Abstract
Lung cancer is the primary cause of cancer mortality in developed countries. First diagnosis only when disease has already reached the metastatic phase is the main reason for failure in treatment. To this regard, although low-dose spiral computed tomography (CT) has proven to be effective in the early detection of lung cancer (providing both higher resectability and higher long-term survival rates), the capacity of annual CT screening to reduce lung cancer mortality in heavy smokers has yet to be demonstrated. Numerous ongoing large-scale randomised trials are under way in high-risk individuals with different study designs. The initial results should be available within the next 2 years.
Similar content being viewed by others
The magnitude of the problem
Lung cancer kills more than 1.3 million people every year (Peto et al, 1996), with figures registering a continual increase in the Far East in countries such as China (Yang et al, 2004). Improvements in clinical management have been modest over the past 20 years, with an overall 5-year survival rate just above 10% in Europe (Verdecchia et al, 2007). Presence of metastatic disease at diagnosis is the main reason for treatment failure, and 5-year survival of patients resected in stage Ia is >70% (Goldstraw et al, 2007). In developed countries, smoking sanctions have achieved a significant reduction in the prevalence of active smokers and lung cancer mortality in males, but not yet in females (Levi et al, 2003). Despite the success of early prevention, a large cohort of former smokers remain at high risk of cancer for many years.
Previous research involving other modalities
Early detection trials with chest radiography (CXR) and sputum cytology, funded by the US National Cancer Institute in the 1970s, were ineffective in decreasing lung cancer mortality, despite the higher proportion of early-stage cancer identified through screening (Melamed et al, 1984). Quite unexpectedly, the 25-year follow-up of the Mayo trial showed that overall mortality was higher in the CXR arm compared with the standard care arm (difference not reaching statistical significance, P=0.09), even though the survival rate of lung cancer patients diagnosed at an early stage in the CXR arm was much higher (69 vs 54% at 5 years, median 16 years vs 5 years, respectively) (Marcus et al, 2006). These results confirmed the inefficacy of CXR monitoring, as well as the occurrence of overdiagnosis in the intervention arm.
Observational studies with low-dose spiral CT
The advent of low-dose spiral chest computed tomography (LDCT) opened a new perspective for early diagnosis, and initial studies conducted in Japan in the 1990s demonstrated the potential value of LDCT for lung cancer screening (Kaneko et al, 1996). Since then, the rapid technological development in multislice machines has improved the sensitivity and reliability of spiral CT, providing the concrete possibility of detecting pulmonary lesions of 3–4 mm in size in a few seconds, without the use of intravenous contrast.
In 1999, the Cornell University of New York published the first results of the Early Lung Cancer Action Project (ELCAP), showing that spiral CT scans had accuracy and sensitivity rates that were six times higher than CXR results in identifying very small lung tumours (56% <1 cm) with a resectability rate of 96% and a frequency of stage I neoplasms of 85%. This study provided solid guidelines for the management of CT-detected pulmonary lesions, including needle aspiration biopsy of small pulmonary lesions (Henschke et al, 1999).
The results of observational studies, including 64 475 subjects, are summarised with relative references in Table 1. The median age was 59 years (range 53–67), with minimum age ranging from 40 to 60 years. Five studies included non-smokers, representing 17–54% of participants in each trial, and an overall proportion of 20%. In the remaining eight studies, the median pack-years (p-y) was 43 years (range 30–45).
At baseline, the overall frequency of participants with suspicious non-calcified solid lesions was 20% (range 7–53), lung cancer detection rate was 1% (range 0.4–2.7), and the proportion of stage I lung cancer was 81% (range 50–100%). The two extensive Japanese studies (Sone et al, 2001; Nawa et al, 2002) that included a significant proportion of non-smokers (38–54%) had the lowest frequency of baseline lesions (7–11%) and lung cancer detection rates (0.4–0.5%). On the other hand, the highest baseline detection rate (2.7%) reported by Henschke et al (1999) is mainly attributable to the accrual of heavier smokers above the age of 60 years (median 67 years, 45 p-y) and prolonged diagnostic workup of lesions detected at baseline (up to 2 years). In fact, in the more recent Korean study (Chong et al, 2005), in which nearly half of the 6406 participants were low risk and 23% were non-smokers, the lung cancer detection rate at baseline was only 0.4%. Interestingly, the use of the latest generation spiral CTs (8–16 slice) increased the frequency of subjects with suspicious nodules above 50%, but the lung cancer detection rate was not substantially greater (1.1%) (Veronesi et al, 2008). Ten studies reported the number of lung cancers detected at first annual CT repeat (Table 1): a total of 197 cases from 56 252 subjects, corresponding to a 0.3% rate (range 0.1–1.4) and a cumulative frequency at 2 years of 1.4% (range 0.6–2.6).
