Abstract
Background:
Radiotherapy for breast cancer reduces disease recurrence and breast cancer mortality. However, it has also been associated with increased second cancer risks in exposed sites.
Methods:
We evaluated long-term second cancer risks among 182 057 5-year survivors of locoregional invasive breast cancer diagnosed between 1973 and 2000 and reported to US NCI-SEER Program cancer registries. Multivariate Poisson regression was used to estimate the relative risk (RR) and excess cases of second cancer in women who had surgery and radiotherapy, compared with those who had surgery alone. Second cancer sites were grouped according to doses received from typical tangential breast fields.
Results:
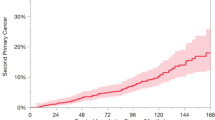
By the end of 2005 (median follow-up=13.0 years), 15 498 second solid cancers had occurred, including 6491 contralateral breast cancers. The RRs for radiotherapy were 1.45 (95% confidence interval (CI)=1.33–1.58) for high-dose second cancer sites (1+ Gy: lung, oesophagus, pleura, bone and soft tissue) and 1.09 (1.04–1.15) for contralateral breast cancer (≈1 Gy). These risks decreased with increasing age and year of treatment. There was no evidence of elevated risks for sites receiving medium (0.5–0.99 Gy, RR=0.89 (0.74–1.06)) or low doses (<0.5 Gy, RR=1.01 (0.95–1.07)). The estimated excess cases of cancer in women treated with radiotherapy were as follows: 176 (95% CI=69–284) contralateral breast cancers or 5% (2–8%) of the total in all 1+year survivors, and 292 (222–362) other solid cancers or 6% (4–7%) of the total.
Conclusions:
Most second solid cancers in breast cancer survivors are not related to radiotherapy.
Similar content being viewed by others
Main
Substantial improvements in breast cancer treatment and screening signify that nearly 90% of women diagnosed with breast cancer survive for >5 years (Berry et al, 2005; Ries et al, 2008). Currently, an estimated 2.5 million breast cancer survivors live in the United States (Ries et al, 2008), and the long-term health of these women is an important public health issue. A recent descriptive analysis of Surveillance Epidemiology and End Results Program (SEER) cancer registries found that breast cancer survivors have an 18% higher risk of developing a subsequent cancer compared with the general population (Curtis et al, 2006). Shared environmental and genetic factors are likely to be involved, but some of the increased risk is probably a late adverse effect from the cancer treatments such as radiotherapy (Clarke et al, 2005). Randomised trials and cancer registry-based studies have shown that radiotherapy significantly reduces the risk of recurrence and breast cancer mortality, and also increases the risk of second cancers of the lung, oesophagus, soft tissue, contralateral breast and leukaemia (Huang and Mackillop, 2001; Gao et al, 2003; Zablotska and Neugut, 2003; Clarke et al, 2005; Zablotska et al, 2005).
Surveillance Epidemiology and End Results Program registries cover the largest population of any national cancer registries and contain information on radiotherapy treatment, tumour characteristics and have long-term follow-up. In this study, we performed the first systematic evaluation of all second solid cancer risks after radiotherapy treatment for invasive breast cancer in the United States using the SEER databases. The large sample size and long-term follow-up enabled evaluation of patterns of effect modification, estimation of the number of excess cases and the proportion of second solid cancers occurring among breast cancer survivors that might be attributable to radiotherapy.
Materials and methods
Population and follow-up
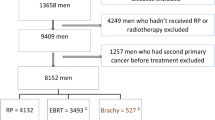
The cohort was composed of women who were diagnosed with a first primary invasive locoregional breast cancer reported to one of the nine SEER registries between 1 January 1973 and 31 December 2000 (n=328 691). As there is at least a 5-year lag period between radiation exposure and solid cancer induction (BEIR VII, 2005), we excluded 103 235 women who did not survive for 5 years. The follow-up time for second cancers began 5 years after the date of initial cancer diagnosis and ended at the date of diagnosis of second primary cancer, at last known vital status, death or at the end of the study (31 December 2005), whichever occurred first. As underreporting of second cancers has been noted to occur among elderly patients who frequently have other comorbid conditions (Fraumeni et al, 2006), we excluded women whose first breast cancer was diagnosed after the age of 75 years (n=33 214) and restricted follow-up to attained ages <80 years. We also excluded women if it was unknown whether they had received radiotherapy (n=352), chemotherapy (n=1273) or hormonal therapy (n=1304); women who did not have breast cancer surgery or if surgery was unknown (n=4848) and women who had distant metastases at diagnosis or unknown disease stage (n=7853). As a number of women were missing more than one piece of information, the final cohort included 182 057 women.
