Abstract
Purpose
To compare the effect of posterior capsular opacification (PCO) on visual function in patients with monofocal and multifocal intraocular lenses (IOLs).
Methods
Thirty-three consecutive patients with clinically significant PCO, 24 with monofocal, and nine with multifocal IOLs, were recruited. Patients with concurrent cause of visual loss or pupillary distortion were excluded. LogMAR high- and low-contrast (10%) distance visual acuity (VA), logMAR near VA, Pelli–Robson contrast sensitivity (CS), colour confusion index (CCI), and the presenting symptoms were compared between the two groups.
Results
There was no significant difference between the proportions of patient with different PCO grade in the two groups. At presentation, high- and low-contrast distance VA were significantly greater in the multifocal group (0.40 vs0.20; P=0.04 and 0.34 vs0.98; P=0.006), whereas near VA, CS, and CCI were not significantly different between the two groups. After capsulotomy, the above visual functions were not significantly different between the two groups. Blurred distance and near vision were the most common presenting symptoms (95.8 and 100% in the monofocal group and 88.9 and 66.7% in the multifocal group). A greater proportion of patients in the monofocal group had blurred near vision (100 vs66.7%) and, whereas the symptoms in the majority of patients in the monofocal group were moderate to severe, they were mild to moderate in the multifocal group.
Conclusion
The effect of PCO on visual function in the two groups seems to be comparable, although patients in the multifocal group appear to present with earlier loss of visual function.
Similar content being viewed by others
Introduction
Posterior capsular opacification (PCO), by causing forward and backward light scattering, reduces visual acuity (VA) and contrast sensitivity (CS).1, 2, 3, 4, 5 The magnitude of the effect of PCO on visual function was found to be related mainly to its location, density, and type, with epithelial pearls having a more pronounced effect on VA and CS.1, 6, 7
All published studies of the effect of PCO on visual function have been conducted on patients with monofocal intraocular lenses (IOLs). Because multifocal intraocular lens design reduces CS,8, 9 it is not known if this can be exacerbated by the development of PCO, which could lead to an increased rate of Nd:YAG capsulotomy. We hypothesised that the magnitude of PCO-induced impairment of visual function when presenting for Nd:YAG capsulotomy might be different between patients with monofocal and multifocal IOLs.
The aim of this study was to compare the functional impairment in patients with monofocal and multifocal IOLs who presented for Nd:YAG capsulotomy. The results will help in understanding the relative effect of this complication on visual function in the two groups of patients and whether functional loss can potentially be a risk factor for increased Nd:YAG capsulotomy rate.
Patients and methods
This is a prospective nonrandomised case–control study. The appropriate ethical approval was obtained for the study and all eligible patients were informed of the study design and its aims before they gave consent to be included.
Eligibility and inclusion criteria
Fifty-four patients were recruited consecutively from the outpatient clinic at Essex County Hospital, Colchester between April and November 2004. Only the first eye to develop the symptoms for patients who needed bilateral Nd:YAG capsulotomy was included. Patients were considered eligible for inclusion if they had undergone cataract extraction and implantation of either monofocal or multifocal IOLs and were referred because of visual symptoms attributable to PCO and had lost at least one line of Snellen's VA.
Exclusion criteria
Patients with a history suggestive of amblyopia (n=1) or colour blindness (n=1) and those who had glaucoma (n=6), diabetic retinopathy (n=4), neo-vascular or atrophic age-related maculopathy (n=6), or pupillary abnormality (n=3) were excluded, which left 33 patients.
Questionnaire
A questionnaire (Table 1, Table 2) was administered by the examiner during the consultation. It included questions about different PCO-related visual symptoms, including blurred distance and near vision, colour vision, dysphotopic symptoms, or diplopia. Patients were asked to rate the symptoms as mild, moderate, or severe, depending on how much it affected their day-to-day activities. After capsulotomy, the questions were whether the symptoms have disappeared, improved, or got worse and if new symptoms had developed.
Examination
VA, CS, and colour vision were measured by an assistant who was masked to the type of the IOL.
