Abstract
Aims
To assess the efficacy and safety of intravitreal triamcinolone in the treatment of postoperative cystoid macular oedema (CMO).
Methods
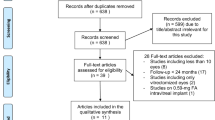
A retrospective case series review of 21 eyes (20 patients) that had an intravitreal injection of triamcinolone 4 mg for postoperative CMO. Diagnosis was confirmed by fundus fluorescein angiography and/or optical coherence tomography in all eyes.
Results
Mean age of patients was 71.1 years. CMO had developed following routine phacoemulsification cataract extraction (13 eyes), phacoemulsification cataract extraction complicated by posterior capsule tear and vitreous loss (two eyes), vitrectomy (three eyes), or planned combined phacoemulsification and vitrectomy (three eyes). Mean duration of CMO before triamcinolone injection was 4.9 months. Mean duration of follow-up was 7.4 months. Two eyes required a repeat injection. Mean logarithm of minimum angle of resolution (LogMAR) visual acuity (VA) before treatment was 0.53; at 1 month post injection, this increased significantly to 0.33 (P<0.001). Improvement in VA was maintained throughout follow-up; at 6 months or later, mean LogMAR VA was significantly better than baseline (0.33 vs 0.53, P=0.02). At the latest review, 43% of eyes had improved Snellen VA by two or more lines and 86% by one or more lines compared to baseline. The remaining 14% had reduced Snellen VA compared to baseline. In the post-injection period, 33% of eyes developed an intraocular pressure of 22 mm Hg or higher and all responded well to short-term topical agents. There were no other post-injection complications.
Conclusion
Intravitreal triamcinolone results in a rapid improvement in VA that may be sustained for more than 6 months.
Similar content being viewed by others
Introduction
Cystoid macular oedema (CMO) is an important cause of reduced vision following cataract and vitreoretinal surgery. The diagnosis of postoperative CMO, especially at subclinical level, has been facilitated by the widespread availability of optical coherence tomography (OCT). Various treatment options have been suggested, including topical corticosteroids, topical non-steroidal anti-inflammatory drugs, systemic carbonic anhydrase inhibitors, and laser photocoagulation.1, 2, 3, 4 The aims of our study were to assess the efficacy and safety of intravitreal triamcinolone acetonide (IVTA) in the treatment of CMO following cataract and vitreoretinal surgery.
Materials and methods
We carried out a retrospective case series review of all IVTA injections that had been carried out for postoperative CMO between August 2002 and December 2004 at Southampton Eye Unit, UK. The procedure had been performed on 21 eyes of 20 patients. All eyes had the diagnosis confirmed by pre-treatment OCT or fundus fluorescein angiography (FFA).
Patients underwent baseline examination, including Snellen visual acuity (VA), slit-lamp biomicroscopy, Goldmann tonometry, and dilated fundus examination. CMO was diagnosed clinically by slit-lamp biomicroscopy and confirmed with either OCT or FFA. The IVTA injections were carried out under aseptic conditions in theatre. Triamcinolone acetonide 4 mg in 0.1 ml (Kenalog, Bristol-Meyers Squibb, Middlesex, United Kingdom) was injected pars plana, 3.0 and 3.5 mm behind the limbus for pseudophakic and phakic individuals, respectively. Topical antibiotics (g. chloramphenicol or oc. chloramphenicol) were used in the postoperative period to the treated eye for 1 week. All patients were asked to attend outpatient review initially at 2–4 weeks and then at 6–8 weeks post treatment. Subsequent reviews were scheduled for 3–5 months and then 6–8 months post treatment, unless there was clinical need for earlier review. Patients experiencing pain or decreased vision were advised to attend before their booked appointment.
Results
This study reviewed 21 eyes of 20 patients (16 male, 4 female). The mean age of patients was 71.1 years (SD 9.9, median 72.5, range 55–93 years). Six patients (30%) were diabetic and seven (35%) were hypertensive. The mean intraocular pressure (IOP) before treatment was 16 mm Hg (SD 3.7, range 10–25, median 16); two eyes had primary open-angle glaucoma, one narrow angle glaucoma, and one pseudo-exfoliation glaucoma, all with an IOP less than 21 mm Hg before the procedure. One eye had a pre-injection IOP of 25 mm Hg following complicated cataract surgery.