In studies in which the enrolled population demonstrated similar cancer risk factors, most of the differences observed in the baseline detection rate were related to the diagnostic algorithm, the analysis of CT images, and the definition of a positive screen applied by each centre, and tended to level up with the first CT repeat. In fact, excluding the two Japanese studies with a high proportion of non-smokers, the cumulative lung cancer detection rate by the second year of screening was 1.6% (range 1.3–2.6, Table 1).
Randomised trials with low-dose spiral CT
A number of randomised trials are currently being performed worldwide, involving more than 90 000 individuals (Table 2).
Of particular interest is the Lung Screening Study (LSS), a completed feasibility trial carried out in the United States, which randomised 3318 smokers (age 55–74 years, ⩾30 p-y, median 54 p-y) to LDCT or CXR, performed at baseline and first year repeat (Gohagan et al, 2005). The LSS confirmed LDCT’s higher lung cancer detection rate compared with CXR: 1.8 vs 0.5% at baseline, and 2.4 vs 1.3% at the first year repeat. On the basis of the success of LSS, the National Cancer Institute, in collaboration with the American College of Radiology Imaging Network, launched the National Lung Screening Trial, which represents the largest randomised controlled trial comparing LDCT with CXR, with lung cancer mortality as the end point (Clark et al, 2008). More than 53 000 participants were enrolled from over 30 centres across the United States. The National Lung Screening Trial has 90% statistical power to detect a 20% reduction in lung cancer mortality in the LDCT arm. The trial design included three annual screening examinations, which were completed in 2006, and subjects are currently in follow-up, with final results expected in 2011.
The European screening programme currently includes six randomised studies: the NELSON trial in the Netherlands, the Danish Lung Cancer Screening Trial in Denmark, The LUSI trial in Germany, and three Italian studies, namely, DANTE-Milan and ITALUNG-Florence, and MILD-Milan, all comparing annual CTs with observation without screening.
The NELSON trial was designed to detect a 25% reduction in lung cancer mortality in subjects aged 50–74 years having smoked >15 cigarettes per day for >25 years, or >10 cigarettes per day for >30 years, with a planned population of 20 000 subjects and three 16-slice CT examinations at years 1, 2, and 4 in the screening arm (van den Bergh et al, 2008). The NELSON trial accrued nearly 16 000 individuals in the Netherlands and Belgium, and the remaining 4000 needed to reach statistical power were recruited from Denmark. Initial results of Nelson have shown a 0.9% lung cancer detection rate at baseline, with a 99.9% negative predictive value of the diagnostic algorithm, based on the automated assessment of volume and doubling time (van Klaveren et al, 2009). The proportion of invasive procedures that revealed benign disease was 27.2%. The Danish Lung Cancer Screening Trial has a similar risk population (50–70 years, ⩾20 p-y), but includes annual CT screening for 5 years, with results regularly uploaded into the Nelson database. The baseline lung cancer detection rate of the Danish Lung Cancer Screening Trial was similar to the one of Nelson (0.8%) (Pedersen et al, 2009).
A similar trial, LUSI, was launched in Germany in 2007, and is now in the randomisation phase (Becker et al, 2008).
The DANTE-Milan study was the first European randomised trial to be launched in 2001, enrolling 2472 subjects (60–74 years, ⩾20 p-y) in annual CT screenings or in observation for 4 years (Infante et al, 2008). At baseline, participants in both arms had to undergo one single CXR and sputum cytology examination, which led to lung cancer detection in eight patients in the control arm. The ITALUNG-Florence randomised 3206 subjects (55–69 years, ⩾20 p-y) to annual CT vs observation for 4 years. Baseline CT detected 21 lung cancers in 20 subjects (1.5%) (Lopes Pegna et al, 2009). The Multicentric Italian Lung Detection trial started in Milan in 2005 and is still open to accrual. Until now, more than 4400 participants have been assigned to LDCT or control, for a period of 10 years. In the LDCT arm, a second randomisation has been planned to compare yearly CT screening with testing every 2 years. All participants will undergo an antitobacco counselling programme, pulmonary function test evaluation, and tissue sampling for extensive biomarker assessment.
