Abstract
Aim
To investigate and correlate the corneal, refractive, topographic and familial characteristics of a large cohort with keratoconus.
Methods
Prospective observational study of 200 consecutive patients presenting with keratoconus during the 4 year-period 1997–2000. Subjects were examined at enrolment and at a final review. Data were collected on demographic characteristics, referral route, symptoms, refractive correction, eye rubbing, family history, medical history, slit-lamp biomicroscopic corneal signs, and computerized corneal topography.
Results
Mean age at enrolment was 30.9±10.4 (range, 12.2–72) years (N=200, 62.5% male, 93% white Caucasian) with a 5% family history of keratoconus. Atopic diseases included asthma (23%), eczema (14%), and hay fever (30%). Only 9% wore contact lenses before referral. Mean follow-up was 1004 days ±282 (range, 390–1335) and 9.7±8.9 (range, 1.1–60) years from diagnosis. The mean simulated K1 corneal power at enrolment was 51.74±5.36 (range, 42.59–67.32) D and 88.5% exhibited bilateral keratoconus. Fifty-three (15%) topographically confirmed cones exhibited no clinical corneal signs at presentation. At enrollment, 56% had a pachymetry <0.480 mm increasing to 77% at final review. Forty-eight percent of subjects reported significant eye rubbing and there was a highly statistically significant difference (two sample t-test P=0.018) between keratoconus and control groups. TMS-2 axial corneal power was strongly associated with corneal scarring and age at diagnosis. The size of the scarring effect was 2.2 D (95% confidence interval (CI) 1.34, 3.06).
Conclusions
This study provides an overview of a large population with keratoconus highlighting presenting features and clinical and topographic progression over a 4 year-period.
Similar content being viewed by others
Introduction
Although keratoconus is a relatively common ectatic disease of the cornea, there is a surprising lack of large, prospective, longitudinal studies of the disease. Indeed, to the authors' knowledge, currently, the USA-based Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study is the only major study reported within the literature and the Dundee University Scottish Keratoconus Study (DUSKS), which we report herein, is the only established longitudinal prospective evaluation of keratoconus in the UK. However, there are three major differences between the DUSKS and the CLEK studies.
First, the CLEK dataset is multi-center representing an amalgamation of several baseline papers,1, 2, 3, 4, 5 secondly, a major difference in diagnostic criteria between the DUSKS and CLEK studies is that DUSKS includes analysis of computerised corneal topography and pachymetry, and finally, the keratoconic populations are different, with the higher proportion of ethnic populations in the CLEK study potentially influencing all cited factors.6
The aims of the DUSKS project were to investigate and correlate the corneal, refractive, topographic, and familial characteristics of people with keratoconus, within the Tayside region of Scotland.
Methods
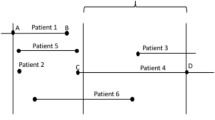
This prospective observational study was based within the corneal and anterior segment service within the Department of Ophthalmology, University of Dundee, Ninewells Hospital and Medical School (catchment population area approximately 426 000). The study was approved by the Tayside Research Ethics Committee. In total, 275 consecutive patients with keratoconus were identified and assessed during the 4-year study period (1997–2000) and, following informed consent, 200 of those subjects were enroled into DUSKS. All subjects either demonstrated corneal signs and/or corneal topographic signs of keratoconus (Tomey TMS™-2 Bausch & Lomb) and the diagnosis was confirmed by a corneal subspecialist.
Each subject was examined at the time of enrolment (baseline review 1) and at a final review (review 2). Data were collected on demographic characteristics (gender, age, occupation, ethnicity, mother's age at birth, handedness, driving ability), referral route to the Hospital Eye Service, symptoms on referral, mode of refractive correction before referral, age at diagnosis, age at enrolment, eye rubbing, family history of keratoconus, and medical history (eczema, hay fever, asthma, cardiac, and joint problems), slit-lamp biomicroscopic corneal findings (Fleischer's ring, Vogt's striae, scarring, prominent corneal nerves, and corneal staining), corneal thickness (Orbscan™ Bausch & Lomb), and topographic classification using the TMS-2 (axial power).
