Abstract
There is compelling evidence for the involvement of hypothalamic-pituitary-adrenal (HPA) axis abnormalities in depression. Growing evidence has suggested that the combined dexamethasone (DEX)/corticotropin-releasing hormone (CRH) test is highly sensitive to detect HPA axis abnormalities. We organized a multicenter study to assess the DEX/CRH test as a state-dependent marker for major depressive episode in the Japanese population. We conducted the DEX/CRH test in 61 inpatients with major depressive episode (Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM-IV)) and 57 healthy subjects. In all, 35 patients were repeatedly assessed with the DEX/CRH test on admission and before discharge. The possible relationships between clinical variables and the DEX/CRH test were also examined. Significantly enhanced pituitary–adrenocortical responses to the DEX/CRH test were observed in patients on admission compared with controls. Such abnormalities in patients were significantly reduced after treatment, particularly in those who underwent electroconvulsive therapy (ECT) in addition to pharmacotherapy. Age and female gender were associated with enhanced hormonal responses to the DEX/CRH test. Severity of depression correlated with DEX/CRH test results, although this was explained, at least in part, by a positive correlation between age and severity in our patients. Medication per se was unrelated to DEX/CRH test results. These results suggest that the DEX/CRH test is a sensitive state-dependent marker to monitor HPA axis abnormalities in major depressive episode during treatment. Restoration from HPA axis abnormalities occurred with clinical responses to treatment, particularly in depressed patients who underwent ECT.
Similar content being viewed by others
INTRODUCTION
There is compelling evidence for an important role of hypothalamic-pituitary-adrenal (HPA) axis abnormalities in the pathophysiology of mood disorders (Holsboer, 1995; Plotsky et al, 1998). To quantify the dysregulation of HPA axis, the dexamethasone (DEX) suppression test (DST) has been studied most extensively since Carroll et al (1981) standardized it as a biological marker for the diagnosis of melancholia. A major drawback of the DST, however, is its modest sensitivity (rate of nonsuppression of cortisol) of 40–50% (Carroll, 1982; American Psychiatric Association, 1987). Subsequently, a refined laboratory test that combines the DST and corticotropin-releasing hormone (CRH) challenge, the DEX/CRH test, has been introduced (Holsboer et al, 1987; von Bardeleben and Holsboer, 1989). In normal subjects, pretreatment with DEX suppresses pituitary–adrenal responses to CRH. In depressed patients, however, the same procedure enhances hormonal responses to CRH, resulting in higher sensitivity of the DEX/CRH test to major depression by up to 80% (Heuser et al, 1994b). Furthermore, the DEX/CRH test was shown to be more closely associated with the activity of HPA system (24-h cortisol profiles) than the standard DST in healthy and depressed subjects (Deuschle et al, 1998). We have confirmed the relatively high sensitivity of the DEX/CRH test in Japanese patients with depressive disorder (Oshima et al, 2000; Kunugi et al, 2004). These findings indicate that the DEX/CRH test is a useful laboratory tool to monitor HPA axis abnormalities in depressed patients in clinical practice. However, previous studies have not always provided consistent results as to whether clinical variables, such as age, severity, and diagnosis (unipolar vs bipolar), are associated with DEX/CRH test results.
In serial DST studies, conversion from nonsuppressor to suppressor status is temporally associated with clinical responses to antidepressants (eg Holsboer et al, 1982; Greden et al, 1983). In line with this, hormonal responses to the DEX/CRH test also restored after successful treatment with antidepressants (Holsboer-Trachsler et al, 1991; Heuser et al, 1996; Baghai et al, 2002; Hatzinger et al, 2002), suggesting that the DEX/CRH test is a useful state-dependent marker. However, it has been argued that DEX/CRH test results may be trait dependent, particularly in bipolar patients (Holsboer et al, 1995; Schmider et al, 1995; Watson et al, 2004; Ising et al, 2005).
Changes in repeated DEX/CRH tests may depend on treatment modality. In responders to repetitive transcranial magnetic stimulation therapy, post-DEX cortisol levels prior to CRH challenge decreased, while no change of CRH-induced ACTH and cortisol release was observed (Zwanzger et al, 2003). Similarly, partial changes in DEX/CRH tests were observed in responders to partial sleep deprivation therapy (Schule et al, 2002). Concerning electroconvulsive therapy (ECT), there is little information on changes in the DEX/CRH test. Previous studies employing conventional DST have provided inconsistent results: some authors reported a positive correlation between response to ECT and normalization of the HPA axis (Albala et al, 1981; Papakostas et al, 1981; Grunhaus et al, 1987; Devanand et al, 1991); an author reported an equivocal result (Devanand et al, 1987); and others failed to find such a relationship (Coryell, 1986; Fink et al, 1987). These inconsistent results require further investigations.