Treatment information
Women were classified according to whether they had received radiotherapy as part of their initial breast cancer treatment. Surgery was classified as mastectomy (total, modified radical, extended radical mastectomy) or breast-conserving surgery (partial mastectomy, lumpectomy, wedge resection, quadrantectomy, segmental mastectomy, tylectomy, subcutaneous mastectomy). Before 1983, the type of surgery performed was not available in SEER, but as breast-conserving surgery was rare, surgery before this date was assumed to have been mastectomy. The effects of chemotherapy and hormonal therapy were not assessed directly because of concerns regarding underascertainment in SEER (Brown et al, 2000), but the relative risks (RRs) for radiotherapy were adjusted for chemotherapy and hormonal therapy treatment.
We grouped second cancer sites a priori into three dose groups according to the estimated mean organ dose from the basic breast cancer radiotherapy treatment involving tangential fields: high (1+ Gy), medium (0.5–0.99 Gy) and low (<0.5 Gy) dose. This dosimetry was conducted using thermoluminscent dosimeters in tissue equivalent phantoms assuming a standard treatment protocol with 50 Gy tumour dose and beam energy of 6 MV photons (Appendix A) (Stovall et al, 2006; Stovall et al, 2008). Ipsilateral second breast cancers were excluded because of the difficulty in distinguishing between recurrence and subsequent primary cancer.
Statistical analysis
The observed (O) number of second cancers for each site was compared with the expected (E) number in women in the general population. The expected number of second cancers was estimated by multiplying age-, sex-, race- and calendar-period-specific cancer incidence rates in the nine SEER registries by stratum-specific person-years at risk and then summing across strata (Seer*stat, version 6.4.4). Standardised incidence ratios (SIRs) were calculated by dividing the observed number of cancers (O) by the expected number (E). Tests of statistical significance were two sided and were based on Poisson exact methods (Liddell, 1984).
Multivariate Poisson regression analysis (using Epicure, 2007) was used to estimate the RR (and 95% confidence intervals (CI)) for the groups of second solid cancers (defined above according to dose) after radiotherapy and surgery compared with surgery alone, with the expected number of second cancers used as an offset. If Or and Er indicate the number of observed and expected cancers, respectively, in the surgery+radiotherapy (r=1) and surgery alone (r=0) groups, then the statistical expectation of Or is given by

where θ and β are parameters to be estimated and 1+β is the RR associated with radiotherapy. The use of the expected number of cancers as an offset indirectly adjusts for potential confounding by attained age and attained calendar period (Yasui et al, 2003). Analyses were additionally adjusted for breast cancer stage, age at and year of breast cancer diagnosis, chemotherapy and hormonal therapy treatment (yes/no) through stratification. Trend tests were conducted using ordinal categories as continuous variables.
We investigated potential effect modifiers by stratification, including age at, year of and time since first cancer diagnosis, as well as stage and type of surgery (breast-conserving vs mastectomy). As the majority of women who receive breast-conserving surgery are recommended to receive radiotherapy, the proportion of women who had this type of surgery without radiotherapy in SEER was relatively small (17%), and this subgroup is unlikely to be a representative subset of breast cancer patients. Therefore, to obtain stable risk estimates in subgroup analyses according to surgery type, we used a combined surgery-only comparison group that included both breast-conserving surgery and mastectomy patients. Tests for heterogeneity between surgery types took account of the lack of independence of the comparison group (Berrington and Cox, 2003).