A control group was established for comparison (anonymous questionnaire was used—Appendix 1) in relation to data acquired from questions in relation to systemic diseases, environmental factors, and eye rubbing. The control group constituted 100 subjects randomly recruited from visitors to Ninewells Hospital and was not matched in relation to age, gender, or refractive correction. The only contra-indications to inclusion were previous attendance at an Ophthalmology department or a family history of eye disease.
Statistical analysis
The sign test was used to investigate changes between the first and second clinical reviews in relation to corneal power and thickness. This test requires no assumptions of symmetry or normality in the distribution of changes. The χ2 test for independence of categorical variables in a 2-way contingency table was performed to investigate the presence of an association between asthma, hayfever, eczema, incidence, and amount of eye rubbing or cone steepness. Pearson correlation coefficients were used to assess the strength of association among the continuous measurements of Orbscan corneal power, TMS corneal power, and corneal thickness. Multiple linear regression was used to identify which variables, for example scarring, asthma, eye rubbing, and gender, had statistically important effects on the age of diagnosis and TMS corneal power.
Results
Baseline data
A total of 200 subjects with keratoconus were enroled during the study period. The mean age at enrolment was 30.9±10.4 (range, 12.2–72, median 30.1) years old for all subjects (n=200). There was a higher percentage of male subjects (62.5%) than female subjects. The majority of subjects (93%) were white Caucasian (Asians 6.5%, Afro-Caribbean 0.5%).
Twenty-one subjects had undergone penetrating keratoplasty (PKP) before enrolment. The study group that suffered from asthma was 23%, 14% suffered from eczema, and 30% from hayfever. One female subject had Turner's syndrome. The mean age of the subjects' mothers, at the time of the subjects' birth, was 27.47±5.99 (range, 17–43, median 26) years old. There was a family history of keratoconus in one or more family members in 5% of DUSKS subjects, although amongst the small Asian (Indian sub-continent) subgroup, this rose to 25%.
The mean age of diagnosis by the Hospital Eye Service (HES) was 24.05±8.97 (range, 10–59, median 21.8) years old. The percentage of subjects diagnosed over 40 years of age was 7.5%. There was a trend (which did not reach statistical significance—P=0.07) of the male mean age of diagnosis (23.5±9.2, range, 10–59, median 21 years old) being younger than that for female subjects (24.9±8.5, range, 12–45.11, median 23 years old).
Optometrists referred the majority of subjects to the HES (79%), with the most reported symptom being blurred vision (93%). Other reasons for referral were frequent changes of spectacles (21%), poor visual acuity with spectacles (41%), and sensitivity to light (35%). In nearly two-thirds of the subjects, the mode of correction before referral was spectacles (63.5%, mean length of wear 8.9±8, range, 1–30 years) with only 9% wearing contact lenses, the majority of which were soft lenses (72%, mean length of wear 5.2±2.7, range, 2–12 years). The most prevalent occupation (21%) was that of a trades person (e.g. joiner, carpet fitter), with administration close behind (20%). Thereafter, 9% of keratoconics were managers and 7% were students, with 4% each being engineers, salesmen, social workers, accountants, and housewives. Three percent were farmers and 2% each were teachers, lecturers, waiters, computer engineers, laboratory technicians, cooks, and shop owners. Only 2% of keratoconics were unemployed and 19% reported not holding a driving licence.
The mean follow-up was 1004 days ±282 (range, 390–1335, median 1035). Eighteen (9%) failed to achieve 1-year follow-up (7 female subjects and 11 male subjects) and therefore, did not have the ‘review 2’ data analysed. The mean length of time from diagnosis of keratoconus to the end of the study was 9.7±8.9 (range, 1.1–60 years, median 7.3) years.