The present study aimed to assess the DEX/CRH test as a state-dependent marker to monitor HPA axis abnormalities in patients with major depressive episode, including patients receiving ECT. Furthermore, we examined DEX/CRH test results for a possible association with clinical variables, such as age, gender, severity, and medication.
METHODS
Subjects
Subjects were 57 healthy controls (37 men and 20 women; mean age: 31 years, range: 22–48, standard deviation (SD): 7) and 61 inpatients (24 men and 37 women; mean age: 54 years, range 30–82, SD: 13) with major depressive episode according to the Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM-IV) (American Psychiatric Association, 1994), who were recruited from eight institutions in Japan. All the patients and controls were biologically unrelated Japanese. In all, 54 patients were diagnosed with unipolar major depression (29 with single episode and 25 with recurrent episodes), and the remaining seven with bipolar I disorder. The following were excluded: patients who had somatic disorders, such as inflammation, endocrine disorders, and neoplasm; patients who were treated with liver-enzyme-inducing drugs, lithium carbonate, or carbamazepine; and patients who were withdrawn from abused illicit drugs and other substances, such as benzodiazepines and alcohol. After full description of the study, written informed consent was obtained from every subject for his/her participation in the study. The study protocol was approved by the ethics committee of each institution.
Among the 61 patients, 35 (13 men and 22 women; 13 unipolar depression with single episode, 18 unipolar depression with recurrent episodes, and four bipolar disorder; mean age: 55 years, SD: 15) were repeatedly assessed with the DEX/CRH test on admission and before discharge, while the remaining 26 were assessed only once on admission. Among the 35 patients, 12 underwent ECT in addition to pharmacotherapy. Based on the effect size reported by Holsboer-Trachsler et al (1991), this sample size (N=35) had a power of 96% at the 0.05 level of significance (two-tailed) to detect effects of treatment on DEX/CRH test results.
The severity of index depressive episode was assessed with the 21-item version of the Hamilton depression rating scale (HDRS; Hamilton, 1967) when the DEX/CRH test was conducted. Patients who were scored less than 15 by the HDRS on admission were not enrolled in the study. The majority of the patients were medicated with antidepressants, while seven patients were drug naive on admission. We did not control for class of antidepressant medication, and data were obtained in the ordinary clinical setting in Japan. Thus, a variety of antidepressants were medicated; however, switch in medication was avoided for at least 4 days before conducting the DEX/CRH test. ECT was administered six to 10 times (two or three times a week) for each patient with electrical stimuli of 100–110 V for 5–10 s, discharged with bilateral electrodes placed bifrontotemporally. Patients were anesthetized with propofol, and motor convulsion was suppressed with succinylcholine.
DEX/CRH Test
The DEX/CRH test was conducted as described by Zobel et al (2001). Subjects were pretreated with an oral dose of 1.5 mg of DEX (Asahikasei Pharmaceutical Corporation, Tokyo, Japan) at 2300 hours. On the next day, a vein was cannulated at 1430 hours to collect blood at 1500, 1530, 1545, 1600, and 1615 hours via an intravenous catheter. Human CRH (100 μg) (hCRH ‘Mitsubishi’, Mitsubishi Pharma Corporation, Tokyo, Japan) was administered intravenously at 1500 hours immediately after the first blood collection (protocol 1). In part of patients (N=8), a vein was cannulated at 1330 hours to collect blood at 1400, 1415, 1430, 1500, and 1600 hours (protocol 2). hCRH was administered intravenously immediately after the first blood collection at 1400 hours. Subjects rested supine throughout the test in a calm room. Between the collections of blood specimen, the catheter was kept patent by physiological saline infusion at a rate of 50 ml/h. Blood samples were immediately centrifuged and stored at −20°C. Plasma concentrations of ACTH and cortisol were measured by radioimmunoassay at SRL Corporation (Tokyo, Japan). The detection limits for ACTH and cortisol were 5.0 pg/ml and 1.0 μg/dl, respectively.
Data Presentation for Hormonal Measures
We defined A0 as the plasma concentration of ACTH in the blood sample obtained at 1500 hours for protocol 1 or 1400 hours for protocol 2, that is, plasma concentrations that were measured at 16 or 15 h after the oral intake of DEX but immediately before the infusion of CRH. A30 and A60 were defined as the plasma concentrations of ACTH, which were measured at 30 and 60 min after the intravenous infusion of CRH, respectively. Adif denotes the difference between the A0 and A60 values. The C0, C30, C60, and Cdif values were defined similarly for the plasma concentrations of cortisol. These values were available in both protocols 1 and 2, which enabled us to combine data from these protocols and to analyze all the subjects simultaneously. There was no evidence for significant effects on hormonal outcomes due to a 1 h difference between the two protocols (data not shown), combining the data from the two protocols. According to our previous reports (Oshima et al, 2000; Kunugi et al, 2004), the plasma concentrations of ACTH and cortisol peak at approximately 60 min after infusion of CRH, indicating that the A60 and C60 values reflect the maximal responses to CRH. The area under the time curve (AUC, arbitrary unit) was calculated according to the trapezoidal rule (Aauc for ACTH and Cauc for cortisol). Aauc was calculated from the A0, A30, and A60 values, and Cauc from the C0, C30, and C60 values.
