Abstract
Objectives:
(1) To develop a fully automated algorithm for segmentation of visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT), excluding intermuscular adipose tissue (IMAT) and bone marrow (BM), from axial abdominal magnetic resonance imaging (MRI) data. (2) To evaluate the algorithm accuracy and total method reproducibility using a semi-automatically segmented reference and data from repeated measurements.
Background:
MRI is a widely used in adipose tissue (AT) assessment. Manual analysis of MRI data is time consuming and biased by the operator. Automated analysis spares resources and increase reproducibility. Fully automated algorithms have been presented. However, reproducibility analysis has not been performed nor has methods for exclusion of IMAT and BM been presented.
Methods:
In total, 49 data sets from 31 subjects were acquired using a clinical 1.5 T MRI scanner. Thirteen data sets were used in the derivation of the automated algorithm and 36 were used in the validation. Common image analysis tools such as thresholding, morphological operations and geometrical models were used to segment VAT and SAT. Accuracy was assessed using a semi-automatically created reference. Reproducibility was assessed from repeated measurements.
Results:
Resulting AT volumes from the automated analysis and the reference were not found to differ significantly (2.0±14% and 0.84±2.7%, given as mean±s.d., for VAT and SAT, respectively). The automated analysis of the repeated measurements data significantly increased the reproducibility of the VAT measurements. One athletic subject with very small amounts of AT was considered to be an outlier.
Conclusions:
An automated method for segmentation of VAT and SAT and exclusion of IMAT and BM from abdominal MRI data has been reported. The accuracy and reproducibility of the method has also been demonstrated using a semi-automatically segmented reference and analysis of repeated acquisitions. The accuracy of the method is limited in lean subjects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout









Similar content being viewed by others
References
Obesity. Preventing and Managing the Global Epidemic. World Health Organization (WHO): Geneva, 2000.
Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG et al. Obesity and the risk of heart failure. N Engl J Med 2002; 347: 305–313.
Kopelman PG . Obesity as a medical problem. Nature 2000; 404: 635–643.
Wajchenberg BL . Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev 2000; 21: 697–738.
Ross R . Advances in the application of imaging methods in applied and clinical physiology. Acta Diabetol 2003; 40 (Suppl 1): S45–S50.
Thomas EL, Saeed N, Hajnal JV, Brynes A, Goldstone AP, Frost G et al. Magnetic resonance imaging of total body fat. J Appl Physiol 1998; 85: 1778–1785.
Positano V, Gastaldelli A, Sironi AM, Santarelli MF, Lombardi M, Landini L . An accurate and robust method for unsupervised assessment of abdominal fat by MRI. J Magn Reson Imaging 2004; 20: 684–689.
Liou TH, Chan WP, Pan LC, Lin PW, Chou P, Chen CH . Fully automated large-scale assessment of visceral and subcutaneous abdominal adipose tissue by magnetic resonance imaging. Int J Obes (London) 2006; 30: 844–852.
Elbers JM, Haumann G, Asscheman H, Seidell JC, Gooren LJ . Reproducibility of fat area measurements in young, non-obese subjects by computerized analysis of magnetic resonance images. Int J Obes Relat Metab Disord 1997; 21: 1121–1129.
Gastaldelli A, Miyazaki Y, Pettiti M, Buzzigoli E, Mahankali S, Ferrannini E et al. Separate contribution of diabetes, total fat mass, and fat topography to glucose production, gluconeogenesis, and glycogenolysis. J Clin Endocrinol Metab 2004; 89: 3914–3921.
Machann J, Thamer C, Schnoedt B, Haap M, Haring HU, Claussen CD et al. Standardized assessment of whole body adipose tissue topography by MRI. J Magn Reson Imaging 2005; 21: 455–462.
Staten MA, Totty WG, Kohrt WM . Measurement of fat distribution by magnetic resonance imaging. Invest Radiol 1989; 24: 345–349.
Gerard EL, Snow RC, Kennedy DN, Frisch RE, Guimaraes AR, Barbieri RL et al. Overall body fat and regional fat distribution in young women: quantification with MR imaging. AJR Am J Roentgenol 1991; 157: 99–104.
Ross R, Leger L, Morris D, de Guise J, Guardo R . Quantification of adipose tissue by MRI: relationship with anthropometric variables. J Appl Physiol 1992; 72: 787–795.
Shen W, Wang Z, Punyanita M, Lei J, Sinav A, Kral JG et al. Adipose tissue quantification by imaging methods: a proposed classification. Obes Res 2003; 11: 5–16.
Gonzalez CR, Woods RE . Digital Image Processing 2nd edn. Prentice Hall, Upper Saddle River, New Jersey, 2002.