Corneal topography
The mean SimK1 corneal power for keratoconic eyes at review 1 (enrolment) was 51.74±5.36 (range, 42.59–67.32, median 50.93) D. Bilateral keratoconus was present in 88.5% of subjects with the inferior (67%) oval cone (75%) classification being the most common (% varying with corneal topography scale used).
Corneal signs
The most frequently observed sign within classified cones was of a Fleischer's ring at review 1 (76%) and at review 2 (79%). Fifty-three (15%) classified cones exhibited no corneal signs at review 1 and 39 cones (12%) at review 2. Scarring was associated most frequently with a central (45, 29%, review 1 and 2, respectively) globus cone (62, 71%, review 1 and 2, respectively). There was an increasing prevalence of scarring with increasing corneal power (TMS-2 axial), as shown in Table 1. Of the 22 cones recorded as unclassified throughout the study, 82% were associated with scarring.
Minor corneal staining, usually at the 3 and 9 o'clock or central position, was seen in 59% of contact lens wearers at the final review. Hurricane type keratopathy (fluorescein whorl pattern of superficial epithelial punctate keratopathy) was recorded in 4%. Evidence of foreign body staining was noted in 18% at the final review, which appeared to be related to a manual occupation (78%). Identification of prominent corneal nerves between reviews increased, these being present in 11% of eyes at review 1 increasing to 18% at review 2. There were no signs of corneal hydrops.
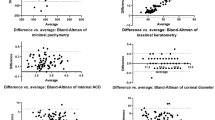
The mean corneal thickness for all affected eyes at review 1 (n=310) was 0.443 (range, 0.229–0.586, median 0.456) mm and at review 2 (n=302) was 0.412 (range, 0.430–0.575, median 0.430) mm. The Orbscan meridional directions of the mean thinnest point was found to be 221 (mean deviation 25.5) and 315 (mean deviation 36.2) degrees for the right and left eye, respectively, at review 1 (both eyes n=326). At review 2, the Orbscan meridional directions of the mean thinnest point was found to be similar within the inferio-temporal quadrant, for the right and left eye, respectively 233, (mean deviation 35.6) and 313 (mean deviation 29.5) degrees (both eyes n=326). The proportion of subjects with corneal thickness less than 0.480 was 56% at enrollment and 77% at the final review. Corneal thickness decreased significantly (P=0.008 for the right eye and P=0.016 for the left eye), from reviews 1 to 2 in keratoconic eyes. There is a correlation of approximately 0.6 (Pearson) between corneal power (TMS-2 axial) and corneal thickness (Orbscan), demonstrating a trend but not statistical significance.
Questionnaire responses: asthma, hay fever, eczema, and eye rubbing
The control group consisted of 38 male subjects and 62 female subjects, of whom 19% wore contact lenses (6% rigid gas permeable). The mean age was 39.23±18.6 (range, 18–77) years old. The prevalence of asthma, hay fever, and eczema was 6, 16, and 16%, respectively, and 91% were right-handed. The most frequent occupation was that of a student, followed by retired persons.
Only 11% of DUSKS subjects reported never rubbing their eyes and 48% reported either frequently or a great deal, whereas for the controls, only 4% reported never and 39% reported either frequently or a great deal. However, only 22.3% of the control group placed a mark over the 50 mm half-way mark on the visual analogue scale. In respect to reported eye rubbing, when using the visual analogue scale, there was a highly statistically significant difference (two sample t-test P=0.018) between the control group and the keratoconus group, with the latter group rubbing their eyes more. However, when using the ‘closed question’ methodology to investigate the self-reported frequency of eye rubbing, this did not reach statistical significant difference between the two groups (Appendix 1).
Although there is no apparent consistent pattern in relation to the mean age at diagnosis, gender, and eye rubbing, there appeared to be a complex interaction effect. The earlier diagnosed males tended to report rubbing their eyes more than females. Most (85.5%) DUSKS subjects were right–handed; however, the steepest cone (using the CVK TMS-2 axial maps) was found in the left eye in 44.5% of cases at review 1. In 16 of the subjects, there was no obvious difference in the bilateral expression of the disease at the time of initial presentation.