As the plasma cortisol criterion concentration of 5 μg/dl was suggested to be most effective for assessing an abnormal DST result (Carroll, 1982), ‘nonsuppressor’ was defined to be an individual who showed a C0 value of ⩾5 μg/dl irrespective of the C60 value. Furthermore, ‘intermediate suppressor’ was defined a priori to be an individual who showed a C0 value of <5 μg/dl and a C60 of ⩾5 μg/dl. The remaining individuals, who showed both C0 and C60 values of <5 μg/dl, were defined as ‘suppressors’. These definitions were almost identical to those described by Kunugi et al (2004).
Statistical Analysis
All statistical analyses were made with SPSS for Windows (version 11, SPSS Japan, Tokyo). Intergroup comparisons were made for age and HDRS scores according to t-test or one-way ANOVA. The proportion of categorical data, such as gender, was compared according to the χ2 test for independence. Intergroup comparisons were made for ACTH and cortisol according to the Mann–Whitney U-test (comparisons between two groups) or the Kruskal–Wallis H-test (comparisons among three groups). Differences between hormonal responses observed on admission and before discharge were tested according to the Wilcoxon paired signed-ranks test. Nonparametric tests were employed because the endocrine values did not always show a normal distribution and part of subjects showed the A0 and/or C0 values below detection limits. All p-values reported are two-tailed. A value of p<0.05 was considered statistically significant.
RESULTS
Hormonal Responses in Patients and Controls
Effects of age and gender
Hormonal responses in patients (on admission) and controls are shown in Table 1. To see the effects of age on hormonal responses, the patient group was dichotomized into the ‘young’ (⩽50 years) and ‘aged’ (>50 years) patient groups. All controls, whose age ranged between 22 and 48 years, were considered to be ‘young’ subjects. To see the effects of gender, hormonal values were presented separately by gender. In the patient group, all the mean hormonal values (A0, A60, Adif, Aauc, C0, C60, Cdif, and Cauc) were higher in the aged patient group than in the young patient group, although a statistically significant difference was found only for A0 (p=0.048, Mann–Whitney U-test) and a nonsignificant trend for Cauc (p=0.055).
When males and females were compared, hormonal responses to pretreatment with DEX (A0 and C0) did not seem to be consistently different in young patients, aged patients, or controls (see Table 1). However, hormonal responses to CRH as manifested by Adif and Cdif were consistently higher in females than in males for all the three groups (young patients, aged patients, and controls). Among young patients, Cdif was significantly higher in females than in males (p=0.029, Mann–Whitney U-test), although differences in Adif did not reach statistical significance (p=0.17). Similarly, in aged patients, the mean Cdif value was significantly higher in females than in males (p=0.034). However, differences in mean Adif failed to reach statistical significance (p=0.14). Among subjects in the control group, females showed statistically higher Adif values than males, and there was a trend towards an increased Cdif value in females than in males.
Patients vs controls
Since the above data indicated that age and gender have effects on the DEX/CRH test, young patients (14 men and eight women) only were compared with controls (37 men and 20 women). These two groups were nearly matched for the ratio of males to females (p=0.91, χ2 test), although there was still a significant difference in mean age (41 years SD 7 vs 31 years SD 7; p<0.001 by t-test). Although the values for ACTH (A0, A60, Adif, and Aauc) were consistently higher in young patients than in controls (see Table 1), none of the differences reached statistical significance (p=0.41 for A0, p=0.27 for A60, p=0.13 for Adif, p=0.74 for Aauc, Mann–Whitney U-test). However, the values for cortisol were significantly higher in young patients than in controls (p=0.004 for C0, p=0.033 for C60, p=0.036 for Cauc), except for Cdif (p=0.14).
One might suspect, however, that the significant differences observed in cortisol measures were attributable simply to the differential age distributions between young patients and controls. To resolve this issue, post hoc analyses were performed, selecting 18 patients and 18 controls matched for both age and gender (12 males and six females; mean age 38 years (SD 6) for patients and controls). Results in these subjects were essentially unchanged; cortisol measures were significantly higher in patients than in controls (p=0.009 for C0, p=0.044 for C60, p=0.040 for Cauc), except for Cdif (p=0.21). This ensures that enhanced cortisol responses to the DEX/CRH test in patients were not attributable simply to differential age distribution between patients and controls.