Visual acuity
High-contrast (90%) distance and near best-corrected visual acuities (BCVA) were measured using logMAR charts at 3 m and 40 cm, respectively. The charts were externally illuminated and illumination levels at the charts were 400 lux. The patients were encouraged to read down the charts until they read a whole line incorrectly, (forced choice testing). The acuity was recorded as a logMAR score of the total number of letters that were identified correctly.
Contrast sensitivity
Pelli–Robson and low-contrast (10%) logMAR acuity charts were used to examine CS. Pelli–Robson chart has eight lines of Sloan letters; each subtends a visual angle of 3 degrees at a test distance of 1 m. The letters are arranged in triplets, each progressively decrease in contrast from 96 to 1%. The 10% logMAR acuity chart was tested at 3 m. Both charts were externally illuminated and the illumination levels at their surfaces were approximately 400 and 300 lux, respectively.
Colour vision
All the patients underwent Ishihara test to identify those with congenital colour blindness. Colour vision was then tested using Lanthony desaturated D15 test that was conducted under an additional external illumination of 1000 lux produced by a fluorescent lamp placed at 35 cm from the colour chips. The Colour Vision Recorder software (version 2.3; Optical Diagnostics, Culemborg The Netherlands) was used to record the results and to calculate the colour confusion index (CCI).10 The latter indicates how much the patient's arrangement of the colour chips deviates from the perfect arrangement: an index of 1 indicates a perfect arrangement and a value larger than 1 indicates some colour confusion or error.
Slit lamp examination
This included anterior segment and fundus examination in addition to intraocular pressure measurement.
Determining type and grading of PCO
A single examiner (MAE) determined the PCO type and grade. Because the multifocal design was readily available on clinical examination, masking the examiner to the type of the implant was impossible. PCO was classified clinically into ‘fibrotic’ or ‘cellular’ according to the predominant feature (> 50%) within the retro-optic part of the posterior capsule. PCO grading was carried out after pupillary dilatation and was determined based on the visibility of the posterior segment structures on the slit lamp. A modification of the grading system used by several other authors11, 12, 13, 14 was adopted (Table 2).
Nd:YAG capsulotomy
Before capsulotomy, G. Tropicamide 1% was instilled in the eye to achieve 4–6 mm of pupillary dilation. Also, G. Apraclonidine 0.1% was used before and after the procedure to prevent rise of intraocular pressure. The procedure was preformed using Cooper Vision 2500 (Alcon Inc., Fort North, Texas, USA) machine and 2–4 mJ of energy per pulse that were increased as needed. The laser beam was posteriorly defocused in order to avoid pitting the lens.
After care
After capsulotomy, G. Dexamethasone 0.1% (Maxidex; Alcon Inc.) was prescribed QDS for 1 week and BID for 1 week.
Post-capsulotomy examination and questionnaire
All the patients were reviewed 2–6 weeks. VA, CS, and colour vision were assessed as before and under the same conditions. A questionnaire designed to explore the changes in visual symptoms was administered by the same interviewer. Anterior and posterior segments were examined for adequacy of the capsular opening, clarity of the visual axis, IOL position, signs of inflammation, and the presence of macular oedema.
Statistical analysis
The primary outcome of the study was the difference between the two groups of patients in visual functions, that is, distance and near VA, CS, and CCI, at presentation. The secondary outcome was the difference in the proportion of patients with different PCO-related symptoms in the two groups.
We used the independent t-test or Mann–Whitney test (when the data were not normally distributed) for comparison of continuous data. Fisher's exact test was used for comparing proportions of patients with different PCO-related symptoms. The study had 90% power to detect a 0.2 log units (two lines on the high and low contrast log MAR chart) in the mean preoperative acuity (SD 0.1), of 0.3 of log units of Pelli–Robson CS (one line), and 0.25 in the mean CCI (with a SD of 0.15) at an alpha level of 0.05.
Results
Clinical features
Thirty-three patients were included in the study, 13 of them were men and the median age was 76.2 years (range 18–91 years). Thirty-two of the patients had undergone phacoemulsification and one extracapsular cataract extraction. Twenty-four patients (72.7%) had monofocal IOL, including PMMA: 95UV, Storz, St Louis, MO, USA (refractive index (RI)=1.49) (n=3, 12.6%); Silicone: SI30NB, SI40NB, or Clariflex; Advanced Medical Optics Inc. Irvine, CA, USA (RI=1.46) (n=15, 62.6%); Lenstec LH3000, Lenstec Inc. St Petersberg, Florida, USA (RI=1.4585) (n=5, 25%); or Hydrogel: Li61U Soflex, Bausch & Lomb Claremont, CA, USA (RI=1.427) (n=1, 4.2%). Nine patients (27.3%) had silicone refractive multifocal IOL, Array SA40N, Advanced Medical Optics Inc. (RI=1.46, n=9, 100%).