When comparing the prevalence of asthma, hayfever, and eczema between the control group and the keratoconus group (23, 30 and 14%, respectively), the latter group had a statistically higher prevalence of hayfever (χ2 analysis P=0.007) and asthma (χ2 analysis P=0.0002). Asthma, hayfever, or eczema keratoconic sufferers tended to rub their eyes more frequently (χ2 test 26.87 df 4, 73.61 df4, 26.03 df 4, respectively). However, when compared with corneal power (TMS-2), there was no significant association with any of the atopic populations (χ2 test 4.02 df 3, 0.969 df3, 0.691 df 3, respectively).
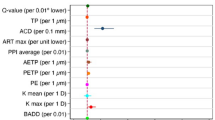
Multiple regression analysis
TMS-2 axial corneal power is strongly associated with the presence of scarring and age of diagnosis. The size of the scarring effect is 2.2 D (95% confidence interval (CI) 1.34, 3.06); that is, the power in eyes with scarring is 2.2 D higher than in eyes with no scarring (adjusting for the subject's age). For an increase in 1 D in power the odds in favour of scarring rise by a factor of 1.21 or 21% (95% CI 1.12, 1.30).
The effect of age at diagnosis is a decrease in power of about 1.5 D per decade (95% CI: 0.7, 2.3) or every 1 D increase in power was associated with a reduction in age at diagnosis of about 0.44 years (95% CI: 0.21, 0.66). There was a noticeable effect associated with the presence of asthma, with the age of diagnosis for those with asthma being on average 3.1 years earlier than those without asthma (95% CI:0.1, 6.2).
Discussion
The current, DUSKS, study tends to add to the weight of evidence1, 7, 8, 9 that a higher percentage of males are diagnosed with keratoconus (DUSKS 62.5%) with an underlying trend of being diagnosed earlier.10, 11 Comparisons between CLEK and DUSKS is shown in Table 2. The mean age at diagnosis of keratoconus is typically within the second or early third decade of life11, 12, 13 (DUSKS and CLEK2 24 and 27 years old, respectively), although, only a small proportion of keratoconics are newly diagnosed after 40 years of age (DUSKS 7.5%, CLEK 10.1%2).
Older keratoconics are under-represented in studies of keratoconus and with only 4% of DUSKS subjects being older than 49 years (CLEK2 12%, Lass et al.11 10%) and yet only 15% had undergone PKP. As the mortality rate of keratoconics is similar to the normal population14 and most do not undergo surgery,15 the majority should be wearing contact lenses beyond their 50s. However, as keratoconics demonstrate periods of stability 8–12 years post diagnosis,16 older individuals may be managed more frequently by community Optometrists and hence their relative under-representation.
The majority of DUSKS subjects were referred to the HES via Optometrists (79%), presenting with similar symptoms (blurred vision, poor visual acuity with spectacles, frequent changes of spectacles and sensitivity to light), as reported previously within the literature.17, 18 Surprisingly, 26.5% of subjects attended the HES with no visual correction and only 9% had previous contact lens wear. The majority (98%) of DUSKS subjects were employed (41% were in either manual or administrative occupations) and most held a drivers licence (81%).
Mother's age has an increasing effect on genetic conditions such as Down's syndrome, which has a strong association with keratoconus.19 The mean age of the DUSKS subjects' mothers at their births was 27.47 years old. The only genetic association within DUSKS was a case of Turners syndrome, a known association.20 The percentage of patients citing a family history of keratoconus varies from 6 to 23.5%,1, 7, 8, 16, 21, 22 only 5% reported a family history in the current study (25% within the small Asian subgroup). Ethnic differences in the prevalence of keratoconus have been well documented.6, 21
Keratoconus is usually a bilateral condition,23 although asymmetrical,24, 25 with the second eye lagging about 5 years behind the first.26 In DUSKS, 88.5% were found to exhibit bilateral keratoconus, usually asymmetrical in presentation (P=0.005). Fleischer's-ring was the most frequently observed corneal sign (86–89%) as reported previously2, 27 followed by Vogt's striae (67–68%) and corneal scarring (21–20%) at review 1 and 2, respectively. Notably, corneal slit-lamp signs cannot be relied upon solely as diagnostic criteria as approximately 15% of eyes exhibited no corneal signs despite pathognomonic topographic signs of keratoconus.
