Abstract
Introduction:
This paper reports on an ongoing primary care audit of cancer referrals undertaken in Scotland in 2006–2007 and 2007–2008.
Methods:
General practitioners (GPs) in Scotland were asked to review all new cancer diagnoses within their practice during the preceding year.
Results:
4181 patients were identified in year 1 and 12 294 in year 2. The pathway taken for patients to present to, and be referred from, their GP has been analysed for 7430 of the 12 294 patients identified within year 2 across five separate health boards. The time from first symptoms to presentation to a GP varied between tumour types, being the longest (median 30 days) for head and neck cancers and the shortest (median 2 days) for bladder cancer. In all, 25% of patients within the following tumour groups waited longer than 2 months to present to their GP following first symptoms: prostate, colorectal, melanoma and head and neck cancers. Once patients had presented to their GP, those with prostate and lung cancer were referred later (median time 11 days) than those with breast cancer (median time 2 days). The priority with which GPs referred patients varied considerably between tumour groups (breast cancer 77.5% ‘urgent’ compared with prostate cancer 44.7% ‘urgent’). In one health board the proportion of cancer patients being referred urgently increased from 46% to 58% between the first and second audit.
Conclusion:
Our data show that there are very different patterns of presentation and referral for patients with cancer, with some tumour groups being more likely to be associated with a delayed diagnosis than others.
Similar content being viewed by others
Main
Early presentation, prompt investigation and timely access to definitive treatment unquestionably improves the experience of patients, although there is some doubt about when and whether delays affect outcomes with many cancers (Richards et al, 1999; Jensen et al, 2007; Neal et al, 2007; Chen et al, 2008; Hamilton, 2009).
Different countries have different systems for allowing access to specialist services. In the United Kingdom, other than diagnoses made through the three screening services (breast, cervical and more recently, colorectal cancers), patients usually first present to their general practitioners (GPs). GPs have an important function in assessing which patterns of symptoms are most likely to be suggestive of cancer. If cancer is suspected, patients may be referred immediately on first presentation for specialist assessment and investigations, or they may have initial investigations and review within primary care and then be referred when the results of tests are available.
Specific guidelines have been developed in Scotland and elsewhere to support GPs in referral decisions for patients with suspected cancer (National Institute for Health and Clinical Excellence, 2005; Scottish Executive Health Department (SEHD), 2007; Scottish Government, 2009).
Targets have been introduced in an attempt to ensure that patients suspected of having cancer are seen and investigated promptly, then fast-tracked for definitive treatment to cure or palliate their cancer. In both England (Secretary of State for Health, 1997) and Scotland (SEHD, 2001), there is a 62-day target from referral to treatment for patients whose referral is marked urgent and for those referred as an emergency (including self-referral to accident and emergency departments). In England (but not in Scotland), there is also a 2-week target from urgent referral to first assessment by specialist services (Secretary of State for Health, 1997).
The aim of this study is to gain a better understanding of how quickly patients with cancer initially present to their GP, and how they are then referred to secondary care for further investigation and treatment.
Materials and methods
On two separate occasions between 2005 and 2008, GPs in most health boards in Scotland were asked to review all new cancer diagnoses within their practice during the preceding year. It was hoped that by engaging practices in a cancer-review process, it would be possible to consolidate knowledge around the early parts of the cancer journey including typical presentation of cancers, symptom development and when and how to refer for further investigation. The first audit took place in 2006–2007 and involved reviewing all patients diagnosed with cancer in 2005–2006; the second took place in 2007–2008, relating to patients diagnosed in 2006–2007. Engagement with the study was facilitated by the enhanced service component of the General Medical Services Contract, which enabled a payment for participating practices.
Participating GPs across Scotland were asked to review the clinical notes of each new patient diagnosed with cancer and were given guidance regarding how to record the items listed in Table 1 onto a standard electronic template. They were then asked to reflect on the patient journey and to comment on ways that it could have been improved. Patients with cancer detected through the national screening programmes were excluded from the study, as were those with non-melanoma skin cancer.