Postoperative CMO had developed following routine phacoemulsification cataract extraction (13 eyes), phacoemulsification cataract extraction complicated by posterior capsule tear and vitreous loss (two eyes), vitrectomy (three eyes), or planned combined phacoemulsification and vitrectomy (three eyes). The mean duration of CMO before IVTA injection was 4.9 months (SD 5.0, range 1–24 months, median 4). All eyes had shown a poor response to topical ketorolac 0.5% and/or dexamethasone 0.1%. Mean duration of follow-up after IVTA was 7.4 months (SD 3.9, median 7, range 2–13 months). Two eyes required a repeat IVTA injection; end of follow-up was considered the review just before the repeat injection.
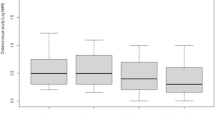
Snellen VA measurements were converted to logarithm of minimum angle of resolution (LogMAR) equivalents in order to facilitate data analysis. Mean LogMAR VA before treatment was 0.53; at 1 month post IVTA injection, this had increased significantly to 0.33 (P<0.001). This improvement in VA remained throughout follow-up; at 6 months or later, mean LogMAR VA was significantly better than baseline (0.33 vs 0.53, P=0.02). At final review, mean LogMAR VA was significantly better than baseline (0.34 vs 0.53, P=0.005). Details of each visit can be seen in Table 1.
At 1 month post IVTA injection, 44% of eyes had Snellen VA improved by two or more lines compared to baseline. At 6 months or later, 50% of eyes maintained such an improvement. Details can be seen in Table 2. At the latest review, 86% of eyes had Snellen VA improved by one or more lines compared to baseline. The remaining 14% had reduced Snellen VA compared to baseline; details can be seen in Table 3.
No intraoperative complications were recorded. In the post-injection period, an IOP of 22 mm Hg or higher was recorded in eight eyes (38.0%). One eye that had raised IOP before the procedure did not show a further increase. IOP elevations were temporary and settled on topical medication. There were no cases of postoperative endophthalmitis or other post-injection complications.
Discussion
Intravitreal triamcinolone has been used successfully to treat macular oedema associated with conditions such as retinal vein occlusion, uveitis, and diabetic maculopathy.5, 6, 7 Small case series have also described a beneficial effect in pseudophakic CMO.8, 9, 10, 11, 12
The pathogenesis of postoperative CMO is unclear. It has been suggested that vitreoretinal traction during ocular surgery may cause a breakdown of the blood retinal barrier, leading to postoperative CMO.13 Increased levels of intraocular prostaglandins after ocular surgery may also be an aetiological factor.14, 15 This would explain the beneficial effect of corticosteroids and non-steroidal anti-inflammatory drugs.1, 8, 9, 10, 11, 12, 15, 16 The exact mechanism of action of triamcinolone remains unclear. Intravitreal steroids have been shown to stabilise the blood retinal barrier in patients that have had laser photocoagulation and to reduce the vitreous concentration of vascular endothelial growth factor.17, 18
In our study, intravitreal triamcinolone was associated with an improvement in vision. Compared to baseline, mean LogMAR VA was improved at all post-injection reviews. The improvement in VA was manifest as early as 1 month following the procedure and remained significantly better than baseline even after 6 months. Nine eyes that had 9 months or more follow-up maintained improved vision compared to baseline (0.28 vs 0.53, P=0.01). The results of our study suggest that for postoperative CMO, the beneficial effect of IVTA on VA may be more long term.
The use of intravitreal triamcinolone for postoperative CMO has been described in small case series of pseudophakic CMO. A long-term sustained effect was reported by Karacorlu et al,9 who described a case series of six eyes that were treated with 4 mg triamcinolone. At 6 months, all six eyes had VA better than baseline. Mean duration of CMO before treatment was 8.7 (range 4–16). Jonas et al10 described a case series of five eyes that were treated with 25 mg triamcinolone. At the end of follow-up (mean 6.6 months), mean VA was better than baseline and according to the authors there was no tendency to suggest a decrease in VA. The time interval since cataract surgery ranged from 3 to 12 months.