An interesting correlation was identified between corneal power and the presence of corneal scarring. Utilising multiple regression analysis, the scarring effect on corneal power is noted to be approximately 2.2 D; that is, the power in eyes with scarring is 2.2 D higher than in keratoconic eyes without scarring. The CLEK study reported a higher prevalence of corneal scarring (36.6%3) than DUSKS but also noted that scarring was associated with increased corneal power.28 In DUSKS, corneal staining was evident in 71% of eyes at review 2 but appeared to be primarily related to either contact lens wear or foreign bodies. Although RGP contact lens wearers are more vulnerable to 3 and 9 o'clock staining,29 corneal staining can occur even in noncontact lens wearers30 as well as soft contact lens wearers.31
Orbscan has been investigated with regard to the pachymetry of ‘normal’ corneas and demonstrated to measure these as thicker (23–28 μm)32, 33 than comparable ultrasound measurements. However, Orbscan is noninvasive34 and more reproducible than ultrasound and optical pachymetry.35 The mean corneal apex thickness in DUSKS reduced significantly from 0.443 to 0.412 mm at review 2 (mean 1004 days). Both data points are comparable to measurements (mean 0.434) reported in the literature.36 A weak correlation between corneal thickness and corneal power (r-value 0.6) was identified. Watters and Owens37 have suggested a pachymetry threshold of 480 microns as a key diagnostic descriptor of keratoconus. Within DUSKS, 77% of keratoconic corneas were thinner than 480 microns at the second review. Owing to the wide-field pachymetry map produced by Orbscan, unlike ultrasound, it is possible to identify the thinnest area of the cornea. In DUSKS, this thinnest area was most commonly identified as the inferior quadrant (69.6% inferior temporal) as in other studies.23, 38, 39
A proposed external pressure trigger for keratoconus development is previous rigid contact lens wear;40 however, in this keratoconus population within the small group who wore contact lenses (9%), the majority (72%) had worn soft contact lenses before referral. Previously, the high percentage of subjects with a history of RGP contact lens wear before referral to the HES was thought to be due to the better optical correction of subclinical keratoconics using RGP in comparison with soft lenses. However, owing to the high prevalence of soft contact lenses fitted within the community41 and greater detection of keratoconus, this factor may increasingly lose validity as a strong association.
Another trigger mechanism could be eye rubbing.42 Within DUSKS 89% (CLEK reported 50.5%1) of subjects reporting eye rubbing, almost half (48%) confirmed this occurred frequently or a great deal. Although DUSKS subjects tended to rub their eyes more frequently, this did not correlate with a significant association with the axial corneal power in these subjects, and hand dominance and steepness of the cone did not reveal any statistical correlation.
Visual analogue scales represent a simple technique for measuring subjective experience and have been established as being valid and reliable.43 In DUSKS, using visual analogue scales (Appendix 1) to describe eye rubbing history, a statistically significant difference was identified between enroled subjects and a normal control population (19% wearing contact lenses), with keratoconics rubbing their eyes more frequently. However, by comparison, the closed questionnaire technique demonstrated a trend but no statistically significant difference. A general limitation of all eye-rubbing studies is that the force is not measured, only the frequency. Other factors to consider are the method of rubbing (knuckle or finger pads), duration, and seasonal variations.
The control group for the questionnaire component of this study was randomly selected from those attending Ninewells hospital. Although relevant systemic conditions such as asthma, hayfever, eczema, and atopy typically manifest before the third decade, and therefore the prevalence already established in both groups, it should be noted that one of the potential limitations of this questionnaire study is that the control group were, on average, 8 years older (39.23 years) and had a female gender preponderance compared with the study population’.