The number of excess cancers related to radiotherapy was estimated as the number of cases in those treated with radiotherapy minus the estimated number of cases that would have occurred in these women if they had not received radiotherapy. The proportion of second cancers attributable to radiotherapy was estimated by dividing this excess by the total number of second cancers in both 1+ and 5+ year survivors. Although it is unlikely that there are any radiation-related cancers before 5 years, the attributable risk among all survivors (defined here as 1+ years) is the most relevant summary statistic for all breast cancer survivors. The excess absolute risk (per 10 000 person-years) was estimated by dividing the excess by the associated number of person-years.
Results
Overall, 38% of women with breast cancer had surgery+radiotherapy and 62% were treated with surgery alone (Table 1). Radiotherapy was slightly less common in those who were older at diagnosis, was increasingly common over time and was more frequent in those who received breast-conserving surgery. Within categories of surgery type, stage was related to treatment with radiotherapy, particularly after mastectomy, in which radiotherapy was more common after regional than after localised disease (27 vs 8%).
The women were followed up for an average of 13 years. During the follow-up period (1978–2005), a total of 15 498 women developed a second primary solid cancer, including 6491 contralateral breast cancers (Table 2). Women treated with surgery+radiotherapy had a higher risk of several second solid cancers compared with the general female population, with more than two-fold SIRs observed for oesophageal, pleural, bone, soft tissue and contralateral breast cancer. These sites typically receive doses from radiotherapy of 1 Gy or more (Appendix A). The adjusted RRs for surgery+radiotherapy, compared with surgery alone, were 1.09 (1.04–1.15) for contralateral breast cancer, 1.45 (95% CI=1.33–1.58) for high-dose, 0.89 (0.74–1.06) for medium-dose and 1.01 (0.95–1.07) for low-dose sites.
For sites in the high-dose group, the RR for surgery+radiotherapy, compared with surgery alone, decreased with increasing age at treatment (P-trend<0.001) and with increasing year of treatment (P-trend=0.01), but increased with increasing time since diagnosis (P-trend<0.001) (Table 3). For patients diagnosed with breast cancer in 1983 or later, the risks were higher after mastectomy (RR=1.50, 95% CI=1.22–1.82) than after breast-conserving surgery (RR=1.28, 95% CI=1.14–1.43), but the difference was not statistically significant (P>0.5).
We further examined the risks for specific sites within the high-dose group that had the largest number of cases: lung, oesophagus and soft tissue. The RR of lung cancer was significantly increased (RR=1.38 (95% CI=1.26–1.51)) and was higher for ipsilateral than for contralateral lung cancer (1.54 (1.36–1.75) vs 1.18 (1.02–1.35)). For patients diagnosed with breast cancer in 1983 or later, lung cancer risk was higher after mastectomy (RR=1.43 (95% CI=1.15–1.77)) than after breast-conserving surgery, but was still significantly elevated (RR=1.20 (1.07–1.36)). For oesophageal cancers, the RR was 1.99 (1.37–2.88), and there was no difference according to surgery type. Overall, the risk for soft tissue cancers was 2.52 (1.67–3.81), but it was especially highly elevated for angiosarcomas (RR=13.7 (4.0–95.6)). The majority of angiosarcomas diagnosed in women who had surgery+radiotherapy were located in the thorax (n=12 out of 16).
The RR for contralateral breast cancer in women who had surgery+radiotherapy, compared with those who had surgery alone, decreased with increasing age at first breast cancer treatment (P-trend=0.03, Table 4). The RR was lower for cancers treated after 1993 (P-trend=0.02), but was not clearly associated with time since treatment, stage or type of surgery.
In total, there were an estimated 176 (95% CI=69–284) excess cases of contralateral breast cancer in women who had surgery+radiotherapy, or 5% (95%CI=2–7%) of the contralateral breast cancers diagnosed in 1 year survivors (Table 5). The excess absolute risk of contralateral breast cancer associated with radiotherapy was 2 (1–4) cases per 10 000 person-years. There were an estimated 292 (95% CI=222–362) excess cases of solid cancers (other than contralateral breast cancer) in women who had radiotherapy, or 6% (3–8%) of the total in 1 year survivors (Table 5). The excess was largely composed of cancers of the lung (∼80%). The excess absolute risk for these cancers associated with radiotherapy was 4 (3–5) cases per 10 000 person-years. When considering only 5+year survivors, the attributable risk estimates were slightly higher: 8% (3–14%) for contralateral breast cancer and 10% (5–14%) for other solid cancers.