A pilot trial, entitled Depiscan, was launched in France in 2002, to assess the feasibility of a screening programme with accrual based on 232 general practitioners and occupational physicians. The trial entered only 621 subjects in 2 years, and was closed because of insufficient accrual (41% active investigators) and poor compliance (Blanchon et al, 2007). At baseline, eight lung cancers (2.4%) were detected in the CT arm and one (0.4%) in the CXR arm. A further randomised trial is still in the planning phase in the United Kingdom.
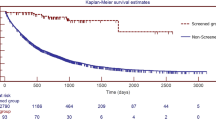
The DANTE study is the only European study with published results on screening efficacy (Infante et al, 2009). After a median follow-up of 3 years, lung cancer was detected in 60 (4.7%) subjects receiving LDCT and in 34 (2.8%) controls (P=0.016), with a higher percentage of stage I lung cancer (54 vs 34%, respectively; not significantly different: P=0.06), corresponding to a three-fold increase in the total number of stage I lung cancer cases (33 vs 12; P=0.004). However, the number of stage III–IV lung cancers was not reduced in the LDCT arm (24 vs 21 cases), and lung cancer mortality was identical in the two arms (20 deaths each), as well as mortality due to other causes (26 vs 25). In summary, the mid-term results of the first randomised trial have not confirmed LDCT screening as having a measurable effect in diminishing lung cancer mortality. Nonetheless, a definitive answer regarding the concrete possibility of preventing mortality in heavy smokers with annual LDCT screening will be determined by the long-term follow-up of all randomised trials, the first of which is the National Lung Screening Trial. A research priority for the coming years will be to guarantee that all European trials, in which the control arm is observational and intervention is prolonged beyond 3 years, can be pooled in a large meta-analysis, to reach adequate statistical power.
Issues specific to screening with spiral CT
Prevalence of false-positive findings
The frequency of non-calcified pulmonary lesions in heavy smokers aged ⩾50 years is related to the sensitivity of the spiral CT: with the 16-slice CT, the lung cancer diagnostic rate is about 1% per year, but the probability of detecting benign lesions is 50 times higher (Veronesi et al, 2008, Table 1). Consequently, the overall screening performance depends on the selected diagnostic algorithm.
In the Mayo CT trial, the cumulative frequency of subjects with suspicious lesions was 74% at 5 years, but only 6% of them proved to have cancer, with a 70% rate of false-positive findings among all participants in the study (Swensen et al, 2005), whereas in the Milan study, using single-slice CT and a cutoff diameter above 5 mm, the frequency of subjects with suspicious lesions was only 19% at 5 years, 20% of whom proved to have cancer, with only 15% false-positive CTs overall (Pastorino, 2006). Nonetheless, the cumulative lung cancer detection rate was 4% in both trials (average 0.8% per year), with other major end points such as resectability and proportion of stage I disease being very similar. These results are intriguing in terms of screening performance, as one would expect a more sensitive diagnostic workup to be associated with a better clinical outcome.
Diagnostic assessment of small pulmonary nodules requires serial CT scanning for the detection of morphological changes, and the availability of reliable software for fully automated three-dimensional segmentation and highly consistent volume measurement of lung nodules has become essential in evaluating growth as evidence of potential malignancy (Wiemker et al, 2005; Marchianò et al, 2009).
Long-term follow-up of lesions ⩽5 mm suggests that these nodules require no additional workup. For lesions between 5 and 10 mm, surveillance of growth should be performed by three-dimensional volumetry, as volume doubling is equivalent to only a 26% increase in diameter, a difference that may be difficult to detect with manually guided diameter measurements. Changes in size indicative of a doubling time ranging from 30 to 360 days are consistent with cancer and require further investigation (Libby et al, 2004).
Pure non-solid lesions, or ground-glass opacities, have a low risk of malignancy (10–15%), usually represented by well-differentiated bronchioloalveolar carcinomas (BACs), but their volume and growth are more difficult to evaluate. Part-solid lesions have a higher risk of malignancy (up to 50%), directly related to the size and growth of the solid component (Henschke et al, 2002).
