Abstract
Aims
To study the pattern of residual undetached cortical vitreous (RCV) after posterior vitreous detachment (PVD) in eyes with rhegmatogenous retinal detachment (RRD) and to examine the relationship between RCV and the development of epiretinal membrane (ERM).
Methods
A prospective study was conducted in 33 consecutive patients with clinically evident PVD who underwent pars plana vitrectomy for RRD. During vitrectomy, triamcinolone acetonide (0.2 cm3, 10 mg/cm3) was applied to stain the RCV. The pattern of the staining were recorded. The formation of postoperative ERM was correlated with the staining pattern of RCV. Each case was followed for at least 6 months.
Results
In all, 23 of the 33 patients had RCV of variable size, with a single stain patch observed in 13 patients and multiple patches in seven patients. Large circumferential areas of staining at the mid-periphery were noted in three patients. A total of 10 cases had staining over the fovea and five patients had staining over the disc. ERM developed in seven patients during follow-up. None corresponded to RCV.
Conclusion
RCV is common in eyes with PVD and RRD. The macula and disc area are the most frequent locations for these vitreous islands. The relationship between RCV and ERM remains to be investigated.
Similar content being viewed by others
Introduction
Spontaneous posterior vitreous detachment (PVD) occurs in more than half of those older than 50 years, and the overall incidence is nearly 30%.1 After PVD, avulsion of retina vessels, vitreoretinal traction, and retinal flap tears may develop at areas of strong vitreoretinal adhesion. Conversely, fragments of hyaloid membrane may be left undetached on the posterior retina without causing significant retinal changes. The location and the long-term effect of these residual membranes have not been fully studied.
Clinical examination of the vitreous can be compromised by its transparency. Use of the Goldmann contact lens has been advocated for examination of peripheral vitreous and visualization of cells, along with the El Bayadi-Kajiura lens for visualization of complex posterior vitreoretinal relationships.2 Kinetic contact B-scan ultrasonography has been a useful diagnostic adjunct in determining the status of the vitreoretinal interface.3 As well, monochromic photography usefully documents the spatial relationships in macular vitreoretinal interface disorder.4 Scanning laser ophthalmoscopy, optical coherence tomography and dynamic light scattering enable better visualization of the vitreoretinal interface.5, 6, 7
As helpful as these techniques are in studying the vitreous, they either require experienced investigators or examine only a limited area of the vitreo-retinal structure. Furthermore, marked variations in individual observation results can occur.
Recently, triamcinolone acetonide (TA) has been used to improve the visualization of cortical vitreous during vitrectomy surgery.8, 9 Residual cortical vitreous are observed directly after the steroid particles adhere to the vitreous fibres. Presently, we used TA to stain the residual hyaloid membranes on the retinal surface in eyes undergoing vitrectomy for rhegmatogenous retinal detachment (RRD) with spontaneous PVD. We studied the location and pattern of residual undetached cortical vitreous and examined the relationship between premacular hyaloid fragments and the development of epimacular membrane.
Materials and methods
We prospectively studied 33 consecutive patients (33 eyes) with spontaneous PVD and RRD requiring pars plana vitrectomy. The study was approved by the ethics committee of National Taiwan University Hospital. A clearly visible Weiss ring was the criteria for the presence of PVD. Eyes with inflammatory diseases, diabetic retinopathy or history of previous retinal surgery were excluded. The patients (11 men, 22 women) ranged in age from 13 to 85 years (average, 49.1 years). Each patient was examined and followed for more than 6 months (average follow-up period, 12 months; range, 6–16 months) in National Taiwan University Hospital between February 2003 and July 2004.