Clinical variables and DEX/CRH test results
Possible relationships between clinical variables and DEX/CRH test results were examined in the patient group. There was a significant or a nonsignificant trend towards a positive correlation between HDRS scores on admission and some hormone values (A60: Pearson's r=0.27, p=0.035; Adif: r=0.27, p=0.038; Aauc: r=0.25, p=0.055; C60: r=0.23, p=0.079; Cauc: r=0.24, p=0.059), suggesting that pituitary–adrenal responses to the DEX/CRH test tend to become higher as severity of depression increases. When confounding factors of age and gender were examined, however, there was a highly significant positive correlation between age and HDRS scores (r=0.39, p=0.002), although there was no significant difference in mean HDRS score between males and females (t=−1.2, df=59, p=0.23). Thus, the observed correlation between HDRS scores and the DEX/CRH test might be explained, at least in part, by the correlation between HDRS scores and age in our sample. No significant difference was found in hormonal measures between patients on medication and patients without medication on admission (Table 2). When the diagnosis groups (unipolar depression with single episode, recurrent unipolar depression, and bipolar disorder) were compared, ACTH responses differed consistently with a significant difference (Adif) and a nonsignificant trend (A0 and A60) (Table 2). Against our expectation, ACTH responses were high in the decreasing order of patients with unipolar depression with single episode, those with bipolar disorder, and those with recurrent unipolar depression. Comparisons of confounding factors of age, gender, and HDRS score revealed no significant difference among these three diagnosis groups (age: p=0.35 by one-way ANOVA; gender: p=0.37 by χ2 test; HDRS score: p=0.52 by one-way ANOVA).
Repeated Assessments of the DEX/CRH Test
Among patients, 35 were repeatedly assessed with the DEX/CRH test on admission and before discharge. The mean HDRS scores as well as plasma concentrations of ACTH and cortisol before and after treatment are shown in Table 3. HDRS scores lowered substantially due to treatment. All values of ACTH and cortisol decreased significantly after treatment. When suppression status was examined, the distributions of nonsuppressors, intermediate suppressors, and suppressors changed significantly after treatment (14, 51, and 34%, respectively, on admission, in contrast to 11, 14, and 74%, respectively, before discharge; p=0.004 by the Wilcoxon paired signed-ranks test). No significant correlation was found between changes in HDRS scores and changes in any of hormonal measures in the 35 patients.
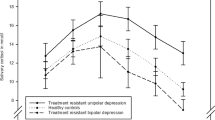
Restoration from HPA axis abnormalities was examined separately in patients who underwent ECT and in patients who underwent pharmacotherapy alone. Figure 1 shows time-course changes of the mean plasma concentrations of cortisol in patients who underwent ECT (N=12) and in patients who did not (N=23). As shown in Figure 1, the magnitude of hormonal response reduction appeared to be greater in patients who underwent ECT in addition to pharmacotherapy compared with those who underwent pharmacotherapy alone. As shown in Table 3, indeed, changes in hormone concentrations between pre- and post-treatment were significant only for Aauc, C60, and Cauc in the pharmacotherapy group, while all values of both ACTH and cortisol, except for A0, changed significantly in the ECT group.
DISCUSSION
We assessed the DEX/CRH test as a state-dependent marker to monitor HPA axis abnormalities in depression. We found that elderly and female individuals tended to show increased pituitary–adrenal responses to the DEX/CRH test compared to young and male individuals, respectively. We confirmed that pituitary–adrenal responses to the DEX/CRH test are enhanced in depressed patients compared to controls. Severity of depression correlated with the DEX/CRH test results, although this was explained, at least in part, by a positive correlation between age and severity in our patients. Medication per se was unrelated to DEX/CRH test results. For patients who were repeatedly assessed with the DEX/CRH test, hormonal responses were reduced after treatment. This reduction was observed predominantly in patients who underwent ECT in addition to pharmacotherapy rather than in those who underwent pharmacotherapy alone.
Effects of Age and Gender
In our patients, all the mean plasma concentrations of hormones were higher in the aged patient group (>50 years) than in the young patient group (⩽50 years), although a statistically significant difference was found only for A0 and a nonsignificant trend for Cauc. Previous studies have provided conflicting results as to the possible effects of age on hormonal responses to the DEX/CRH test. von Bardeleben and Holsboer (1991) reported that the cortisol response to the DEX/CRH test increased with age in patients with depression but was absent in controls. Heuser et al (1994a) examined healthy subjects and found that hormonal responses to the DEX/CRH test were enhanced in older subjects (aged 60–84 years) compared to younger subjects (22–48 years). In line with this, Kudielka et al (1999) found that healthy elderly women (60–75 years) exhibited a markedly enhanced cortisol response to the DEX/CRH test compared to young controls (20–31 years). In contrast, a more recent study found no significant effect of age on hormonal responses to the DEX/CRH test in acutely depressed inpatients (Kunzel et al, 2003). Studies in rats have provided evidence that aged animals tend to show enhanced hormonal responses to the DEX/CRH test compared to young animals, and that vasopressin is involved in these age-associated changes (Hatzinger et al, 1996, 2000; Revskoy and Redei, 2000). Our results support the possibility that older age is associated with enhanced pituitary–adrenal responses to the DEX/CRH test, at least in depressed patients.