There was no significant difference in age, gender distribution, PCO type or grade, the time to presentation for capsulotomy, or the spherical equivalent between the two groups (Table 3).
Visual function
At presentation, high- and low-contrast logMAR acuity were significantly better (smaller values) in the multifocal group (0.40 vs 0.20; P=0.04 and 0.34 vs 0.98; P=0.006) (Table 4). On the other hand, near acuity, Pelli–Robson CS, and CCI were not significantly different between the two groups. After capsulotomy, high- and low-contrast distance and near VA, Pelli–Robson CS, and CCI were not significantly different between the two groups (Table 4).
Questionnaire results
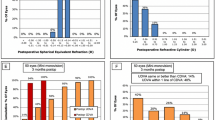
The presenting symptoms (Table 5 and Figure 1) in the majority of patients in the two groups were blurred distance or near vision (95.8 and 100% in the monofocal group and 88.9 and 66.7% in the multifocal group). Glare and halos affected 45.8 and 25% of patients in the monofocal group and each affected 44.4% of patients in the multifocal group. Other dysphotopic symptoms such as seeing stars/streaks/flare; and other symptoms such as double vision and floaters affected a smaller proportion of patients in the two groups (Table 5). A significantly greater proportion of patients in the monofocal group had blurred near vision (100 vs 66.7%; Fisher's exact; P=0.01). There was no statistically significant difference between the proportions of patients affected by the other symptoms in the two groups. Whereas all the symptoms in the majority of patients in the monofocal group were moderate to severe, in the majority of patients in the multifocal group they were mild to moderate (Table 5).
After capsulotomy, Table 6 shows that all patients in the monofocal group experienced improvement or complete disappearance of their symptoms. One of the patients in the multifocal group (12.5%) had persistent symptoms of blurred distance and near vision and another (12.5%) had persistent glare and halos. Also, 19 and 25% of the monofocal and multifocal group, respectively, reported seeing floaters that was graded as mild by all the patients.
Discussion
Several studies have shown that patients with monofocal and multifocal IOLs have comparable visual functions and that the effect of the multifocal lens design on visual function is limited and clinically insignificant.15, 16, 17, 18, 19, 20 In this study, we compared the presenting visual functions between two groups of patients who had either monofocal or multifocal IOLs and presented with PCO and needed Nd:YAG capsulotomy with view to relating that to a possible effect on Nd:YAG capsulotomy rate. We showed that while near BCVA, Pelli-Robson CS and CCI were not significantly different at presentation in the two groups, high- and low-contrast acuity values were significantly greater in the multifocal group. After Nd:YAG capsulotomy, all visual functions were comparable in the two groups.
Hayashi et al,3 in a study of the effect of PCO on visual functions, showed that VA had a stronger association with PCO than CS or glare sensitivity. Other studies of the effect of PCO on CS2, 5 have shown that patients predominantly suffer a global loss over all spatial frequencies. Cheng et al,1 however, showed a preferential loss at low- to intermediate spatial frequency (6 c.p.d). Our findings suggest that logMAR acuity charts (of high and low contrast), perhaps by displaying a wider range of spatial frequencies21 (Figure 2), are probably more sensitive in detecting PCO-related differences and differences between the two IOL groups than other charts.