Role of PET in diagnostic evaluation of positive CT screens
Large meta-analyses have demonstrated the clinical value of PET in the differential diagnosis of undetermined pulmonary nodules detected by spiral CT, with a sensitivity rate of 96–97%, a specificity of 78–82%, and an accuracy rate reaching 92% with the CT/PET fusion machine (Kim et al, 2007). Moreover, a randomised trial demonstrated that preoperative PET significantly improves lung cancer staging, by detecting occult metastases in otherwise resectable patients (van Tinteren et al, 2002).
In a recent paper, we reported that selective use of PET scans may be helpful in the management of CT-detected lesions ⩾7 mm. In the first 5 years of screening, PET was applied to only 1.4% of spiral CTs, with an overall sensitivity rate of 94%, specificity of 82%, and an accuracy rate of 88% (Pastorino et al, 2009). In addition, we demonstrated that the intensity of metabolic activity, expressed by standardised uptake value (SUV), can predict long-term survival in screening-detected lung cancer in a non-invasive manner. In fact, 5-year survival was 100% for SUV ⩽2.5, 60% for SUV >2.5 and <8, and only 20% for SUV ⩾8 (P=0.001). If confirmed by other studies, these results might improve the clinical management of CT-detected tumours in the future, reducing the risk of unnecessary treatment for indolent disease.
Overdiagnosis of indolent tumours
Detection and treatment of slow-growing disease, also called overdiagnosis, represents one of the most likely explanations for the lack of mortality reduction observed in chest X-ray-screening trials, despite a significant increase in the overall resectability rate and proportion of stage I cancers in the intervention arm (Marcus et al, 2006). Overdiagnosis bias refers to the screening-related detection of cancers that would not have contributed to the death of the patient because of competing causes of death or because the lesion is indolent. The occurrence of slow-growing lung cancer has often been rejected because of similar histopathological and molecular features of screening and non-screening-detected cases. However, the significant rise in the frequency of adenocarcinoma from 32% of all cases in the SEER database from 1983 to 1987 (Travis et al, 1995) to more than 70% (range 55–95%) in CT-screening trials (Table 1 references) may well represent overdiagnosis. An international panel has reviewed the histopathological features of 279 stage IA adenocarcinomas belonging to the I-ELCAP database, to determine whether survival differed from the proportion of the BAC component (Vazquez et al, 2008). The revision confirmed that 81% of CT-detected adenocarcinomas show a substantial BAC component, and that 5-year survival was 100% for pure BAC and 95% for mixed BAC. Such a sudden shift towards adenocarcinoma and BAC cannot be explained by major changes in the epidemiology of tobacco consumption, and is strongly suggestive of an excessive detection of indolent disease by CT screening.
Morbidity of CT screening
The side effects and morbidity of CT screening are difficult to assess using observational studies. The frequency of surgical procedures for benign disease, not including bronchoscopy and fine-needle aspiration biopsy, is reported in Table 3. Invasive biopsies for benign lesions represent, on an average, 18% (range 0–33%) of all surgical procedures and 0.3% of individuals undergoing CT screening. Postoperative mortality is not mentioned in most studies, and numbers are too low for a proper estimate of the risk. Randomised trials may allow a better evaluation of the impact of CT screening on quality of life and proportion of unnecessary invasive diagnostic procedures and hospital admissions, including morbidity and mortality, by comparing the two arms.
Lung cancer mortality and survival in CT screening
In 2005, Swensen et al, comparing the lung cancer mortality rates in the Mayo CT study with those observed in the previous CXR trial, found no differences in lung cancer mortality rates between the two studies in the subset of men aged 50 years or older (2.8 vs 2.0 per 1000 person-years) (Swensen et al, 2005). On the other hand, in 2006, the International ELCAP study group published a report on the efficacy of CT screening, in which the overall survival of 484 screening-detected lung cancer patients was 80% at 10 years, regardless of stage and treatment, and reached 92% in the subset of clinical stage I resected within 1 month of diagnosis (I-ELCAP, 2006). The authors therefore concluded that CT screening could prevent 80% of all lung cancer deaths in high-risk individuals. However, the analysis was focused only on cancer detected at baseline and first CT repeat, without long-term follow-up of the entire cohort. Moreover, patients’ outcome at 10 years was projected from a median observation period of only 3 years, and lung cancer-specific survival was used instead of overall survival.