Discussion
In this large long-term study of breast cancer survivors, significantly increased RRs of second solid cancers after radiotherapy were observed for the group of sites that typically receive the highest radiation exposure (⩾1 Gy). There was no overall excess risk for the group of sites that typically receive lower radiation exposures (<1 Gy). In total, it was estimated that about 5% (95% CI=2–7%) of contralateral breast cancers and 6% (3–8%) of other solid cancers occurring among 1+year survivors could be related to radiotherapy. Risks were generally lower for more recent treatment periods and higher for younger ages at treatment.
To our knowledge, this is the first study to assess and quantify the long-term risk of all solid cancers after breast cancer radiotherapy in the United States. Our site-specific results were broadly similar to those from a pooled analysis of 63 randomised clinical trials of breast cancer radiotherapy (Clarke et al, 2005) and several observational studies. In these studies, there was evidence of increased risks of lung (Zablotska and Neugut, 2003; Roychoudhuri et al, 2004; Clarke et al, 2005; Darby et al, 2005; Andersson et al, 2008; Schaapveld et al, 2008), oesophageal (Zablotska and Neugut, 2003; Roychoudhuri et al, 2004; Clarke et al, 2005) and contralateral breast cancer (Gao et al, 2003; Roychoudhuri et al, 2004; Clarke et al, 2005), as well as soft tissue sarcomas (Huang and Mackillop, 2001; Clarke et al, 2005; Andersson et al, 2008), in women treated with radiotherapy compared with unirradiated women. In the pooled analysis of clinical trials (Clarke et al, 2005), the authors did not estimate attributable risks, but it was possible to estimate them on the basis of the data presented. Overall, about 8% of total cancers were attributable to radiotherapy, slightly higher than the estimate from this study.
Our results suggested that, in general, radiation-related risks were lower among women treated in more recent years (1993+). This is likely the result of several factors, including reduced volume of irradiated tissues such as the lung, since the introduction of computed tomography planning (Muren et al, 2002; Wang and Harris, 2004; Van der Laan et al, 2008), and also because of shorter available follow-up time. Another factor that probably contributed to this trend was the increasing use of breast-conserving surgery. Although detailed treatment information was not available in SEER, women who received mastectomy probably received supraclavicular, and possibly also internal mammary irradiation, more often than women who had breast-conserving surgery, which would increase doses (Appendix A). In an earlier analysis of lung cancer risk after breast cancer radiotherapy in the SEER registries, it was suggested that there was no increased risk of lung cancer in women who had breast-conserving surgery (Zablotska et al, 2005). We used a combined comparison group of women who had surgery only (mastectomy or breast-conserving surgery) in the current analysis to obtain a broader, more representative referent group of women not treated with radiotherapy. Using this approach, there was evidence of a small, but significantly increased, risk of lung cancer and other cancers in high-dose regions after breast-conserving surgery. In terms of absolute numbers and fatality, lung cancer is by far the most important second cancer after breast cancer, hence it remains important to continue to monitor lung cancer risks after current radiation treatment protocols, taking into account smoking history (Prochazka et al, 2005; Kaufman et al, 2008).
Three earlier studies with individual dosimetry have reported an increased risk of contralateral breast cancer after radiotherapy in the youngest patients (<age 45) (Boice et al, 1992; Hooning et al, 2008; Stovall et al, 2008). This is consistent with the well-established modifying effects of age at radiation exposure; risk decreases with increasing age at exposure and is particularly low in post-menopausal women (Preston et al, 2002). This study and two earlier investigations (including the pooled analysis of clinical trials; Gao et al, 2003; Clarke et al, 2005) found an elevated risk of contralateral breast cancer after radiotherapy following young age at exposure, and also among post-menopausal women. Given the large number of post-menopausal breast cancer patients treated with radiotherapy, this is another question that warrants further study. Although we found no difference in contralateral breast cancer risk in women who had radiotherapy after mastectomy compared with those who underwent breast-conserving surgery, a recent Dutch study reported lower risks after mastectomy (Hooning et al, 2008). However, the majority of women in the Dutch study who had mastectomy were treated with electrons rather than with photons, which should result in a lower radiation dose to the contralateral breast (Stovall et al, 2008) and is the most likely explanation for the difference in findings.