Ross R, Shaw KD, Martel Y, de Guise J, Avruch L . Adipose tissue distribution measured by magnetic resonance imaging in obese women. Am J Clin Nutr 1993; 57: 470–475.
Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J et al. Visceral adipose tissue: relations between single-slice areas and total volume. Am J Clin Nutr 2004; 80: 271–278.
Kuk JL, Church TS, Blair SN, Ross R . Does measurement site for visceral and abdominal subcutaneous adipose tissue alter associations with the metabolic syndrome? Diabetes Care 2006; 29: 679–684.
Shen W, Punyanitya M, Chen J, Gallagher D, Albu J, Pi-Sunyer X et al. Visceral adipose tissue: relationships between single slice areas at different locations and obesity-related health risks. Int J Obes (London) 2007; 31: 763–769.
Brennan DD, Whelan PF, Robinson K, Ghita O, O'Brien JM, Sadleir R et al. Rapid automated measurement of body fat distribution from whole-body MRI. AJR Am J Roentgenol 2005; 185: 418–423.
Kullberg J, Angelhed JE, Lönn L, Brandberg J, Ahlström H, Frimmel H et al. Whole-body T1 mapping improves the definition of adipose tissue: consequences for automated image analysis. J Magn Reson Imaging 2006; 24: 394–401.
Belaroussi B, Milles J, Carme S, Zhu YM, Benoit-Cattin H . Intensity non-uniformity correction in MRI: existing methods and their validation. Med Image Anal 2006; 10: 234–246.
Yang GZ, Myerson S, Chabat F, Pennell DJ, Firmin DN . Automatic MRI adipose tissue mapping using overlapping mosaics. MAGMA 2002; 14: 39–44.
Cootes TF, Taylor CJ, Cooper DH, Graham J . Active Shape Models-Their Training and Application. Comput Vis Imag Underst 1995; 61: 38–59.
Nelder JA, Mead R . A simplex method for function minimization. Comput J 1965; 7: 308–313.
Otsu N . A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern 1979; 9: 62–66.
Udupa JK, Leblanc VR, Zhuge Y, Imielinska C, Schmidt H, Currie LM et al. A framework for evaluating image segmentation algorithms. Comput Med Imaging Graph 2006; 30: 75–87.
Acknowledgements
This study was supported by the Swedish Research Council, Grant no. K2006-71X-06676-24-3.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
Definition of analysis tools
Connected area mapping. The CAM tool processes a binary input volume, treated as a set of 2D-images. First, a slice-wise labelling is performed, using an eight-neighbourhood (3 × 3) structuring element, to separate different objects. Secondly, all object pixels are given the value of the size of the connected area to which they belong.
Connected volume mapping. This tool is based on the same principle as the CAM tool but the volumes of the connected components are analysed in 3D using an 18-neighbourhood structuring element.
Orthogonal convex hull. This tool is an adapted version of a slice-wise operating convex hull.16 A convex hull by definition enables all pixels in an object to connect to any other pixel in the object using a straight line fully enclosed by the object. In the orthogonal convex hull, object pixels are only connected in the x and y directions.
Pelvis model. A model of the pelvis geometry was created as the mean shape of manually measured pelvis shapes of the subjects in the derivation cohort. The centre pixel of the spinal cord, Pi, where i=1…16 defines the slice, was visually determined in slices 1–8. Position P8 was used as the reference position in each volume. The positions P9–P16 were set equal to P8. Occasionally, the spinal cord was not present in slices 1–3. When not, the points affected (P1–P3) were set equal to the point of the closest superior slice, with spinal cord present. The change of Pi across image slices 1–8, in anterior–posterior direction, was modelled using constant increments.
Two straight lines were manually fitted from each Pi along the shape of the pelvis, see Figure 10. The lines were drawn both to the left and to the right, forming a v-shape, in all images where the pelvis was present. The lines were drawn anterior to the subject's iliac crests separating pelvis from the VAT area. The angles of all lines were measured. The angle change between image slices, where pelvis was present, was modelled using linear interpolation between slices 1 and 12. For slices 13–16, the same angle as for slice 12 was used. Manual measurements of positions and angles were performed using the software ImageJ (Image Processing and Analysis in Java, v1.36b, 13 March 2006, http://rsb.info.nih.gov/ij/).
Vertebra model. A model of the vertebral region was created by manual delineation of this region in all subjects in the derivation cohort. The purpose was to include geometrical a priori information on a region known to contain inter-/intramuscular AT and BM. The region included sacrum, the vertebras, and the spinal muscles. Psoas muscles were not included since the surrounding AT was classified as VAT. The common region delineated in all subjects, merged using point P8 in each subject as reference, was used in the model.
Dilation and erosion. Dilation and erosion is performed in 3D, using an 18-neighbourhood, and in 2D using an eight-neighbourhood structuring element, respectively.