The variability in the subjective reporting causes additional difficulties in comparing studies. McMonnies and Boneham44 recently published an eye-rubbing study using visual analogue scales and reported that the control group (RGP wearers) rubbed their eyes significantly less than the keratoconic group (n=53), which is similar to the observations in DUSKS. In 12 out of the 17 subjects who rubbed their eyes the most, the hand dominance and the more advanced eye were significantly related; however, these authors also reported that keratoconus developed in subjects with no history of severe rubbing.44
There also appears to be a link between keratoconus and atopy1, 45 with a higher proportion of asthma,46 eczema,12, 47 and hayfever13, 48 sufferers within a keratoconic population. The prevalence of allergic disease is increasing with environmental causes cited as responsible for this rising trend.48 Although the exact nature of the association between atopy and keratoconus is unclear, the frequency of their co-existence does seem to suggest this is not a chance observation. When DUSKS subjects were compared with the control group, there was a statistically higher prevalence of hay fever and asthma within the keratoconic population. Comparing the DUSKS and CLEK study,1 the latter reported a lower history of asthma (14.9%) and eczema (8.4%), with a higher percentage of hayfever (52.9%) and atopic history (53%). Using multiple regression analysis, there was a noticeable effect of the presence of asthma and age at diagnosis of keratoconus, with asthmatics being diagnosed on average 3.1 years earlier within the DUSKS group.
Conclusion
The DUSKS project provides a clear panorama of keratoconus, including presentation, management, and associations, in a large Scottish cohort. These initial DUSKS data have demonstrated that the majority of keratoconics are: referred by Optometrists to the HES with symptoms of blurred vision; male subjects; employed and holding a driving licence; reporting a high prevalence of atopic history and eye rubbing, but a low percentage of family history, generally diagnosed in the latter part of the second decade of life with the younger age at diagnosis being affected by higher corneal power and the co-existence of asthma. Additionally, the most common corneal slit-lamp sign is Fleischers'ring, with the incidence of corneal scarring increasing with steepening corneal power. Corneal thickness reduced significantly over the study period.
References
Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT et al. Baseline findings in the collaborative longitudinal evaluation of keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci 1998; 39: 2537–2546.
Zadnik K, Barr JT, Gordon MO, Edrington TB . Biomicroscopic signs and disease severity in keratoconus. Cornea 1996; 15 (2): 139–146.
Szczotka LB, Barr JT, Zadnik K . A summary of the findings from the collaborative longitudinal evaluation of keratoconus (CLEK) study. Optometry 2001; 72 (9): 574–584.
Barr JT, Zadnik K, Wilson BS, Edrington TB, Everett DF, Fink BA et al. Factors associated with corneal scarring in the collaborative longitudinal evaluation of keratoconus (CLEK) study. Cornea 2000; 19 (4): 501–507.
Zadnik K, Barr JT, Edrington TB . Corneal scarring and vision in keratoconus. A baseline report from the Collaborative longitudinal evaluationof keratoconus study (CLEK). Cornea 2000; 19 (6): 804–812.
Georgiou T, Funnell CL, Cassels-Brown A, O'Conor R . Influence of ethnic origin on the incidence of keratoconus and associated atopic disease in Asians and white patients. Eye 2004; 18: 379–383.
Ihalainen A . Clinical and epidemiological features of keratoconus: genetic and external factors in the pathogenesis of the disease. Acta Ophthalmol 1986; 178: 1–64.
Owens H, Gamble G . A profile of keratoconus in New Zealand. Cornea 2003; 22 (2): 122–125.
Crews MJ, Driebe WT, Stern GA . The clinical management of keratoconus: a 6 year retrospective study. CLAO 1994; 20: 194–197.
Tuft SJ, Moodaley LC, Gregory WM, Davison CR, Buckley RJ . Prognostic factors for the progression of keratoconus. Ophthalmology 1994; 101: 439–447.