A concurrent meta-analysis of three single-arm studies (Mayo Clinic, Milan and Lee Moffitt Cancer Center) including 3246 subjects and 10 942 person-years was performed by the epidemiologists of Memorial Sloan Kettering Cancer Centre, using a validated model to predict lung cancer incidence and mortality (Bach et al, 2007). The results of this study, published in JAMA, 2007, demonstrated that CT screening resulted in a 3.5-fold increase in lung cancer diagnoses and a 10-fold increase in surgical resections. However, the number of cases of advanced lung cancer and lung cancer death did not differ from expected numbers of advanced lung cancer and lung cancer death, with those numbers generated from a simulation model that used the CARET data. Quite interestingly, the results were consistent among all three centres, despite the potential differences in epidemiological risk and screening methodology, mirroring the findings of the only published randomised trial, the DANTE study, in which lung cancer mortality was identical in the CT screening and observational arms (Infante et al, 2009). Why was earlier detection in the first 2 years of screening not effective in preventing, at least to some extent, the occurrence of metastatic lung cancer in the long term? One possible explanation is that spiral CT is unable to intercept the fast-growing or ‘most aggressive’ lung cancers before the onset of metastases.
Role of biomarkers in lung cancer screening
Biomarker research in CT screening trials, combining non-invasive genomic and proteomic analysis of target tissues, may represent a significant improvement in early detection, offering a potential contribution to diagnostic algorithms, assessment of individual risk, as well as management of CT-detected cancers. The issue of early detection biomarkers in lung cancer has recently been reviewed by Montuenga and Pio (2009), with a focus on blood and sputum evaluation. Even though there is no single validated molecular biomarker for early lung cancer detection, a complex spectrum of molecular profiles in body fluids of subjects enrolled in CT screening trials now offers truly innovative prospects for early diagnosis.
For instance, proteomic analysis of plasma, using SELDI-TOF and protein chip technology, has revealed high sensitivity and specificity, with an 8.7-fold excess risk of cancer for CT-screened individuals with elevated SAA protein levels (Cremona et al, 2010). Another new field of research is represented by breathing analysis, using electronic sensors (e-nose) to capture volatile compounds, or to extract genomic and proteomic material from frozen exhaled breath condensation (Horváth et al, 2009).
Conclusions
Prospective randomised controlled trials remain the most appropriate instrument to test the efficacy of CT screening in heavy smokers. The ongoing randomised studies currently being conducted around the world have the adequate size and appropriate design to provide unequivocal evidence of even modest reductions in lung cancer mortality. In the meantime, CT screening for lung cancer should be considered as an experimental procedure, which is not to be offered or promoted outside controlled clinical trials. Innovative strategies could be tested to implement early detection research, possibly combining radiological monitoring with pharmacological intervention on smoking cessation, and the validation of lung biomarkers.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bach PB, Jett JR, Pastorino U, Tockman MS, Swensen SJ, Begg CB (2007) Computed tomography screening and lung cancer outcomes. JAMA 297: 953–961
Bastarrika G, García-Velloso MJ, Lozano MD, Montes U, Torre W, Spiteri N, Campo A, Seijo L, Alcaide AB, Pueyo J, Cano D, Vivas I, Cosín O, Domínguez P, Serra P, Richter JA, Montuenga L, Zulueta JJ (2005) Early lung cancer detection using spiral computed tomography and positron emission tomography. Am J Respir Crit Care Med 171: 1378–1383