With respect to gender, female depressed and normal subjects were reported to have increased hormonal responses to the DEX/CRH test in comparison with male counterparts (Heuser et al, 1994a; Kunzel et al, 2003). Our results give further support for this gender difference. Based on our data, responses to pretreatment with DEX (A0 and C0) did not seem to be consistently different between males and females among young patients, aged patients, and controls (Table 1). However, hormonal responses to the subsequent injection of CRH as manifested by Adif and Cdif were consistently higher in females than in males for all the three groups. These results suggest that gender difference in hormonal responses to the DEX/CRH test might be attributable predominantly to that in hormonal responses to CRH.
Patients vs Controls
When young patients were compared with controls, all hormonal responses of both ACTH and cortisol were consistently higher in patients on admission than in controls (Table 1). The differences in C0, C60, and Cauc were statistically significant. The differences in A0, A60, Adif, Aauc, and Cdif failed to reach statistical significance, which was probably attributable to the lack of statistical power due to the small number of young patients (N=22). Even when post hoc analyses were performed in 18 patients and the same number of controls, matched for both age and gender, results were similar. Overall, our data provide further evidence for enhanced HPA activity detected with the DEX/CRH test in depressed patients.
Clinical Variables and DEX/CRH Test
We found a positive correlation between HDRS scores on admission and hormonal values, suggesting that pituitary–adrenal responses to the DEX/CRH test tend to become higher as severity of depression increases. This observation is in accordance with previous studies (von Bardeleben and Holsboer, 1991; Rybakowski and Twardowska, 1999; Kunzel et al, 2003). In our sample, however, there was a highly significant correlation between HDRS scores and age (p=0.002), which was stronger than the correlation between HDRS scores and hormonal measures, indicating that the observed correlation between HDRS scores and the DEX/CRH test might be explained, at least in part, by the correlation between HDRS scores and age. Zobel et al (2004) recently reported that a decrease in cortisol response to the DEX/CRH test was more closely related to an improvement in specific brain functions (especially working memory) than to the global severity of depression.
Hormonal measures were not significantly different between patients on medication and patients without medication on admission, indicating that the fact of being on medication per se was unrelated to DEX/CRH test results. This observation is in line with the finding of Kunzel et al (2003), that is, the presence or absence of antidepressant treatment, the type of antidepressant treatment, or the number of ineffective antidepressant treatment trials during the index episode had no effect on hormonal responses to the DEX/CRH test. One exceptional drug is mirtazapine, an antidepressant known to acutely inhibit cortisol secretion in healthy subjects; the drug was shown to attenuate rapidly HPA axis hyperactivity in depressed patients via direct pharmacoendocrinological effects, which was not necessarily related to clinical improvement (Schule et al, 2003).
With respect to possible differences in DEX/CRH test results among the diagnosis groups (unipolar depression with single episode, recurrent unipolar depression, and bipolar disorder), ACTH responses were high in the decreasing order of patients with unipolar depression with single episode, those with bipolar disorder, and those with recurrent unipolar depression. This finding was unexpected because at least three research groups had obtained evidence that HPA abnormalities as detected with the DEX/CRH test became more pronounced as the number of previous episodes increased (Hatzinger et al, 2002; Kunzel et al, 2003; Gervasoni et al, 2004). Inconsistency between previous studies and ours might be attributable to the effects of confounding factors of age, gender, and HDRS score. However, we found no significant difference in any of these variables among the three diagnosis groups. Alternatively, differences in ACTH responses may have occurred by chance, considering that there was no significant difference in cortisol responses among the diagnosis groups. Further investigations are required to draw any conclusion.
Repeated Assessments of the DEX/CRH Test
When depressed patients were repeatedly assessed with the DEX/CRH test on admission and before discharge, all the measures of ACTH and cortisol were significantly reduced after treatment. Our results are consistent with previous studies reporting a reduction in hormonal responses to the DEX/CRH test after successful pharmacotherapy with antidepressants (Holsboer-Trachsler et al, 1991; Heuser et al, 1996; Deuschle et al, 1997; Baghai et al, 2002; Frieboes et al, 2003), suggesting that alterations in the HPA axis as detected with the DEX/CRH test are, at least in part, state dependent.
When suppression status was examined, the distributions of nonsuppressors, intermediate suppressors, and suppressors significantly changed after treatment (14, 51, and 34%, respectively, on admission; 11, 14, and 74%, respectively, before discharge) (p=0.004). However, the difference in the rate of nonsuppressors (defined as C0 of ⩾5 μg/dl) alone (14 vs 11%) was not statistically significant in our patients. This finding indicates that pretreatment with DEX alone (ie conventional DST) lacks sensitivity to monitor changes in HPA abnormalities during the treatment course of depressed patients and that the combination of CRH with DEX (ie DEX/CRH test) is much more sensitive. The definition of ‘intermediate suppressors’ (defined as C0 of <5 μg/dl and C60 of ⩾5 μg/dl) might be useful in future studies and in the clinical setting.