The relationship between different letter-based test charts and CS (courtesy of T. Adams).19
There are two explanations for the difference found between the two groups: either that patients with multifocal IOLs were referred earlier for Nd:YAG capsulotomy or that these patients were less tolerant to PCO-induced functional loss. Against the first proposition is the fact that there was no significant difference between the time to capsulotomy between the two groups. Also, the two groups had comparable precapsulotomy clinical features, including their PCO type (cellular or fibrotic) and grade. Even if these patients had been referred sooner, that would have been upon their request, which rather supports the latter proposition. More in favour of this proposition is the consistently smaller values of the mean gain in visual functions in the multifocal group (0.33 log units for high-contrast acuity, 0.24 log units for Pelli–Robson CS, and 0.12 log units for low-contrast acuity vs 0.54, 0.48, and 0.88) (Table 4). Moreover, the presenting symptoms in the multifocal group were predominantly mild or moderate, whereas in the monofocal group they were moderate or severe. Notably, although the symptoms in the two groups were generally comparable, more patients in the monofocal group had difficulty with reading than those in multifocal group. This, in addition to further suggesting earlier presentation of these patients, could be related to the enhancement of near vision performance achieved by the added power of the multifocal IOL. In a previous study of bifocal IOLs (3M/Vision Care, St Paul, MN, USA), Gimbel et al22 suggested that patients with other causes of visual loss, including PCO, might find the loss in contrast sensitivity additive.
CCI showed the least change of all visual functions, indicating that colour vision is perhaps more resistant to PCO-induced blur. This is consistent with the evidence suggesting that colour vision is resistant to different forms of blur, including optical blur23, 24 and that resulting from medial opacities such as cataract.25
After capsulotomy, the majority of patients in the two groups experienced improvement or disappearance of their symptoms. One patient (12.5%) with multifocal IOL experienced persistent glare or halos and another experienced persistent blurring of vision, without any clinically evident cause. A small percentage in each group (19 and 25%, respectively) developed floaters, but all patients reported that to be mild and not affecting their vision.
It was not possible to compare the survival time between the two groups of patients nor between those in the subgroups with different PCO types and grades because of the small sample size and the absence of a control group who did not have PCO or require Nd:YAG capsulotomy. A similarly designed study with a larger sample size and a contemporary control group will enable further assessment of the incidences in patients with different types of PCO.
In conclusion, this study suggests that patients with multifocal IOLs present for Nd:YAG capsulotomy with a lesser magnitude of functional impairment, which mainly affects high- and low-contrast acuity. This perhaps reflects more vision consciousness or sensitivity to early functional loss and could lead to a higher rate of Nd:YAG capsulotomy in these patients. This information should help in patient counselling and the planning of their follow-up.
References
Cheng CY, Yen MY, Chen SJ, Kao SC, Hsu WM, Liu JH et al. Visual acuity and contrast sensitivity in different types of posterior capsule opacification. J Cataract Refract Surg 2001; 27: 1055–1060.
Meacock WR, Spalton DJ, Boyce J, Marshall J . The effect of posterior capsule opacification on visual function. Invest Ophthalmol Vis Sci 2003; 44: 4665–4669.
Hayashi K, Hayashi H, Nakao F, Hayashi F . Correlation between posterior capsule opacification and visual function before and after neodymium: YAG laser posterior capsulotomy. Am J Ophthalmol 2003; 136: 720–726.
Magno BV, Datiles MB, Lasa MS, Fajardo MR, Caruso RC, Kaiser-Kupfer ML et al. Evaluation of visual function following neodymium:YAG laser posterior capsulotomy. Ophthalmology 1997; 104: 1287–1293.
Tan JC, Spalton DJ, Arden GB . The effect of neodymium: YAG capsulotomy on contrast sensitivity and the evaluation of methods for its assessment. Ophthalmology 1999; 106: 703–709.
Aslam TM, Aspinall P, Dhillon B . Posterior capsule morphology determinants of visual function. Graefes Arch Clin Exp Ophthalmol 2003; 241: 208–212.
Aslam TM, Patton N . Methods of assessment of patients for Nd:YAG laser capsulotomy that correlate with final visual improvement. BMC Ophthalmol 2004; 4: 13.
Haring G, Dick HB, Krummenauer F, Weissmantel U, Kroncke W . Subjective photic phenomena with refractive multifocal and monofocal intraocular lenses. Results of a multicenter questionnaire. J Cataract Refract Surg 2001; 27: 245–249.
Leyland M, Zinicola E . Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology 2003; 110: 1789–1798.
Bowman KJ . A method for quantitative scoring of the Farnsworth Panel D-15. Acta Ophthalmol (Copenhagen) 1982; 60: 907–916.