Becker N, Delorme S, Kauczor HU (2008) LUSI: the German component of the European trial on the efficacy of multislice-CT for the early detection of lung cancer. Onkologie 31: PO320
Blanchon T, Bréchot JM, Grenier PA, Ferretti GR, Lemarié E, Milleron B, Chagué D, Laurent F, Martinet Y, Beigelman-Aubry C, Blanchon F, Revel MP, Friard S, Rémy-Jardin M, Vasile M, Santelmo N, Lecalier A, Lefébure P, Moro-Sibilot D, Breton JL, Carette MF, Brambilla C, Fournel F, Kieffer A, Frija G, Flahault A, ‘Dépiscan’ Group (2007) Baseline results of the Depiscan study: a French randomized pilot trial of lung cancer screening comparing low dose CT scan (LDCT) and chest X-ray (CXR). Lung Cancer 58: 50–58
Chong S, Lee KS, Chung MJ, Kim TS, Kim H, Kwon OJ, Choi YH, Rhee CH (2005) Lung cancer screening with low-dose helical CT in Korea: experiences at the Samsung Medical Center. J Korean Med Sci 20 (3): 402–408
Clark KW, Gierada DS, Marquez D, Moore SM, Maffitt DR, Moulton JD, Wolfsberger MA, Koppel P, Phillips SR, Prior FW (2008) Collecting 48 000 CT Exams for the Lung Screening Study of the National Lung Screening Trial. J Digit Imaging 22 (6): 667–680
Cremona M, Calabrò E, Randi G, De Bortoli M, Modellini P, Verri C, Sozzi G, Pierotti MA, La Vecchia C, Pastorino U, Bongarzone I (2010) Diagnostic value of SELDI-TOF MS plasma peptidome in early-stage lung cancer. Cancer 116: 1326–1335
Diederich S, Thomas M, Semik M, Lenzen H, Roos N, Weber A, Heindel W, Wormanns D (2004) Screening for early lung cancer with low-dose spiral computed tomography: results of annual follow-up examinations in asymptomatic smokers. Eur Radiol 14: 691–702
Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, Postmus PE, Rusch V, Sobin L (2007) The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol 2: 706–714
Gohagan JK, Marcus PM, Fagerstrom RM, Pinsky PF, Kramer BS, Prorok PC, Ascher S, Bailey W, Brewer B, Church T, Engelhard D, Ford M, Fouad M, Freedman M, Gelmann E, Gierada D, Hocking W, Inampudi S, Irons B, Johnson CC, Jones A, Kucera G, Kvale P, Lappe K, Manor W, Moore A, Nath H, Neff S, Oken M, Plunkett M, Price H, Reding D, Riley T, Schwartz M, Spizarny D, Yoffie R, Zylak C, The Lung Screening Study Research Group (2005) Final results of the Lung Screening Study, a randomized feasibility study of spiral CT versus chest X-ray screening for lung cancer. Lung Cancer 47: 9–15
Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, Libby DM, Pasmantier MW, Koizumi J, Altorki NK, Smith JP (1999) Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet 354: 99–105
Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS (2002) CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 178: 1053–1057
Horváth I, Lázár Z, Gyulai N, Kollai M, Losonczy G (2009) Exhaled biomarkers in lung cancer. Eur Respir J 34: 261–275. Review
Infante M, Lutman FR, Cavuto S, Brambilla G, Chiesa G, Passera E, Angeli E, Chiarenza M, Aranzulla G, Cariboni U, Alloisio M, Incarbone M, Testori A, Destro A, Cappuzzo F, Roncalli M, Santoro A, Ravasi G, DANTE Study Group (2008) Lung cancer screening with spiral CT: baseline results of the randomized DANTE trial. Lung Cancer 59: 355–363
Infante M, Cavuto S, Lutman FR, Brambilla G, Chiesa G, Ceresoli G, Passera E, Angeli E, Chiarenza M, Aranzulla G, Cariboni U, Errico V, Inzirillo F, Bottoni E, Voulaz M, Alloisio M, Destro A, Roncalli M, Santoro A, Ravasi G, for the DANTE Study Group (2009) A randomized study of lung cancer screening with spiral computed tomography (the DANTE Trial): three-year results. Am J Resp Crit Care Med 180: 445–453
The International Early Lung Cancer Action Program Investigators (I-ELCAP) (2006) Survival of patients with stage I lung cancer detected on CT screening. N Engl J Med 355: 1763–1771
Kaneko M, Eguchi K, Ohmatsu H, Kakinuma R, Naruke T, Suemasu K, Moriyama N (1996) Peripheral lung cancer: screening and detection with low-dose spiral CT versus radiography. Radiology 201: 798–802