Data were available from five health boards across Scotland during the first review, and from nine health boards during the second (Scotland is served by 11 mainland and three island health boards), and work is currently underway to amalgamate these data across the whole of Scotland. The results in this paper relate to the initial analysis of the second year's data, taken from five of the nine participating health boards. Comparative data from one health board relating to priority of referral over the two separate years of the audit have also been included.
Results
In all, 4181 patients were identified with a new diagnosis of cancer during year 1 and 12 294 in year 2. This compares with a total of ∼27 000 new cases of cancer diagnosed each year in Scotland (Information Services Division, 2008). In the first year of the audit, each health board collected data in different ways, making collation difficult. Arrangements in year 2 were more systematic, allowing data to be collected on 12 294 patients with cancer. Detailed analysis has been conducted on data for 7430 of the 12 294 patients. Data on the remaining 4864 patients are not yet analysed.
The 7430 cases analysed were identified by 540 GP practices from five different health boards in Scotland. The cases covered all major tumour types (Figure 1; Table 2) and reflected a similar pattern to that reported nationally (Information Services Division, 2008).
This paper focuses on the analysis of the following:
-
a)
time from patient first noticing symptoms to first presentation with a GP,
-
b)
time from first presentation to time of referral,
-
c)
priority of referral from primary to secondary care.
Time from patient first noticing symptoms to first presentation with a GP
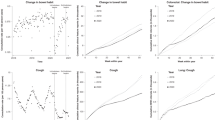
The time taken for patients to present to a GP varied according to tumour site (Figure 2; Table 3). Patients with head and neck cancer took the longest to present (median time 30 days). Patients with melanoma (median time 26 days) and colorectal cancer (median time 21 days) also presented comparatively late. In all, 25% of patients with the following cancers waited longer than 1 month before first presenting: breast, lung, lymphoma, ovarian and upper gastrointestinal. For prostate, colorectal, melanoma, and head and neck cancers, the same proportion of patients, 25%, waited 2 months or more to first present to a GP.
The shortest times between first noticing a sign or symptom and first presentation to a GP were for patients with bladder cancer (median time 2 days), leukaemia (4 days), cervical cancer (6.5 days) and breast cancer (7 days).
Time from first presentation to time of referral
The time taken for a GP to refer a patient with a suspicion of cancer also varied according to tumour group (Figure 3; Table 4). Patients with breast cancer and melanoma were referred quickly (median times 1 day and 2 days, respectively), whereas for other tumour groups (notably lung and prostate), patients spent much longer within the primary care part of the journey before being referred to secondary care (lung cancer 11 days, prostate cancer 11 days). In all, 25% of patients with lung cancer and upper gastrointestinal cancer were not referred for 1 month or more following initial presentation.
Priority of referral from primary to secondary care
One of the most important factors determining time to diagnosis was the priority with which the GP sent the referral. When the referral priority was examined for the four most common cancers (Figure 4; Table 5), a much higher proportion of patients with breast cancer (969; 77.5%) and lung cancer (694; 70.7%) were referred ‘urgently’ to secondary care compared with colorectal cancer (543; 50.6%) and prostate cancer (391; 44.7%). Patients with colorectal and lung cancer were more likely than prostate or breast cancer patients to present as an emergency admission, and of these four tumour groups, patients with prostate cancer had the highest likelihood of being referred to hospital ‘routinely’ (337; 38.6%). The category ‘other’ included referrals that were marked as ‘soon’ and referrals to private hospitals or clinics.
When referral priority data were compared within one of the five health boards over the two separate time periods (following an intensive GP education programme), the proportion of all cancers presenting to GPs that were referred ‘urgently’ increased from 340 out of 739 referrals (46%) in 2005–2006 to 545 out of 940 referrals (58%) in 2006–2007 (Figure 5). The difference in the total number of cancers diagnosed from year 1 to year 2 is accounted for by a slight increase in the number of GP practices taking part in the audit during the second year.
The extent to which the priority of referral contributed to delays in diagnosis was evident when the time to first see a hospital specialist was examined. When the four commonest tumour groups were examined, the time taken to see a specialist was considerably longer if the patient was referred routinely (Figure 6; Table 6). The median time for a patient with lung cancer to see a specialist was 11 days for an urgent referral, yet 28 days for a routine referral.