Not all studies have supported a sustained effect of intravitreal triamcinolone for postoperative CMO. Boscia et al11 published a series of seven eyes that were treated with 4 mg triamcinolone. Although VA improved transiently after the injection, at the end of the follow-up period (mean 11.2 months) VA and macular thickness were not statistically different to baseline. Mean duration of CMO was 18.3 months (range 6–34 months). Conway et al12 reported a series of eight eyes that were treated with 1 mg triamcinolone. Mean VA at the end of follow-up (mean 8 months) was better than baseline, but all eyes had required repeat injection in order to maintain their improved VA. Mean duration of CMO was 20 months. Duration of CMO in these two series was considerably longer than in our study and the series described above by Jonas and Karacorlu. It appears that intravitreal triamcinolone may produce a better visual outcome in non-chronic CMO. A similar observation was noted in a study looking at the visual outcome of uveitic CMO treated with intravitreal triamcinolone. The greatest visual improvement occurred in eyes with CMO duration of less or equal to 12 months; eyes with CMO duration of more than 24 months improved least.6
In our study three eyes had reduced Snellen VA compared to baseline. Case 1 had cataract extraction complicated by posterior capsule tear; a secondary anterior chamber intraocular lens was implanted 6 weeks later. Postoperative CMO was treated with IVTA 4 months following secondary lens implantation. VA initially improved but then deteriorated at 3 months with recurrence of CMO and epiretinal membrane formation. Case 2 had cataract surgery complicated by posterior capsule tear and nuclear fragment drop. Posterior vitrectomy was carried out concurrently with implantation of a sulcus-fixated lens. Postoperative CMO was treated with IVTA injection 2 months following surgery. VA improved but at 6 months post injection, CMO recurred with a reduction of VA. Case 3 developed CMO following routine cataract extraction. The patient had a history of a retinal vein occlusion and mild diabetic retinopathy. Postoperative CMO was treated with IVTA injection 8 months following surgery. VA improved but at 9 months post injection, his CMO recurred. All three cases had recurrence of CMO confirmed by OCT.
The results of our study need to be interpreted with a degree of caution owing to the uncontrolled nature of the study. In addition, the natural history of postoperative CMO includes spontaneous resolution. Therefore, it could be that in a significant number of eyes VA would have improved anyway given more time. However, the rapid onset in efficacy of intravitreal triamcinolone is notable and clinically significant. One of the features of intravitreal triamcinolone in clinical practice is the reduction of macular oedema within the first month following treatment. Karacorlu et al9 showed that at 1 month post injection of IVTA, macular thickness had decreased from a pre-injection value of 504 to 264 μm.9 In macular oedema associated with diabetes or retinal vein occlusion, VA is significantly better at 1 month following triamcinolone injection.5, 19 It is known that chronic CMO may cause non-reversible macular changes, such as serous macular detachment, retinal pigment epithelial changes, and epiretinal membrane formation.20 In addition, chronic CMO is often refractory to treatment, including intravitreal triamcinolone.9, 10 Prompt treatment of postoperative CMO with IVTA may prevent the development of chronic CMO.
Post-injection elevation of IOP was not a particular problem in our series. Seven eyes (33%) developed an IOP of 22 mm Hg or higher following IVTA and all responded well to topical agents. There is a well-documented association between intravitreal triamcinolone injection and elevation of IOP. The published figure of IOP elevation following IVTA varies from 20.8 to 52% of injected eyes.21, 22
Our study demonstrates that intravitreal triamcinolone injection is an effective treatment option for postoperative CMO. It results in a rapid improvement in VA that may be sustained for more than 6 months. However, it is associated with significant ocular morbidity, including glaucoma and endophthalmitis. A randomised controlled study is needed to compare the efficacy and safety of intravitreal triamcinolone with non-invasive treatment options such as topical agents and/or peri-ocular steroids in this particular group of patients.
References
Suckling RD, Maslin KF . Pseudophakic cystoid macular oedema and its treatment with local steroids. Aust NZ J Ophthalmol 1988; 16: 353–359.
Weisz JM, Bressler NM, Bressler SB, Schachat AP . Ketorolac treatment of pseudophakic cystoid macular oedema identified more than 24 months after cataract extraction. Ophthalmology 1999; 106: 1656–1659.
Cox SN, Hay E, Bird AC . Treatment of chronic macular oedema with acetazolamide. Arch Ophthalmol 1988; 106: 1190–1195.
Lardenoye CWTA, van Schooneveld MJ, Treffers WF, Rothona A . Grid laser photocoagulation for macular oedema in uveitis or the Irvine–Gass syndrome. Br J Ophthalmol 1998; 82: 1013–1016.