Lass JH, Lembach RG, Park SB, Hom DL, Fritz ME, Svilar GM et al. Clinical management of keratoconus. A multicentre analysis. Ophthalmology 1990; 97: 433–445.
Krachmer JH, Feder RS, Belin MW . Keratoconus and related non-inflammatory corneal thinning disorders. Surv Ophthalmol 1984; 28 (4): 293–322.
Jimenez JLO, Jurado JCG, Rodriguez FJB, Laborda DS . Keratoconus: age of onset and natural history. Optom Vis Sci 1997; 74 (3): 147–151.
Moodaley LC, Woodward EG, Liu CS, Buckley RJ . Life expectancy in keratoconus. Br J Ophthalmol 1992; 76 (10): 590–591.
Smiddy WE, Hamburg TR, Kracher GP, Stark WJ . Keratoconus: contact lens or keratoplasty? Ophthalmology 1988; 95: 487–492.
Kennedy RH, Bourne WM, Dyer JA . A 48 year clinical and epidemiological study of keratoconus. Am J Ophthalmol 1986; 101 (3): 267–273.
Weed KH, McGhee CNJ . Referral patterns, treatment management and visual outcome in keratoconus. Eye 1998; 12: 663–668.
Lim N, Vogt U . Characteristics and functional outcomes of 130 patients with keratoconus attending a specialist contact lens clinic. Eye 2002; 16: 54–59.
Doyle SJ, Bullock J, Gray C, Spencer A, Cunningham C . Emmetropisation, axial length and corneal topography in teenagers with Down's syndrome. Br J Ophthalmol 1998; 82 (7): 793–796.
Macsai M, Maguen E, Nucci P . Keratoconus and Turner's syndrome. Cornea 1997; 16 (5): 534–536.
Pearson AR, Soneji B, Sarvananthan N, Sandford-Smith JH . Does ethnic influence the incidence or severity of keratoconus? Eye 2000; 14 (4): 625–628.
Lee LR, Readshaw G, Hirst LW . Keratoconus: the clinical experience of a Brisbane Ophthalmologist. Ophthalmic Epidemiol 1996; 3 (3): 119–125.
Rabinowitz YS . Keratoconus. Surv Ophthalmology 1998; 42 (4): 297–319.
Zadnik K, Steger-May K, Fink BA, Joslin CE, Nichols JJ, Rosenshel CE et al. Between eye asymmetry in keratoconus. Cornea 2002; 21 (7): 671–679.
Burger DS . Keratoconus: etiology, diagnosis and management. Practical Optometry 1991; 2 (4): 121–129.
Burns DM, Johnston FM, Frazer DG, Patterson C, Jackson AJ . Keratoconus: an analysis of corneal asymmetry. Br J Ophthalmol 2004; 88 (10): 1252–1255.
Owens H, Walters GA . An evaluation of the keratoconic cornea using computerised corneal mapping and ultrasonic measurements of corneal thickness. Ophthalmic Physiol Opt 1996; 16 (2): 115–123.
Barr JT, Schectman KB, Fink BA, Pierce GE, Pensyl CD, Zadnik K et al. Corneal scarring in the Collaborative longitudinal evaluation of keratoconus (CLEK) study: baseline prevalence and repeatability of detection. Cornea 1999; 18 (1): 34–46.
Van der Worp E, De Brabander J, Swarbrick H, Nuijts R, Hendrikse F . Corneal dessication in rigid contact lens wear: 3 and 9 o'clock staining. Optom Vis Sci 2003; 80 (4): 280–290.
Schwallie JD, McKenney CD, Long WD, McNeil A . Corneal staining in normal contact lens wearers. Optom Vis Sci 1997; 74 (2): 92–98.
Nichols KK, Mitchell GL, Simon KM, Chivers DA, Edrington TB . Corneal staining in hydrogel lens wearers. Optom Vis Sci 2002; 79 (1): 20–30.