Discussion
This study has yielded valuable information about the primary care pathway for over 16 000 patients diagnosed with cancer in Scotland over two separate periods. Detailed analysis of 7430 patients from five separate health boards has been reported in this paper. This has highlighted differences in the way that individual cancers present to, and are referred by, GPs.
Patients with head and neck cancers, melanomas and colorectal cancers waited comparatively longer before seeking help from their GP. When the inter-quartile ranges were examined, it is apparent that 25% patients with prostate cancer, colorectal cancer, melanoma and head and neck cancers took longer than 2 months to present to a GP following the first symptom or sign of cancer. Limited research has been done on what causes patients to delay presenting for advice or referral (Ramirez et al, 1999; Burgess et al, 2001), but it is clear that many patients are not aware of the common symptoms and signs that might suggest a diagnosis of cancer. Although there have been occasional public education and other campaigns to raise awareness and encourage early presentation, there is little objective measurement of their effectiveness. A recent study examined attempts to positively influence and subsequently evaluate interventions to encourage early presentation of women with breast cancer (Burgess et al, 2009).
GPs can influence the time from first presentation to referral. The delay in referral for both lung and prostate cancer patients can be explained by recommendations that initial assessments and investigations be completed before referral (e.g. chest X-ray in suspected lung cancer and evaluation of prostate-specific antigen in prostate cancer) (SEHD, 2007).
For some tumour groups, less than half of all newly diagnosed cancers were referred urgently. Of the four commonest tumour groups, marked differences were noted between the proportions of breast cancer patients referred urgently (969; 77.5%) compared with colorectal (543; 50.6%) and prostate cancer patients (391; 44.7%).
The importance of referring a patient with cancer ‘urgently’ is that these patients are actively ‘fast-tracked’ through the hospital diagnostic system to ensure compliance with the 62-day target from urgent referral to treatment (SEHD, 2001). As ‘routine’ and ‘soon’ referrals are not subject to these targets, they are not prioritised and invariably take much longer to start treatment following the date of referral.
With this audit, GPs were given the opportunity to comment on each individual patient's pathway to diagnosis. On reflection, many GPs indicated that they should have referred their patient more urgently than they did; however, the most common explanation from GPs was that the patient did not have the classic symptoms and signs described within the urgent cancer referral guidelines. Referral guidelines for some tumours may not always favour patients with early symptoms of cancer. One study (Neal et al, 2007) found that for lung cancer (a tumour with a poor prognosis), referral guidelines were prioritising those with more advanced disease. However, the same was not found for patients with colorectal, ovarian or prostate cancer.
Despite doubt about the benefit of urgent referral pathways, one encouraging finding was the change in the proportion of patients referred urgently within one health board during the two separate years of the study. This change was also noted within several different health boards and may reflect increasing awareness of guidelines on the part of referrers and the increased priority that cancer has been given in Scotland in recent years. Data are awaited from a further audit (again through the enhanced service component of the General Medical Services Contract) to examine the compliance of all urgent suspected cancer referrals with current referral guidelines.
By engaging with 540 different GP practices across five health boards, there is a risk of variable data capture depending on the thoroughness with which individual GPs reviewed their clinical notes. The development of clear guidance for data collection and the rigorous checking of all data submitted will have helped to reduce this variability. However, by engaging with GPs across Scotland in the collection of these data, it has been possible to facilitate education around the typical presentation of cancer. Comments written by GPs undertaking this audit provide a wealth of information. Individual practices were frequently very open about their shortcomings and appeared to provide perceptive analysis of the diagnostic journey. Significant event analysis has become an embedded part of reflective learning by GPs and forms a component of the annual appraisal system. Data from this audit facilitated significant event analyses within many of the GP practices taking part.