There are several limitations in the use of SEER cancer registries to evaluate treatment-related second cancer risks. One limitation is the potential for loss to follow-up if a patient moves from the registry area, which would result in an underestimation of the absolute number of second cancers and hence the excess absolute risk estimates. However, mortality data are complete and comparisons of our results for lung cancer incidence with an earlier study of these women evaluating lung cancer mortality produced similar results, suggesting that this bias is likely to be small (Darby et al, 2005). Furthermore, the estimated attributable fraction should be valid, unless loss to follow-up is greater in one treatment group than in the other. Radiotherapy may be underreported in SEER because only information pertaining to the initial treatment course is collected (Malin et al, 2002). Since type of surgery was only recorded in SEER after 1983, we assumed that all breast cancer surgery before that time was mastectomy. This assumption undoubtedly resulted in misclassification, which most likely reduced the RR in the mastectomy group. Lack of individual data on actual treatment fields used also meant that we had to use general dose groupings based on typical organ doses from basic treatment fields. Even though individual organ doses would vary if additional fields were used, we think that it is unlikely that the rank order of organs, and hence our dose groupings, would change significantly. This can be observed in Appendix A for the use of tangential fields+supraclavicular fields.
As radiation treatment was not randomised, selection bias could result in differences between treatment groups with regard to smoking status and other variables that affect second cancer risk. Information on other potential confounding factors such as smoking is usually not available in cancer registry studies. The patterns of risk we observed were consistent with the general literature on radiation carcinogenesis, in that risks were higher for sites that should have received higher doses and also higher for younger ages at exposure (Preston et al, 2007). Furthermore, our findings were similar to the results from randomised clinical trials (Deutsch et al, 2003; Clarke et al, 2005), suggesting that any residual confounding is unlikely to have been substantial. If anything, residual confounding by smoking may have resulted in an underestimation of risks if smokers were less likely to receive radiotherapy than non-smokers.
The strengths of this study include the large size of the population-based cohort and long-term follow-up, which enabled the evaluation of relatively small RRs. We also conducted multivariate analyses to ensure that we controlled for the available confounding factors, including other breast cancer treatments and stage. This, plus the assessment of all second solid cancer sites in a single study, enabled the examination of effect modification by age and year of diagnosis, as well as estimation of the excess number and attributable proportion of second cancers that could be related to radiotherapy.
Most of the women in this study were treated in the past (<1990), and breast cancer treatment and radiotherapy techniques have changed considerably over the past three decades (Shank et al, 2000; Taylor et al, 2007). Indeed, our estimates of RRs were lower in those treated in more recent calendar years, and thus the combined results may overestimate risks for current treatment.