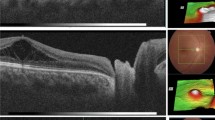
In all cases, the ocular examination included best-corrected Snellen visual acuity, slit-lamp biomicroscopy, and indirect ophthalmoscopy. The vitreous was studied preoperatively with +90-diopter(D) lens under the slit lamp, which allowed observation of the posterior detached vitreous in patients with RRD. After verifying the presence of PVD by direct observation of the hyaloid during the initial phase of PPV, TA (0.2 cm3; 10 mg/cm3) was dispersed over the retinal surface with a 20-gauge needle. The suspension became visibly trapped in the gel structure of the residual undetached cortical vitreous. TA particles that settled on the dependent retinal surface were washed out by backflushing using the backflush needle or the vitrectomy probe. The size, location, and shape of the staining area were recorded. In a few instances, isolated hyaloid fragments outside the macular area were selectively engaged with the backflush needle to test the strength of adhesiveness. All patients were clinically examined at 1 and 4 weeks, 3 months, and at least 6 months postoperatively. Follow-up examinations included best-corrected visual acuity, degree of ocular inflammation, intraocular pressure (IOP), and anatomical outcome. Epiretinal membrane formation was examined using +90 D lens under the slit lamp.
Results
Of the 33 patients, four were without definite refraction documentation, and high myopia was noted in 12 patients (36.4%) (nine males, three females). High myopia is defined as a refractive error with spherical equivalent equal to or more then −6 D; a refractive error of less than −6 D is defined as low myopia. In all, 23 of the 33 patients (69.7%; 18 males, five females) had residual vitreous staining on the retinal surface during surgery, 13 patients (39.4%) had a single patch of staining and seven patients (21.2%) displayed multiple patches. The individual staining area was approximately one-fifth to seven disc size. Three patients (9.1%) displayed large circumferential areas of vitreo-retinal adhesion at mid-periphery connecting with the peripheral vitreous. Of these patients, one had vitreous attached on the nasal side and the other two had 360-degree attachment (Table 1).
The commonest site of staining was the macula (10 of 23 cases, 43.5%), followed equally by the disc and temporal-upper quadrant (both five of 23 cases, 21.7%). The schematic representation of the staining location is shown in Figure 1. Stronger adherence of the residual vitreous was noticed in younger patients. The average age of the 23 cases with positive staining finding was 49.8, while that of the other 10 cases was 52.2. In all, 13 of the 18 cases (72.2%) who were younger than 50 years old had residual undetached vitreous. Of the remaining 15 patients, 10 (66.7%) who were aged 50 years and above had residual vitreous (Table 2).
In all, 10 of 12 (83.3%) high myopic patients vs 10 of 17 (58.8%) low myopic patients had residual vitreous (Table 3).
ERM development was noted during postoperative follow-ups in seven patients (21.2%). This development occurred over the macula (n=5), between the macula and the disc (n=1) and at the temporal-lower quadrant (n=1). Three of these seven patients did not show any RCV by previous TA staining. The remaining four patients did not show a location of ERM formation identical to that of RCV. There were no complications, including endophthalmitis, intraocular pressure elevation, or iatrogenic retinal detachment, in any of the patients. In all, 31 of the 33 patients obtained reattachment with a single operation. Redetachment of the retina occurred in two patients. They were successfully treated during a second surgery with silicone oil injection.
Discussion
Cortical fragments adherent to the retina after PVD is not an uncommon finding. Histopathological examination has revealed that 44% of eyes with a spontaneous PVD have remnants of the vitreous cortex at the macula.10 Endoillumination examination of 48 eyes with RRD and PVD revealed an oval or round defect in detached hyaloid membrane in 31 eyes (65%) and a break in the premacular area in 12 eyes (25%).11, 12 Triamcinolone has been successfully used to stain the cortical vitreous remained on the retinal surface after mechanically induced PVD during vitrectomy.13 Residual hyaloid fragments could be identified directly, with three patterns of RCV being evident: diffuse type (30% incidence), focal type (30%), and no residual RCV (40%). Unlike this previous study, we applied steroid staining after patients developed spontaneous PVD. This technique detected single-patch RCV in 39.4% of our patients; multiple patches in 21.2%, large circumferential patches at mid-periphery in 9.1%, and no RCV in 30.3%. It is unclear whether different underlying aetiologies or the difference in PVD formation caused the distinction between the two studies.