Region growing. All region growings are performed using pixel intensity criteria. In 2D, an eight-neighbourhood is used and in 3D an 18-neighbourhood is used.
Image masking. Image masks are binary images having a foreground represented by white pixels (=1) and a background represented by black (=0) pixels. When the masking is performed, only pixels located in the foreground are considered in further processing.
Appendix B1
Detailed description of step 1
(1A) The input volume image, I, is first thresholded at level T1A=100, empirically determined from the derivation cohort, to separate body and the arms from background noise. The resulting binary image B1A is processed using the CVM tool to derive the volume-mapped image I1CVM. The arms are excluded from I1CVM by removing everything but the largest connected component, creating the binary image B1A2. Note that the arms need to be separated from the abdominal area in each slice of B1A. This was assured during the image acquisition by careful subject positioning. Image I1A is created by masking of the input volume I using B1A2.
(1B) I1A may contain holes from low intensity areas inside the body. A 3D region growing of the background ensures that a single connected component makes up the background. The inverse of the region growing result is denoted B1B and makes up the body, including the low intensity areas in I1A, and gives a crude estimate of the abdominal volume.
(1C) The input volume image I is cropped using the bounding volume of the body in B1B to minimize the data handling in upcoming processing steps. The cropped volume image I is denoted I1C. Note that since the cropping is performed in 3D, all slices are not optimally cropped.
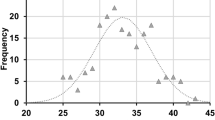
(1D) Histogram H1D is derived from I1C masked by B1B. H1D is analysed to determine if the abdominal histogram has a bimodal shape, characteristic for data sets containing medium to large amounts of AT. Data sets containing small amounts of AT may not show an AT histogram peak, hence have non-bimodal histograms. The bimodal shape is determined by analysing the histogram peaks and nadirs. If two peaks are found, both with amplitudes (A1 and A2) greater than Amin, separated by a minimum intensity range Rmin, having a nadir, positioned between the peaks of an amplitude smaller than K% of the smallest peak amplitude, the histogram shape is considered bimodal. The Amin parameter was used to ensure that peaks were not found in the histogram noise and Rmin was used to prevent subpeaks, sometimes present on main histogram peaks, from being interpreted as a bimodal shape. K was used to control the minimum histogram depth. The parameters determined using manual measurements from the histograms from of all subjects in the derivation cohort were; Amin=200 pixels, Rmin=250 au, and K=80%.
Appendix B2
Detailed description of step 2
(2A) A threshold, T2, is computed to determine pixels in I1C that contain AT. The threshold is determined using the histogram H1D by least square fitting of a Gaussian function, G2, to the AT peak. T2 is determined as the threshold including 95% of the AT represented by the area under G2. B2A is derived by thresholding I1C at level T2.
(2B) Image I1C is masked using B2A creating image I2B, which only contains grey level values from pixels determined to contain AT. Intensity correction is performed by slice-wise modelling of the inhomogeneity. I2B can be thought of as a topological map where intensity represents height. A fitting of a second-degree surface, intensity=ax2+by2+cxy+dx+ey+f, where a–f are coefficients calculated in this step, to the topological map smoothly models the intensity inhomogeneities over the body area in each slice. The fitting of the second-degree surface is performed using the summed least square criteria and the downhill simplex method of Nelder and Mead.26 The results from the fitting of one surface is illustrated in Figure 3.
(2C) The deviations of the smooth intensity inhomogeneity model from the mean AT pixel intensity are used to correct all body pixels in image I1C creating the corrected image I2C.
Appendix B3
Detailed description of step 3
(3A) A border region is determined by creation of a border mask denoted B3A. The mask is defined as the result from a XOR (exclusive or) operation applied on two image masks. The first image mask is a dilated (in 3D) version of the body mask B1B and the second is an eroded (in 3D) version of the body mask.
(3B) A histogram H3 is created from the pixel intensities of I2C masked by B3A. A method based on minimization of weighted within class variances, proposed by Otsu,27 is used to determine the body threshold T3 from H3.
(3C) A 3D region growing, of the background of I2C until reaching T3, gives B3C and ensures that a single connected component makes up the background. The remainder, also a single connected component, makes up the volume of the body. Image I2C masked using B3C is denoted I3C and contains the objectively segmented body after compensation for intensity inhomogeneities.
Appendix B4
Detailed description of step 4
When H1D is determined to be bimodal, in step 1, H4 is derived from the whole abdominal volume and when H1D is determined to be non-bimodal, H4 is derived from a subvolume situated in the SAT region. The subvolume is used to increase the relative amount of pixels containing AT in H4.