Overall, 5–6% of second solid cancers in irradiated women were estimated to be attributable to radiotherapy exposure. Among all breast cancer survivors, this figure was 3%. Our findings suggest that most second solid cancers after treatment for breast cancer are related to other risk factors such as lifestyle or genetic factors. When women and their physicians make treatment decisions, the risk of radiotherapy-related cancer needs to be placed in perspective and balanced with the known tumour control and mortality benefits achieved from treatment.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Andersson M, Jensen MB, Engholm G, Storm H (2008) Risk of second primary cancer among patients with early operable breast cancer registered or randomised in Danish Breast Cancer cooperative Group (DBCG) protocols of the 77, 82 and 89 programmes during 1977–2001. Acta Oncol 47: 755–764
Berrington A, Cox DR (2003) Generalized least squares for the synthesis of correlated information. Biostatistics 4: 423–431
Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Mandelblatt JS, Yakovlev AY, Habbema JD, Feuer EJ (2005) Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353: 1784–1792
Biological Effects of Ionizing Radiation VII (BEIR VII) Committee to assess health risks from exposure to low levels of ionizing radiation, National Research Council. Health Risks from Exposure to Low Levels of Ionizing Radiation. National Academy of Sciences: Washington DC, 2006
Boice Jr JD, Harvey EB, Blettner M, Stovall M, Flannery JT (1992) Cancer in the contralateral breast after radiotherapy for breast cancer. N Engl J Med 326: 781–785
Brown ML, Hankey BF, Ballard-Barbash R (2000) Measuring the quality of breast cancer care. Ann Intern Med 133: 920
Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E, Godwin J, Gray R, Hicks C, James S, MacKinnon E, McGale P, McHugh T, Peto R, Taylor C, Wang Y (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366: 2087–2106
Curtis RE, Ron E, Hankey BF, Hoover RN (2006) New malignancies following breast cancer. In New Malignancies Among Cancer Survivors: SEER Cancer Registries 1973–2000, pp 181–205. National Cancer Institute: Bethesda, MD
Darby SC, McGale P, Taylor CW, Peto R (2005) Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300 000 women in US SEER cancer registries. Lancet Oncol 6: 557–565
Deutsch M, Land SR, Begovic M, Wieand HS, Wolmark N, Fisher B (2003) The incidence of lung carcinoma after surgery for breast carcinoma with and without postoperative radiotherapy. Results of National Surgical Adjuvant Breast and Bowel Project (NSABP) clinical trials B-04 and B-06. Cancer 98: 1362–1368
Epicure (2007) (Epiwin) Version 1 8. Microsoft International Corp: Seattle, USA
Fraumeni Jr JF, Curtis RE, Edwards BK, Tucker M (2006) Introduction. In New Malignancies Among Cancer Survivors: SEER Cancer Registries, 1973–2000 pp 1–7. National Cancer Institute: Bethesda, MD
Gao X, Fisher SG, Emami B (2003) Risk of second primary cancer in the contralateral breast in women treated for early-stage breast cancer: a population-based study. Int J Radiat Oncol Biol Phys 56: 1038–1045
Hooning MJ, Aleman BM, Hauptmann M, Baaijens MH, Klijn JG, Noyon R, Stovall M, van Leeuwen FE (2008) Roles of radiotherapy and chemotherapy in the development of contralateral breast cancer. J Clin Oncol 26: 5561–5568
Huang J, Mackillop WJ (2001) Increased risk of soft tissue sarcoma after radiotherapy in women with breast carcinoma. Cancer 92: 172–180
Kaufman EL, Jacobson JS, Hershman DL, Desai M, Neugut AI (2008) Effect of breast cancer radiotherapy and cigarette smoking on risk of second primary lung cancer. J Clin Oncol 26: 392–398
Liddell FD (1984) Simple exact analysis of the standardised mortality ratio. J Epidemiol Community Health 38: 85–88
Malin JL, Kahn KL, Adams J, Kwan L, Laouri M, Ganz PA (2002) Validity of cancer registry data for measuring the quality of breast cancer care. J Natl Cancer Inst 94: 835–844
Muren LP, Maurstad G, Hafslund R, Anker G, Dahl O (2002) Cardiac and pulmonary doses and complication probabilities in standard and conformal tangential irradiation in conservative management of breast cancer. Radiother Oncol 62: 173–178
Preston DL, Mattsson A, Holmberg E, Shore R, Hildreth NG, Boice Jr JD (2002) Radiation effects on breast cancer risk: a pooled analysis of eight cohorts. Radiat Res 158: 220–235