Kimura et al14 conducted a similar study to observe the premacular vitreous remnant in eyes with RRD. The fragments were removed during vitrectomy. Six of nine eyes (69%) showed remnants of cortical vitreous at the macula. In accordance with these results, the present study also found that significant cases had residual vitreous at the macula and in other areas as well. Unlike the study of Kimura et al, our study was designed so that all the residual vitreous on the macula and most fragments outside the macula were not removed, to allow the examination of the relationship between the residual vitreous and the formation of clinically significant ERM. Past studies have suggested macular undetached hyaloid fragments may be related to future ERM. Kishi and Shimizu11, 12 postulated that the premacular vitreous cortex or the posterior wall of the vitreous pocket is a major structural component of idiopathic premacular fibrosis. Attachment of the vitreous to the macula after PVD may be related to the development of idiopathic premacular fibrosis.15 However, presently, even though seven patients developed visible ERM during follow-up period, none of them had residual vitreous corresponding to the later occurrence of ERM. Furthermore, one patient with vitreous haemorrhage but without triamcinolone macular staining developed a severe macular pucker. These results suggest that residual hyaloid may not be a necessary factor for the development of visible ERM in eyes with RD. On the other hand, we did not examine with OCT pre- and postoperatively. Thus, some thin epiretinal membranes might be missed. Although most of TA suspension was washed out during operation, we cannot rule out the possibility that the transient presence of steroid particles trapped in residual cortical vitreous might play a role in modulating ERM formation. Visible ERM formation can sometimes not take place until nearly 2 years after PVD.16 A longer follow-up period is needed to clarify the association of ERM and macular hyaloid fragments.
The vitreous is more firmly attached physiologically at the margin of the optic nerve head, macula, vitreous base, along major retinal vessels, and retinal tufts. Our study results are in accordance with these attachment points. We demonstrated that the most frequent site for residual vitreous cortex is the macula area followed by the disc area. In eyes with partial PVD, the hyaloid may still adhere to the central fovea after paramacular vitreous detachment develops, causing macular traction during eye movement. This is consistent with the OCT finding of early macular hole, where vitreo-retinal adhesion in the foveal area with surrounding posterior vitreous detachment is frequently seen.17, 18
Presently, unless the undetached hyaloid was in connection with the peripheral vitreous, we intentionally refrained from removing the isolated hyaloid fragments. We did find that in some cases the residual membrane could be easily removed with a backflush action of the backflush needle, while in other cases the fragments were more adherent to the underlying retina. These fragments do not seem to prevent good anatomical results. However, we cannot exclude the possibility that residual hyaloid islands become a scaffold for cellular proliferation and PVR membrane formation if recurrent detachment occurs. In addition, in retinal detachment associated with macular hole in a highly myopic eye, isolated cortical vitreous surrounding the hole may prevent long-term reattachment after vitreous surgery. Thus, when retained hyaloid is recognized in the macula area of a highly myopic eye with macular hole, the removal of it during operation may be an adequate manipulation.19
In this study, we documented widespread undetached vitreous connecting with the peripheral vitreous in three patients, although the vitreous was separated from the retina in the posterior pole. We removed the undetached vitreous in all three cases, believing that these extensive vitreous retina adhesion could affect the surgical results. This finding underscores the importance of evaluating the vitreo-retinal relationship in eyes with RD, even when there is apparent PVD.
In conclusion, intravitreal injection of triamcinolone acetonide is an easy and safe way to identify residual cortical vitreous, which is common in eyes with apparent PVD and RRD. The most frequent location for these vitreous islands are the macula and the disc. Further studies with longer follow-up and larger patient series are warranted to evaluate the relationship between residual cortical vitreous and epiretinal membrane.
References
Pischel DK . Detachment of the vitreous as seen with slit-lamp examination. Trans Am Ophthalmol Soc 1952; 50: 329–346.
Buzey SM, Weiter JJ, Furukawa H, Hirokawa H, Tolentino FI, Trempe CL et al. Examination of the vitreous: a comparison of biomicroscopy using the Goldmann and El Bayadi-Kajiura lenses. Ophthalmology 1985; 92: 1745–1748.
Fisher YL, Slakter JS, Friedman RA, Yannuzzi LA . Kinetic ultrasound evaluation of the posterior vitreoretinal interface. Ophthalmology 1991; 98: 1135–1138.