When patients who underwent pharmacotherapy alone and patients who underwent ECT in addition to pharmacotherapy were examined separately, the magnitude of hormonal response reduction appeared to be greater in the latter than in the former, suggesting that ECT has an additional effect on restoration from HPA axis abnormalities besides the effect of pharmacotherapy. This finding is consistent with the results from several conventional DST studies that reported a positive correlation between hormonal responses to ECT and the normalization of the HPA system (Albala et al, 1981; Papakostas et al, 1981; Grunhaus et al, 1987; Devanand et al, 1991). However, controversial results have also been reported (Coryell, 1986; Fink et al, 1987). This inconsistency in the literature may be due in part to the immediate effects of ECT, which activates HPA axis (Aperia et al, 1984; Swartz and Chen, 1985). Devanand et al (1991) measured plasma cortisol concentrations in depressed patients who had undergone ECT three times, that is, pre-ECT, immediately post-ECT, and 1 week after ECT. They found that plasma cortisol concentrations decreased significantly from pretreatment to immediately post-treatment and then further decreased during the first week after the ECT course. Based on this observation, Devanand et al (1991) pointed out that it may be necessary to wait 1 or more weeks in repeated DST studies in patients receiving ECT. We conducted the post-treatment DEX/CRH test before discharge, but not immediately after ECT, which might have reduced the possible effects of postictal increases in plasma ACTH and cortisol concentrations.
Proposal for a Simpler Test Protocol
In our comparisons between patients and controls, cortisol responses were more clearly different from ACTH responses between the two groups. Furthermore, ACTH and cortisol responses generally tend to parallel as pointed out by Heuser et al (1994b). Therefore, the measurement of ACTH might add little information. In our study, core results were derivable from the C0, C60, and Cdif values. A simpler test protocol might hence be available which measures plasma cortisol concentrations only twice at 1500 hours (immediately before CRH injection) and 1600 hours (1 h later). Such a simpler protocol might save time and cost without losing essential information to be obtained from the DEX/CRH test and might be practical in the clinical setting. However, the current results were based on observations on in-patients with major depressive episode who were acutely ill, and data on chronic depression or minor depression are unavailable in the current study. Further studies are warranted to draw conclusions as to the appropriateness of such a simple test protocol.
Limitations
The present study involves several limitations. First, the sample size was not very large, which might have given rise to type II errors. Second, all patients were in-patients and acutely ill; hence, severe forms of depression might be over-represented in our sample. It is possible that the sensitivity of the DEX/CRH test might be lower in outpatients and patients with chronic depression as, respectively, reported by Gervasoni et al (2004) and Watson et al (2002). Third, the majority of patients were medicated with antidepressants, which might have influenced the DEX/CRH results. Although antidepressants per se have been shown not to influence test results (Heuser et al, 1996; Kunzel et al, 2003), it is possible that the effects of drug treatment already emerged in part of patients. Furthermore, drugs may have exerted some effects on the degradation rate of DEX and in turn influenced DEX/CRH test results. However, a recent study of Watson et al (2004) compared DEX levels between patients and controls and found that there was no difference in DEX levels between the two groups, suggesting that an effect of psychotropic medication on cortisol output via DEX metabolism appears unlikely. Finally, the detection limits for the hormone assay may have reduced the sensitivity, particularly ACTH responses, of the DEX/CRH test.
Conclusions
In conclusion, we obtained additional evidence for enhanced HPA axis activity, which was detected with the DEX/CRH test when Japanese patients with major depressive episode were compared with controls. Age, gender, but not the fact of being on medication per se, are shown to be associated with DEX/CRH test results. Repeated DEX/CRH tests on admission and before discharge provided clear evidence that the DEX/CRH test is a sensitive test as a state-dependent marker to monitor HPA axis abnormalities in Japanese patients with depression. Furthermore, our results suggest that normalization of HPA axis occurs with clinical responses to ECT as well as pharmacotherapy in depressed patients.
References
Albala AA, Greden JF, Tarika J, Carroll BJ (1981). Changes in serial dexamethasone suppression tests among unipolar depressive receiving electroconvulsive treatment. Biol Psychiatry 16: 551–560.
American Psychiatric Association (1987). The dexamethasone suppression test: an overview of its current status in psychiatry: the APA task force on laboratory tests in psychiatry. Am J Psychiatry 144: 1253–1262.
American Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th edn. American Psychiatric Association: Washington, DC.
Aperia B, Thoren M, Zettergren M, Wetterberg L (1984). Plasma pattern of adrenocorticotropin and cortisol during electroconvulsive therapy in patients with major depressive illness. Acta Psychiatr Scand 70: 361–369.