Aslam TM, Dhillon B . Neodymium:YAG laser capsulotomy: a clinical morphological analysis. Graefes Arch Clin Exp Ophthalmol 2002; 240: 972–976.
Kucuksumer Y, Bayraktar S, Sahin S, Yilmaz OF . Posterior capsule opacification 3 years after implantation of an AcrySof and a MemoryLens in fellow eyes. J Cataract Refract Surg 2000; 26: 1176–1182.
Kruger AJ, Schauersberger J, Abela C, Schild G, Amon M . Two year results: sharp versus rounded optic edges on silicone lenses. J Cataract Refract Surg 2000; 26: 566–570.
Sellman TR, Lindstrom RL . Effect of a plano-convex posterior chamber lens on capsular opacification from Elschnig pearl formation. J Cataract Refract Surg 1988; 14: 68–72.
Javitt J, Brauweiler HP, Jacobi KW, Kelmen U, Kohnen S, Quentin CD et al. Cataract extraction with multifocal intraocular lens implantation: clinical, functional, and quality-of-life outcomes. Multicenter clinical trial in Germany and Austria. J Cataract Refract Surg 2000; 26: 1356–1366.
Javitt JC, Steinert RF . Cataract extraction with multifocal intraocular lens implantation: a multinational clinical trial evaluating clinical, functional, and quality-of-life outcomes. Ophthalmology 2000; 107: 2040–2048.
Steinert RF, Aker BL, Trentacost DJ, Smith PJ, Tarantino N . A prospective comparative study of the AMO ARRAY zonal-progressive multifocal silicone intraocular lens and a monofocal intraocular lens. Ophthalmology 1999; 106: 1243–1255.
Vaquero M, Encinas JL, Jimenez F . Visual function with monofocal versus multifocal IOLs. J Cataract Refract Surg 1996; 22: 1222–1225.
Arens B, Freudenthaler N, Quentin CD . Binocular function after bilateral implantation of monofocal and refractive multifocal intraocular lenses. J Cataract Refract Surg 1999; 25: 399–404.
Elgohary MA, Beckingsale AB . Effect of illumination on visual function of multifocal and monofocal IOLs. Eye 2006; 20: 144–149.
Adams AJ . Impact of new and emerging instrumentation in optometry. Optom Vis Sci 1993; 70: 272–278.
Gimbel HV, Sanders DR, Raanan MG . Visual and refractive results of multifocal intraocular lenses. Ophthalmology 1991; 98: 881–887.
Mantyjarvi M, Tuppurainen K . Colour vision and dark adaptation in high myopia without central retinal degeneration. Br J Ophthalmol 1995; 79: 105–108.
Degen RL, Mullane SD, Richards OW . Variation of the green–red ratio with refractive error. Am J Optom Physiol Opt 1983; 60: 151–152.
Pinckers A . Color vision and age. Ophthalmologica 1980; 181: 23–30.
Acknowledgements
We thank Miss Michelle Bradley at the Department of Epidemiology and Public Health, Cambridge University, for the statistical advice and consultation and Mrs Jocelyn Murphy at Essex County Hospital for her help with the patient examination and recruitment.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presentation: as a poster at the Royal College of Ophthalmology Annual Congress, Birmingham, May 2005 Proprietary interests: None Financial support: None
Rights and permissions
About this article
Cite this article
Elgohary, M., Beckingsale, A. Effect of posterior capsular opacification on visual function in patients with monofocal and multifocal intraocular lenses. Eye 22, 613–619 (2008). https://doi.org/10.1038/sj.eye.6702661
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702661
Keywords
This article is cited by
-
Presbyopic lens exchange (PRELEX) cataract surgery outcomes with implantation of a rotationally asymmetric refractive multifocal intraocular lens: femtosecond laser-assisted versus manual phacoemulsification
International Ophthalmology (2019)
-
Primary posterior continuous curvilinear capsulorhexis combined with diffractive multifocal intraocular lens implantation
Eye (2016)
-
Bilateral implantation of multifocal versus monofocal intraocular lens in children above 5 years of age
Graefe's Archive for Clinical and Experimental Ophthalmology (2014)
-
Five-year postoperative outcomes of apodized diffractive multifocal intraocular lens implantation
Japanese Journal of Ophthalmology (2013)