Kim SK, Allen-Auerbach M, Goldin J, Fueger BJ, Dahlbom M, Brown M, Czernin J, Schiepers C (2007) Accuracy of PET/CT in characterization of solitary pulmonary lesions. J Nucl Med 48: 214–220
Levi F, Lucchini F, Negri E, Boyle P, La Vecchia C (2003) Mortality from major cancer sites in the European Union, 1955–1998. Ann Oncol 14: 490–495
Libby DM, Smith JP, Altorki NK, Pasmantier MW, Yankelevitz D, Henschke CI (2004) Managing the small pulmonary nodule discovered by CT. Chest 125: 1522–1529. Review
Lopes Pegna A, Picozzi G, Mascalchi M, Maria Carozzi F, Carrozzi L, Comin C, Spinelli C, Falaschi F, Grazzini M, Innocenti F, Ronchi C, Paci E, for the ITALUNG Study Research Group (2009) Design, recruitment and baseline results of the ITALUNG trial for lung cancer screening with low-dose CT. Lung Cancer 64 (1): 34–40
MacRedmond R, McVey G, Lee M, Costello RW, Kenny D, Foley C, Logan PM (2006) Screening for lung cancer using low dose CT scanning: results of 2 year follow up. Thorax 61: 54–56
Marchianò A, Calabrò E, Civelli E, Di Tolla G, Frigerio LF, Morosi C, Tafaro F, Ferri E, Sverzellati N, Camerini T, Mariani L, Lo Vullo S, Pastorino U (2009) Pulmonary nodules: volume repeatability at multidetector CT lung cancer screening. Radiology 251: 919–925
Marcus PM, Bergstralh EJ, Zweig MH, Harris A, Offord KP, Fontana RS (2006) Extended lung cancer incidence follow-up in the Mayo Lung Project and overdiagnosis. J Natl Cancer Inst 98: 748–756
Melamed MR, Flehinger BJ, Zaman MB, Heelan RT, Parchick WA, Martini N (1984) Screening for lung cancer: results of the Memorial Sloan-Kettering study in New York. Chest 86: 44–53
Montuenga LM, Pio R (2009) Current challenges in lung cancer early detection biomarkers. Eur J Cancer 45 (Suppl 1): 377–378
Nawa T, Nakagawa T, Kusano S, Kawasaki Y, Sugawara Y, Nakata H (2002) Lung cancer screening using low-dose spiral CT: results of baseline and 1-year follow-up studies. Chest 122: 15–20
Novello S, Fava C, Borasio P, Dogliotti L, Cortese G, Crida B, Selvaggi G, Lausi P, Brizzi MP, Sperone P, Cardinale L, Ferraris F, Perotto F, Priola A, Scagliotti G (2005) Three-year ndings of an early lung cancer detection feasibility study with low-dose spiral computed tomography in heavy smokers. Ann Oncol 16: 1662–1666
Pastorino U (2006) Early detection of lung cancer. Respiration 73: 5–13
Pastorino U, Bellomi M, Landoni C, De Fiori E, Arnaldi P, Picchio M, Pelosi G, Boyle P, Fazio F (2003) Early lung-cancer detection with spiral CT and positron emission tomography in heavy smokers: 2-year results. Lancet 362: 593–597
Pastorino U, Landoni C, Marchianò A, Calabrò E, Sozzi G, Miceli R, Picchio M, Mariani L, Messa C, Fazio F (2009) Fluorodeoxyglucose (FDG) uptake measured by positron emission tomography (PET) and standardised uptake value (SUV) predicts long-term survival of CT screening-detected lung cancer in heavy smokers. J Thor Oncol 11: 1352–1356
Pedersen JH, Ashraf H, Dirksen A, Bach K, Hansen H, Toennesen P, Thorsen H, Brodersen J, Skov BG, Døssing M, Mortensen J, Richter K, Clementsen P, Seersholm N (2009) The Danish randomized lung cancer CT screening trial – overall design and results of the prevalence round. J Thorac Oncol 4: 608–614
Peto R, Lopez AD, Boreham J, Thun M, Heath Jr C, Doll R (1996) Mortality from smoking worldwide. Br Med Bul 52: 12–21
Sobue T, Moriyama N, Kaneko M, Kusumoto M, Kobayashi T, Tsuchiya R, Kakinuma R, Ohmatsu H, Nagai K, Nishiyama H, Matsui E, Eguchi K (2002) Screening for lung cancer with low-dose helical computed tomography: anti-lung cancer association project. J Clin Oncol 20: 911–920
Sone S, Li F, Yang ZG, Honda T, Maruyama Y, Takashima S, Hasegawa M, Kawakami S, Kubo K, Haniuda M, Yamanda T (2001) Results of three-year mass screening programme for lung cancer using mobile low-dose spiral computed tomography scanner. Br J Cancer 84: 25–32
Swensen SJ, Jett JR, Hartman TE, Midthun DE, Mandrekar SJ, Hillman SL, Sykes AM, Aughenbaugh GL, Bungum AO, Allen KL (2005) CT screening for lung cancer: five-year prospective experience 1. Radiology 235: 259–265