Ip MS, Gottlieb JL, Kahana A, Scott IU, Altaweel MM, Blodi BA et al. Intravitreal triamcinolone for treatment of macular oedema associated with central retinal vein occlusion. Arch Ophthalmol 2004; 122: 1131–1136.
Kok H, Lau C, Maycock N, McCluskey P, Lightman S . Outcome of intravitreal triamcinolone in uveitis. Ophthalmology 2005; 112: 1916–1921.
Jonas JB, Kreissig I, Sofker A, Degenring RF . Intravitreal injection of triamcinolone for diffuse diabetic macular oedema. Arch Ophthalmol 2003; 121: 57–61.
Benhamou N, Massin P, Haouchine B, Audren F, Tadayoni R, Gaudric A . Intravitreal triamcinolone for refractory pseudophakic macular oedema. Am J Ophthalmol 2003; 135: 246–249.
Karacorlu M, Ozdemir H, Karacorlu S . Intravitreal triamcinolone acetonide for the treatment of chronic pseudophakic cystoid macular oedema. Acta Ophthalmol Scand 2003; 81: 648–652.
Jonas JB, Kreissig I, Degenring RF . Intravitreal triamcinolone acetonide for pseudophakic cystoid macular oedema. Am J Ophthalmol 2003; 136: 384–386.
Boscia F, Furino C, Dammacco R, Ferreri P, Sborgia L, Sborgia C . Intravitreal triamcinolone acetonide in refractory pseudophakic cystoid macular oedema: functional and anatomic results. Eur J Ophthalmol 2005; 15: 89–95.
Conway MD, Canakis C, Livir-Rallatos C, Peyman GA . Intravitreal triamcinolone acetonide for refractory chronic pseudophakic cystoid macular oedema. J Cataract Refract Surg 2003; 29: 27–33.
Gass JD, Anderson DR, Davis EB . A clinical, fluorescein angiographic and electron microscopic correlation of cystoid macular oedema. Am J Ophthalmol 1985; 100: 82–86.
Flach AJ, Stegman RC, Graham J, Kruger LP . Prophylaxis of aphakic cystoid macular oedema without corticosteroids: a paired-comparison, placebo-controlled, double-masked study. Ophthalmology 1990; 97: 1253–1258.
Solomon LD . Efficacy of topical flurbiprofen and indomethacin in preventing pseudophakic cystoid macular oedema: Flurbiprofen-CME Study Group I. J Cataract Refract Surg 1995; 21: 73–81.
Flach AJ, Jampol LM, Weinberg D, Kraff MC, Yannuzzi LA et al. Improvement in visual acuity in chronic aphakic and pseudophakic cystoid macular oedema after treatment with topical 0.5% ketorolac tromethamine. Am J Ophthalmol 1991; 112: 514–519.
Wilson CA, Berkowitz BA, Sato Y, Ando N, Handa JT, de Juan E Jr . Treatment with intravitreal steroid reduces blood–retinal barrier breakdown due to retinal photocoagulation. Arch Ophthalmol 1992; 110: 1155–1159.
Brooks Jr HL, Caballero Jr S, Newell CK, Steinmetz RL, Watson D, Segal MS et al. Vitreous levels of Vascular Endothelial Growth Factor and Stromal-Derived Factor 1 in patients with diabetic retinopathy and cystoid macular oedema before and after intraocular injection of triamcinolone. Arch Ophthalmol 2004; 122: 1801–1808.
Negi AK, Vernon SA, Lim CS, Owen-Armstrong K . Intravitreal triamcinolone improves vision in eyes with chronic diabetic macular oedema refractory to laser photocoagulation. Eye 2005; 19: 747–751.
Guex-Crosier Y . The pathogenesis and clinical presentation of macular oedema in inflammatory diseases. Doc Ophthalmol 1999; 97: 297–309.
Ozkiris A, Erkilic K . Complications of intravitreal injection of triamcinolone acetonide. Can J Ophthalmol 2005; 40: 63–68.
Jonas JB, Kreissig I, Degenring R . Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol 2003; 87: 24–27.
Author information
Authors and Affiliations
Corresponding author
Additional information
No proprietary interest or funding involved
Rights and permissions
About this article
Cite this article
Konstantopoulos, A., Williams, C. & Luff, A. Outcome of intravitreal triamcinolone acetonide in postoperative cystoid macular oedema. Eye 22, 219–222 (2008). https://doi.org/10.1038/sj.eye.6702582
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702582