Ortiz RG, Lopez PF, Lambert HM, Sternberg Jr P, Aaberg TM . Examination of macular vitreoretinal interface disorders with monochromatic photography. Am J Ophthalmol 1992; 113(3): 243–247.
Sebag J, Ansari RR . Dynamic light scatteriing detection of posterior vitreous detachment. Proceeding of the SPIE Optical Engineering Society annual meeting, Ophthalmic Technologies, Vol. VIII, January 1998; San Jose, CA, 1998.
Sebag J, Dunker S, Suh KI, Ansari AA . Dynamic light scattering measurements in vitreous. Invest Ophthalmol Vis Sci 1997; 103: 24–28.
Sebag J . Seeing the invisible: the challenge of imaging vitreous. [Reviews]. J Biomed Optics 2004; 9(1): 38–46.
Peyman GA, Cheema R, Conway MD, Fang T . Triamcinolone acetonide as an aid to visualization of the vitreous and the posterior hyaloid during pars plana vitrectomy. Retina 2000; 20(5): 554–555.
Sonoda KH, Enaida H, Ueno A, Nakamura T, Kawano YI, Kubota T et al. Pars plana vitrectomy assisted by triamcinolone acetonide for refractory uveitis: a case series study. Br J Ophthalmol 2003; 87(8): 1010–1014.
Kishi S, Demaria C, Shimizu K . Vitreous remnants at the fovea after spontaneous vitreous detachment. Int Ophthalmol 1986; 9: 253–260.
Kishi S, Koichi S . Oval defect in detachemed posterior hyaloid membrane in idiopathic preretinal macular fibrosis. Am J Ophthalmol 1994; 118: 451–456.
Kishi S . Diagnostic pearls in the management of vitreomacular disorders. Semi Ophthalmol 1998; 13(1): 2–9.
Sonoda KH, Sakamoto T, Enaida H, Miyazaki M, Noda Y, Nakamura T et al. Residual vitreous cortex after surgical posterior vitreous separation visualized by intravitreous Triamcinolone acetonide. Ophthalmology 2004; 111: 226–230.
Kimura H, Kuroda S, Nagata M . Premacular cortical vitreous in patients with a rhegmatogenous retinal detachment. Retina 2004; 24(2): 329–330.
Hikichi T, Takahashi M, Trempe CL, Schepens CL . Relationship between premacular cortical vitreous defects and idiopathic premacular fibrosis. Retina 1995; 15: 413–416.
Wise GN . Relationship of idiopathic preretinal macualr fibrosis to posterior vitreous detachment. Am J Ophthalmol 1975; 79: 358–362.
Altaweel M, Ip M . Macular hole: improved understanding of pathogenesis, staging and management based on optical coherence tomography. [Review]. Semin Ophthalmol 2003; 18(2): 58–66.
Gass JDM . Idiopathic senile macular hole: its early stages and pathogenesis. Arch Ophthalmol 1988; 106: 629–639.
Murata T, Ueno A, Nakamura T et al. Triamcinolone assisted removal of posterior vitreous membrane as an adjuntive treatment for retinal detachment resulting from a macular hole in highly myopic eyes. Invest Ophth Vis Sci 2002; 43: 2493 [E-abstract].
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests: None declared.
Rights and permissions
About this article
Cite this article
Chen, T., Yang, C. & Liu, K. Intravitreal triamcinolone staining observation of residual undetached cortical vitreous after posterior vitreous detachment. Eye 20, 423–427 (2006). https://doi.org/10.1038/sj.eye.6701892
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701892
Keywords
This article is cited by
-
Selective internal limiting membrane peeling for prevention of secondary epiretinal membrane after vitrectomy for rhegmatogenous retinal detachment
Japanese Journal of Ophthalmology (2024)
-
Characteristics and surgery outcomes of macular hole diagnosed after rhegmatogenous retinal detachment repair
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Visual outcome and complications of 25-gauge vitrectomy for rhegmatogenous retinal detachment; 84 consecutive cases
Eye (2010)
-
Visualizing vitreous in vitrectomy by triamcinolone
Graefe's Archive for Clinical and Experimental Ophthalmology (2009)
-
Intravitreal triamcinolone staining observation of residual undetached cortical vitreous after posterior vitreous detachment
Eye (2007)