Preston DL, Ron E, Tokuoka S, Funamoto S, Nishi N, Soda M, Mabuchi K, Kodama K (2007) Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat Res 168: 1–64
Prochazka M, Hall P, Gagliardi G, Granath F, Nilsson BN, Shields PG, Tennis M, Czene K (2005) Ionizing radiation and tobacco use increases the risk of a subsequent lung carcinoma in women with breast cancer: case-only design. J Clin Oncol 23: 7467–7474
Ries LAG, Melbert D, Krapcho AP, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards BK (2008) SEER Cancer Statistics Review, 1975–2005. National Cancer Institute: Bethesda, MD http://seer.cancer.gov/csr/1975_2005/ based on November 2007 SEER data submission, posted to the SEER web site, 2008
Roychoudhuri R, Evans H, Robinson D, Moller H (2004) Radiation-induced malignancies following radiotherapy for breast cancer. Br J Cancer 91: 868–872
Schaapveld M, Visser O, Louwman MJ, de Vries EG, Willemse PH, Otter R, van der Graaf WT, Coebergh JW, van Leeuwen FE (2008) Risk of new primary nonbreast cancers after breast cancer treatment: a Dutch population-based study. J Clin Oncol 26: 1239–1246
Shank B, Moughan J, Owen J, Wilson F, Hanks GE (2000) The 1993–94 patterns of care process survey for breast irradiation after breast-conserving surgery-comparison with the 1992 standard for breast conservation treatment. The Patterns of Care Study, American College of Radiology. Int J Radiat Oncol Biol Phys 48: 1291–1299
Stovall M, Smith SA, Langholz BM, Boice Jr JD, Shore RE, Andersson M, Buchholz TA, Capanu M, Bernstein L, Lynch CF, Malone KE, Anton-Culver H, Haile RW, Rosenstein BS, Reiner AS, Thomas DC, Bernstein JL (2008) Dose to the contralateral breast from radiotherapy and risk of second primary breast cancer in the WECARE study. Int J Radiat Oncol Biol Phys 72: 1021–1030
Stovall M, Weathers R, Kasper C, Smith SA, Travis L, Ron E, Kleinerman R (2006) Dose reconstruction for therapeutic and diagnostic radiation exposures: use in epidemiological studies. Radiat Res 166: 141–157
Surveillance Research Program, National Cancer Institute SEER*Stat software (2007) (www.seer.cancer.gov/seerstat) version 6.4.4
Taylor CW, Nisbet A, McGale P, Darby SC (2007) Cardiac exposures in breast cancer radiotherapy: 1950s–1990s. Int J Radiat Oncol Biol Phys 69: 1484–1495
Van der Laan HP, Dolsma WV, Maduro JH, Korevaar EW, Langendijk JA (2008) Dosimetric consequences of the shift towards computed tomography guided target definition and planning for breast conserving therapy. Radiat Oncol 31: 6
Wang JS, Harris JR (2004) Postmasectomy radiation therapy. In Diseases of the Breast, 3rd edn, pp 785–800. Lippincott Williams & Wilkins: Philadelphia, PA
Yasui Y, Liu Y, Neglia JP, Friedman DL, Bhatia S, Meadows AT, Diller LR, Mertens AC, Whitton J, Robison LL (2003) A methodological issue in the analysis of second-primary cancer incidence in long-term survivors of childhood cancers. Am J Epidemiol 158: 1108–1113
Zablotska LB, Chak A, Das A, Neugut AI (2005) Increased risk of squamous cell esophageal cancer after adjuvant radiation therapy for primary breast cancer. Am J Epidemiol 161: 330–337
Zablotska LB, Neugut AI (2003) Lung carcinoma after radiation therapy in women treated with lumpectomy or mastectomy for primary breast carcinoma. Cancer 97: 1404–1411
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Berrington de Gonzalez, A., Curtis, R., Gilbert, E. et al. Second solid cancers after radiotherapy for breast cancer in SEER cancer registries. Br J Cancer 102, 220–226 (2010). https://doi.org/10.1038/sj.bjc.6605435
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605435
Keywords
This article is cited by
-
Risk of second primary cancer among women in the Kaiser Permanente Breast Cancer Survivors Cohort
Breast Cancer Research (2023)
-
Clinical and sociodemographic risk factors associated with the development of second primary cancers among postmenopausal breast cancer survivors
Breast Cancer (2023)
-
Cardiac dose in the treatment of synchronous bilateral breast cancer patients between three different radiotherapy techniques (VMAT, IMRT, and 3D CRT)
Discover Oncology (2023)
-
Mortality after second malignancy in breast cancer survivors compared to a first primary cancer: a nationwide longitudinal cohort study
npj Breast Cancer (2022)
-
Risk of primary lung cancer after breast cancer radiotherapy: a systematic review and meta-analysis
Breast Cancer (2022)