Baghai TC, Schule C, Zwanzger P, Minov C, Holme C, Padberg F et al (2002). Evaluation of a salivary based combined dexamethasone/CRH test in patients with major depression. Psychoneuroendocrinology 27: 385–399.
Carroll BJ (1982). The dexamethasone suppression test for melancholia. Br J Psychiatry 140: 292–304.
Carroll BJ, Feinberg M, Greden JF, Tarika J, Albala AA, Haskett RF et al (1981). A specific laboratory test for the diagnosis of melancholia: standardization, validation, and clinical utility. Arch Gen Psychiatry 38: 15–22.
Coryell W (1986). Are serial dexamethasone suppression tests useful in electroconvulsive therapy? J Affect Disord 10: 59–66.
Deuschle M, Schmider J, Weber B, Standhardt H, Korner A, Lammers CH et al (1997). Pulse-dosing and conventional application of doxepin: effects on psychopathology and hypothalamus-pituitary-adrenal (HPA) system. J Clin Psychopharmacol 17: 156–160.
Deuschle M, Schweiger U, Gotthardt U, Weber B, Korner A, Schmider J et al (1998). The combined dexamethasone/corticotropin-releasing hormone stimulation test is more closely associated with features of diurnal activity of the hypothalamo-pituitary-adrenocortical system than the dexamethasone suppression test. Biol Psychiatry 43: 762–766.
Devanand DP, Decina P, Sackeim HA, Hopkins N, Novacenko H, Malitz S (1987). Serial dexamethasone suppression tests in initial suppressors and nonsuppressors treated with electroconvulsive therapy. Biol Psychiatry 22: 463–472.
Devanand DP, Sackeim HA, Lo ES, Cooper T, Huttinot G, Prudic J et al (1991). Serial dexamethasone suppression tests and plasma dexamethasone levels: effects of clinical response to electroconvulsive therapy in major depression. Arch Gen Psychiatry 48: 525–533.
Fink M, Gujavarty K, Greenberg L (1987). Serial dexamethasone suppression tests and clinical outcome in ECT. Convuls Ther 3: 111–120.
Frieboes RM, Sonntag A, Yassouridis A, Eap CB, Baumann P, Steiger A (2003). Clinical outcome after trimipramine in patients with delusional depression—a pilot study. Pharmacopsychiatry 36: 12–17.
Gervasoni N, Bertschy G, Osiek C, Perret G, Denis R, Golaz J et al (2004). Cortisol responses to combined dexamethasone/CRH test in outpatients with a major depressive episode. J Psychiatr Res 38: 553–557.
Greden JF, Gardner R, King D, Grunhaus L, Carroll BJ, Kronfol Z (1983). Dexamethasone suppression tests in antidepressant treatment of melancholia: the process of normalization and test–retest reproducibility. Arch Gen Psychiatry 40: 493–500.
Grunhaus L, Zelnik T, Albala AA, Rabin D, Haskett RF, Zis AP et al (1987). Serial dexamethasone suppression tests in depressed patients treated only with electroconvulsive therapy. J Affect Disord 13: 233–240.
Hamilton M (1967). Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6: 278–296.
Hatzinger M, Hemmeter UM, Baumann K, Brand S, Holsboer-Trachsler E (2002). The combined DEX–CRH test in treatment course and long-term outcome of major depression. J Psychiatr Res 36: 287–297.
Hatzinger M, Reul JM, Landgraf R, Holsboer F, Neumann I (1996). Combined dexamethasone/CRH test in rats: hypothalamo-pituitary-adrenocortical system alterations in aging. Neuroendocrinology 64: 349–356.
Hatzinger M, Wotjak CT, Naruo T, Simchen R, Keck ME, Landgraf R et al (2000). Endogenous vasopressin contributes to hypothalamic-pituitary-adrenocortical alterations in aged rats. J Endocrinol 164: 197–205.
Heuser I, Yassouridis A, Holsboer F (1994b). The combined dexamethasone/CRH test: a refined laboratory test for psychiatric disorders. J Psychiatr Res 28: 341–356.
Heuser IJ, Gotthardt U, Schweiger U, Schmider J, Lammers CH, Dettling M et al (1994a). Age-associated changes of pituitary-adrenocortical hormone regulation in humans: importance of gender. Neurobiol Aging 15: 227–231.
Heuser IJ, Schweiger U, Gotthardt U, Schmider J, Lammers CH, Dettling M et al (1996). Pituitary-adrenal-system regulation and psychopathology during amitriptyline treatment in elderly depressed patients and normal comparison subjects. Am J Psychiatry 153: 93–99.
Holsboer F (1995). Neuroendocrinology of mood disorders. In: Bloom FE, Kupfer DJ (eds). Psychopharmacology: The Fourth Generation of Progress. Raven Press: New York. pp 957–969.
Holsboer F, Lauer CJ, Schreiber W, Krieg JC (1995). Altered hypothalamic-pituitary-adrenocortical regulation in healthy subjects at high familial risk for affective disorders. Neuroendocrinology 62: 340–347.