Swensen SJ, Jett JR, Hartman TE, Midthun DE, Sloan JA, Sykes AM, Aughenbaugh GL, Clemens MA (2003) Lung cancer screening with CT: Mayo Clinic experience. Radiology 226: 756–761
Travis DL, Travis LB, Devesa SS (1995) Lung Cancer. Cancer 75: 191–202
van den Bergh KA, Essink-Bot ML, Bunge EM, Scholten ET, Prokop M, van Iersel CA, van Klaveren RJ, de Koning HJ (2008) Impact of computed tomography screening for lung cancer on participants in a randomized controlled trial (NELSON trial). Cancer 113: 396–404
van Klaveren RJ, Oudkerk M, Prokop M, Scholten ET, Nackaerts K, Vernhout R, van Iersel CA, van den Bergh KA, van’t Westeinde S, van der Aalst C, Thunnissen E, Xu DM, Wang Y, Zhao Y, Gietema HA, de Hoop BJ, Groen HJ, de Bock GH, van Ooijen P, Weenink C, Verschakelen J, Lammers JW, Timens W, Willebrand D, Vink A, Mali W, de Koning HJ (2009) Management of lung nodules detected by volume CT scanning. N Engl J Med 361: 2221–2229
van Tinteren H, Hoekstra OS, Smit EF, van den Bergh J, Schreurs JM, Stallaert R, van Velthoven P, Comans E, Diepenhorst FW, Verboom P, van Mourik JC, Postmus PE, Boers M, Teule GJ, The PLUS Study Group (2002) Effectiveness of positron emission tomography in the preoperative assessment of patients with suspected non-small-cell lung cancer: the PLUS multicentre randomised trial. Lancet 359: 1388–1392
Vazquez M, Carter D, Brambilla E, Gazdar A, Noguchi M, Travis WD, Huang Y, Zhang L, Yip R, Yankelevitz DF, Henschke CI, The International Early Lung Cancer Action Program Investigators (2008) Solitary and multiple resected adenocarcinomas after CT screening for lung cancer: histopathologic features and their prognostic implications. Lung Cancer 64 (2): 148–154
Verdecchia A, Franceschi S, Brenner H, Gatta G, Micheli A, Mangone L, Kunkler I (2007) Recent cancer survival in Europe: a 2000–02 period analysis of EUROCARE 4 data. Lancet Oncol 8: 784–796
Veronesi G, Bellomi M, Mulshine JL, Pelosi G, Scanagatta P, Paganelli G, Maisonneuve P, Preda L, Leo F, Bertolotti R, Solli P, Spaggiari L (2008) Lung cancer screening with low-dose computed tomography: a non-invasive diagnostic protocol for baseline lung nodules. Lung Cancer 61: 340–349
Wiemker R, Rogalla P, Blaffert T, Sifri D, Hay O, Shah E, Truyen R, Fleiter T (2005) Aspects of computer-aided detection (CAD) and volumetry of pulmonary nodules using multislice CT. Br J Radiol 78: S46–S56
Yang L, Parkin DM, Li LD, Chen YD, Bray F (2004) Estimation and projection of the national profile of cancer mortality in China: 1991–2005. Br J Cancer 90: 2157–2166
Acknowledgements
The Milan Early Detection Research programme is supported by a Research Grant from the Italian Ministry of Health (Ricerca Finalizzata), the Italian Association for Cancer Research (AIRC), and the Cariplo Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Pastorino, U. Lung cancer screening. Br J Cancer 102, 1681–1686 (2010). https://doi.org/10.1038/sj.bjc.6605660
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605660
Keywords
This article is cited by
-
CircPVT1: a pivotal circular node intersecting Long Non-Coding-PVT1 and c-MYC oncogenic signals
Molecular Cancer (2022)
-
Speckle-type POZ protein functions as a tumor suppressor in non-small cell lung cancer due to DNA methylation
Cancer Cell International (2018)
-
Concurrent chemoradiotherapy with weekly nedaplatin versus radiotherapy alone in elderly patients with non-small-cell lung cancer
Clinical and Translational Oncology (2018)
-
BCI induces apoptosis via generation of reactive oxygen species and activation of intrinsic mitochondrial pathway in H1299 lung cancer cells
Science China Life Sciences (2018)
-
Trade-off between benefits, harms and economic efficiency of low-dose CT lung cancer screening: a microsimulation analysis of nodule management strategies in a population-based setting
BMC Medicine (2017)