and Edwards BK (ed) March 2005, National Cancer Institute
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55: 74–108
Statistics Norway (2006) Statistics Norway. http://www.ssb.no/english/ April 2006
The Cancer Registry of Norway (2006) The Cancer Registry of Norway. http://www.kreftregisteret.no/ April 2006
Waaler HT (1984) Height, weight and mortality. The Norwegian experiment. Acta Med Scand 679 (Suppl): 1–56
World Health Organization Consultation on Obesity (1998) Preventing and managing the global epidemic: Report of a WHO Consultation on Obesity, Geneva, 3–5 June 1997, pp 1–276. 1998. Geneva, Switzerland: World Health Organization
Acknowledgements
We are grateful to those who for almost 40 years collected the data used in the present study. These people were connected to the former National Health Screening Service, The Nord-Trøndelag Health Survey (HUNT), The Hordaland Health Survey (HUSK) and The Tromsø Study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Engeland, A., Tretli, S., Akslen, L. et al. Body size and thyroid cancer in two million Norwegian men and women. Br J Cancer 95, 366–370 (2006). https://doi.org/10.1038/sj.bjc.6603249
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603249
Keywords
This article is cited by
-
Clinicopathological profile and management of thyroid carcinoma: a Sub-Saharan country experience
Thyroid Research (2023)
-
Potential impact of obesity on the aggressiveness of low- to intermediate-risk papillary thyroid carcinoma: results from a MASTER cohort study
Endocrine (2023)
-
Association of BMI with Clinicopathological Features of Papillary Thyroid Cancer: A Systematic Review and Meta‐Analysis
World Journal of Surgery (2021)
-
Tumour biology of obesity-related cancers: understanding the molecular concept for better diagnosis and treatment
Tumor Biology (2016)
-
Height and Risk of Adult Cancers: a Review
Current Epidemiology Reports (2016)