Yaylali V, Kaufman SC, Thompson HW . Corneal thickness measurements with the Orbscan topography system and ultrasonic pachymetry. J Cataract Refract Surg 1997; 23: 1345–1350.
Chakrabarti HS, Craig JP, Brahma A, Malik TY, McGhee CNJ . Comparison of corneal thickness measurements using ultrasound and Orbscan slit-scanning topography in normal and post-LASIK eyes. J Cataract Refract Surg 2001; 27 (11): 1823–1828.
Lattimore MR, Kaupp S, Schallhorn S, Lewis R . Orbscan pachymetry. Implications of a repeated measures and diurnal variation analysis. Ophthalmology 1999; 106: 977–981.
Marsich MM, Bullimore MA . The repeatability of corneal thickness measures. Cornea 2000; 19 (6): 792–795.
Doughty MJ, Zamman ML . Human corneal thickness and its impact on inra-ocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol 2000; 44 (5): 367–408.
Watters GA, Owens H . Evaluation of mild, moderate and advanced keratoconus using ultrasound pachometry and the EyeSys Videokeratoscope. Optom Vis Sci 1998; 75 (9): 640–646.
Auffarth GU, Wang L, Volcker HE . Keratoconus evaluation using the Orbscan topography system. J Cataract Refract Surg 2000; 26: 222–228.
Colin J, Sale Y, Malet F, Cochener B . Inferior steepening is associated with thinning of the inferotemporal cornea. J Refract Surg 1996; 12: 697–699.
Macsai MS, Varley GA, Krachmer JH . Development of keratoconus after contact lens wear. Arch Ophthalmol 1990; 108: 534–538.
Bowden TJ, Harknett A, Forrest I . Contact lens wearer profile. Contact Lens Anterior Eye 2005; 28 (1): 37–45.
Lindsay RG, Bruce AS, Gutteridge IF . Keratoconus associated with continual eye rubbing due to punctal agenesis. Cornea 2000; 19 (4): 567–569.
McCormack HM, De L, Horne DJ, Sheather S . Clinical applications of visual analogue scales: a critical review. Psychol Med 1988; 18: 1007–1019.
McMonnies CW, Boneham GC . Keratoconus, itch, eye rubbing and hand dominance. Clin Exp Optomol 2003; 9–86 (6): 376–384.
Bawazeer AM, Hodge WL, Lorimer B . Atopy and keratoconus: a multivariate analysis. Br J Ophthalmol 2000; 84: 834–836.
Gasset AR, Hinson WA, Frias JL . Ann ophthalmol keratoconus and atopic diseases Ann Opthalmo 1978; 10 (8): 991–994.
Harrison RJ, Klouda PT, Easty DL, Manku M, Charles J, Stewart CM . Association between keratoconus and atopy. Br J Ophthalmol 1989; 73 (10): 16–22.
McGill JI, Holgate ST, Church MK . Allergic eye disease mechanisms. Br J Ophthalmol 1998; 82: 1203–1214.
Acknowledgements
Baseline data were presented at College of Ophthalmology Annual Meeting 2004. Dr KH Weed was supported by an MRC Clinical Research Fellowship.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
DUSKS Questionnaire

Rights and permissions
About this article
Cite this article
Weed, K., MacEwen, C., Giles, T. et al. The Dundee University Scottish Keratoconus study: demographics, corneal signs, associated diseases, and eye rubbing. Eye 22, 534–541 (2008). https://doi.org/10.1038/sj.eye.6702692
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702692
Keywords
This article is cited by
-
Incidence and prevalence of keratoconus in Taiwan during 2000–2018 and their association with the use of corneal topography and tomography
Eye (2024)
-
Natural history and predictors for progression in pediatric keratoconus
Scientific Reports (2023)
-
Clinical performance of a custom-designed soft contact lens in patients with keratoconus and intolerance to rigid contact lenses
Japanese Journal of Ophthalmology (2022)
-
Risk factors and severity of keratoconus on the East Coast of China
International Ophthalmology (2022)