Although doubt has been cast on the benefit of cancer waiting time targets, whether 2-week waits or 62-day targets (Jones et al, 2001), and some have shown a perverse adverse effect on breast cancer referrals (Potter et al, 2007), public opinion and published evidence supports the benefit of prompt recognition, prompt referral and early effective treatment for patients with cancer. Primary care health professionals have an important function in early diagnosis.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Burgess C, Hunter MS, Ramirez AJ (2001) A qualitative study of delay among women reporting symptoms of breast cancer. Br J Gen Pract 51: 967–971
Burgess C, Linsell L, Kapari M, Omar L, Mitchell M, Whelehan P, Richards MA, Ramirez AJ (2009) Promoting early presentation of breast cancer by older women: a preliminary evaluation of a one-to-one health professional-delivered intervention. J Psychosom Res 67: 377–385
Chen Z, King W, Pearcey R, Kerba M, Mackillop WJ (2008) The relationship between waiting time for radiotherapy and clinical outcomes: a systematic review of the literature. Radiother Oncol 87: 3–16
Hamilton W (2009) Five misconceptions in cancer diagnosis. Br J Gen Pract 59: 441–447
Information Services Division. NHS National Services Division (2008) Cancer in Scotland. ISD: Edinburgh
Jensen AR, Nellemann HM, Overgaard J (2007) Tumour progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol 84: 5–10
Jones R, Rubin G, Hungin P (2001) Is the two week rule for cancer referrals working? BMJ 322: 1555–1556
National Institute for Health and Clinical Excellence (2005) Referral Guidelines for Suspected Cancer. NICE: London
Neal RD, Allgar VL, Ali N, Leese B, Heywood P, Proctor G, Evans J (2007) Stage, survival and delay in lung, colorectal, prostate and ovarian cancer: comparison between diagnostic routes. Br J Gen Pract 57: 212–219
Potter S, Govindarajulu S, Shere M, Braddon F, Curran G, Greenwood R, Sahu AK, Cawthorn SJ (2007) Referral patterns, cancer diagnoses, and waiting times after introduction of two week wait rule for breast cancer: prospective cohort study. BMJ 335: 288–290
Ramirez AJ, Westcombe A, Burgess CC, Sutton S, Littlejohns P, Richards MA (1999) Factors predicting delayed presentation of symptomatic breast cancer: a systematic review. Lancet 353: 1127–1131
Richards MA, Westcombe A, Love SB, Littlejohns P, Ramirez AJ (1999) Influence of delay on survival in patients with breast cancer: a systematic review. Lancet 353: 1119–1126
Scottish Executive Health Department (2001) Cancer in Scotland: Action for Change. SEHD: Edinburgh
Scottish Executive Health Department (2007) Scottish Referral Guidelines for Suspected Cancer. SEHD: Edinburgh
Scottish Government (2009) Scottish Referral Guidelines for Suspected Cancer. Quick Reference Guide. Scottish Government: Edinburgh
Secretary of State for Health (1997) The New NHS, Modern, Dependable. Stationery Office: London
Acknowledgements
We are grateful to GP colleagues who conducted the audit and specifically members of the Scottish Primary Care Cancer Group who supported the process and to Jennifer Keatings, Information Officer, West of Scotland Managed Clinical Network for Cancer for help in the collation and analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Baughan, P., O'Neill, B. & Fletcher, E. Auditing the diagnosis of cancer in primary care: the experience in Scotland. Br J Cancer 101 (Suppl 2), S87–S91 (2009). https://doi.org/10.1038/sj.bjc.6605397
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605397
Keywords
This article is cited by
-
Explaining time elapsed prior to cancer diagnosis: patients’ perspectives
BMC Health Services Research (2017)
-
Knowledge or noise? Making sense of General Practitioners’ and Consultant use of 2-week-wait referrals for suspected cancer
British Journal of Cancer (2017)
-
Primary care characteristics and stage of cancer at diagnosis using data from the national cancer registration service, quality outcomes framework and general practice information
BMC Cancer (2015)
-
The relative length of the patient and the primary care interval in patients with 28 common and rarer cancers
British Journal of Cancer (2015)
-
Assessing the impact of an English national initiative for early cancer diagnosis in primary care
British Journal of Cancer (2015)