When H1D is bimodal, a fitting of a Gaussian function, G4, to the histogram AT-peak is used. The automatic determination of T4 from the fitted G4 is tuned to maximize the similarity to manually determined thresholds. The threshold used as reference for each subject in the derivation cohort was the mean threshold from two-trained operator's independent threshold selections. The mean deviation from the manually determined thresholds was minimized when T4 was selected to include 96% of the area under G4 into the AT class.
When H1D is non-bimodal, a binary mask, B4, is created by applying four iterations of erosion on a copy of B3C. B4 is used to only include the outer body pixels in the creation of the H4. T4 is then determined using an algorithm proposed by Otsu.27
Appendix B5
Detailed description of step 5
(5A) The gradient image, denoted I5-GRAD, is computed from I3C using a finite difference gradient magnitude filter. The computations are performed slice-wise. The gradient response from the skin interface is removed from I5-GRAD by means of a mask created from a slice-wise eroded copy of B3C.
(5B) A coarse mask B5-COARSE is created from I5-GRAD by a thresholding at gradient magnitude level T5=40, empirically determined from the derivation cohort, followed by the use of the CAM tool and the orthogonal convex hull tool to remove small objects and to create a closed object.
(5C) Masking B4-REST using B5-COARSE removes most of the erroneously segmented non-fat pixels from B4-REST creating B5C. B5C is processed using slice-wise morphological opening in the posterior parts of the body to remove objects derived from blood vessels present in the SAT. B5 is created from B5C by application of the orthogonal convex hull tool. The B5 mask is used to mask B4-AT creating B5-VAT and B5-SAT.
Appendix B6
Detailed description of step 6
(6A) The position of the spinal cord is determined at the L4-L5 level (slice 8). This is performed using a template search. The template was created from a smoothed subvolume cropped from a single randomly selected subject from the derivation cohort. The template volume was created as the smallest rectangular volume, with sides parallel to the image x and y directions, including the L4 and L5 vertebras and the spinal cord. A minimization of a least square difference cost function and translation of the template volume were used.
(6B) AT-pixels anterior to the pelvis model v-shape were considered to originate from VAT. AT-pixels posterior to the v-shape were considered to originate from BM or intermuscular AT. The raised AT threshold posterior to the pelvis model reduces the amount of AT pixels from these depots in B5-VAT creating B6-VAT. The raising of the threshold was empirically determined, using the derivation cohort, to 0.25 s.d. of the Gaussian function G4.
Appendix B7
Detailed description of step 7
(7A) The vertebra model is used to include geometrical a priori knowledge for removal of binary objects originating from BM and inter-/intramuscular AT from B6-VAT. The position of the spinal cord, determined in step 6A, is used to position the vertebra model and to remove binary objects, inside or posterior to the vertebra model, from B6-VAT, creating B7A.
(7B) A region growing is performed to extend the VAT depot. This is performed to optimize the similarity, using the precision index proposed by Udupa et al.28 to manually segmented VAT from six subjects in the derivation cohort. Pixels with grey values larger than 90% of the AT threshold T4 in a 3D-neighbourhood of VAT-pixels in B7A are added to B7A, creating B7B.
(7C) The CAM tool is used to remove small binary objects originating from SAT, BM, or inter-/intramuscular AT, from B7B, creating B7C.
(7D) The B5 mask is first eroded slice-wise creating B5-ERODED. The anterior parts of B5-ERODED are determined using a model based on slice-wise manual measurements of the subjects in the derivation cohort. The measurements determined the anterior proportion of the B5-ERODED mask that could be used without including pelvis and vertebras in the mask. Linear interpolation of the proportions was used from slice 1 to 5. Slices 5–16 used a proportion of 0.5. The binary volume created is denoted B7D.
The union of B7C and B7D is processed by the orthogonal convex hull tool, only operating in the y direction, and by one iteration of morphological closing, resulting in the B7 mask. The VAT pixels are determined as the AT pixels masked from B7B using the B7 mask.
Rights and permissions
About this article
Cite this article
Kullberg, J., Ahlström, H., Johansson, L. et al. Automated and reproducible segmentation of visceral and subcutaneous adipose tissue from abdominal MRI. Int J Obes 31, 1806–1817 (2007). https://doi.org/10.1038/sj.ijo.0803671
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803671
Keywords
This article is cited by
-
Abdominal fat quantification using convolutional networks
European Radiology (2023)
-
CAFT: a deep learning-based comprehensive abdominal fat analysis tool for large cohort studies
Magnetic Resonance Materials in Physics, Biology and Medicine (2022)
-
Artificial intelligence-aided CT segmentation for body composition analysis: a validation study
European Radiology Experimental (2021)
-
Assisted quantification of abdominal adipose tissue based on magnetic resonance images
Multimedia Tools and Applications (2020)
-
Automated analysis of liver fat, muscle and adipose tissue distribution from CT suitable for large-scale studies
Scientific Reports (2017)