Holsboer F, Liebl R, Hofschuster E (1982). Repeated dexamethasone suppression test during depressive illness: normalisation of test result compared with clinical improvement. J Affect Disord 4: 93–101.
Holsboer F, von Bardeleben U, Wiedemann K, Muller OA, Stalla GK (1987). Serial assessment of corticotropin-releasing hormone response after dexamethasone in depression. Implications for pathophysiology of DST nonsuppression. Biol Psychiatry 22: 228–234.
Holsboer-Trachsler E, Stohler R, Hatzinger M (1991). Repeated administration of the combined dexamethasone-human corticotropin releasing hormone stimulation test during treatment of depression. Psychiatry Res 38: 163–171.
Ising M, Lauer CJ, Holsboer F, Modell S (2005). The Munich vulnerability study on affective disorders: premorbid neuroendocrine profile of affected high-risk probands. J Psychiatr Res 39: 21–28.
Kudielka BM, Schmidt-Reinwald AK, Hellhammer DH, Kirschbaum C (1999). Psychological and endocrine responses to psychosocial stress and dexamethasone/corticotropin-releasing hormone in healthy postmenopausal women and young controls: the impact of age and a two-week estradiol treatment. Neuroendocrinology 70: 422–430.
Kunugi H, Urushibara T, Nanko S (2004). Combined DEX/CRH test among Japanese patients with major depression. J Psychiatr Res 38: 123–128.
Kunzel HE, Binder EB, Nickel T, Ising M, Fuchs B, Majer M et al (2003). Pharmacological and nonpharmacological factors influencing hypothalamic-pituitary-adrenocortical axis reactivity in acutely depressed psychiatric in-patients, measured by the Dex–CRH test. Neuropsychopharmacology 28: 2169–2178.
Oshima A, Yamashita S, Owashi T, Murata T, Tadokoro C, Miyaoka H et al (2000). The differential ACTH responses to combined dexamethasone/CRH administration in major depressive and dysthymic disorders. J Psychiatr Res 34: 325–328.
Papakostas Y, Fink M, Lee J, Irwin P, Johnson L (1981). Neuroendocrine measures in psychiatric patients: course and outcome with ECT. Psychiatry Res 4: 55–64.
Plotsky PM, Owens MJ, Nemeroff CB (1998). Psychoneuroendocrinology of depression: hypothalamic-pituitary-adrenal axis. Psychiatr Clin N Am 21: 293–307.
Revskoy S, Redei E (2000). Decreased in vitro sensitivity to dexamethasone in corticotropes from middle-age rats. Exp Gerontol 35: 237–242.
Rybakowski JK, Twardowska K (1999). The dexamethasone/corticotropin-releasing hormone test in depression in bipolar and unipolar affective illness. J Psychiatr Res 33: 363–370.
Schmider J, Lammers CH, Gotthardt U, Dettling M, Holsboer F, Heuser IJ (1995). Combined dexamethasone/corticotropin-releasing hormone test in acute and remitted manic patients, in acute depression, and in normal controls: I. Biol Psychiatry 38: 797–802.
Schule C, Baghai T, Zwanzger P, Ella R, Eser D, Padberg F et al (2003). Attenuation of hypothalamic-pituitary-adrenocortical hyperactivity in depressed patients by mirtazapine. Psychopharmacology (Berlin) 166: 271–275.
Schule C, Baghai T, Zwanzger P, Minov C, Padberg F, Rupprecht R (2002). Sleep deprivation and hypothalamic-pituitary-adrenal (HPA) axis activity in depressed patients. J Psychiatr Res 35: 239–247.
Swartz CM, Chen JJ (1985). Electroconvulsive therapy-induced cortisol release: changes with depressive state. Convuls Ther 1: 15–21.
von Bardeleben U, Holsboer F (1989). Cortisol response to a combined dexamethasone–human corticotrophin-releasing hormone challenge in patients with depression. J Neuroendocrinol 1: 485–488.
von Bardeleben U, Holsboer F (1991). Effect of age on the cortisol response to human corticotropin-releasing hormone in depressed patients pretreated with dexamethasone. Biol Psychiatry 29: 1042–1050.
Watson S, Gallagher P, Del-Estal D, Hearn A, Ferrier IN, Young AH (2002). Hypothalamic-pituitary-adrenal axis function in patients with chronic depression. Psychol Med 32: 1021–1028.
Watson S, Gallagher P, Ritchie JC, Ferrier IN, Young AH (2004). Hypothalamic-pituitary-adrenal axis function in patients with bipolar disorder. Br J Psychiatry 184: 496–502.
Zobel AW, Nickel T, Sonntag A, Uhr M, Holsboer F, Ising M (2001). Cortisol response in the combined dexamethasone/CRH test as predictor of relapse in patients with remitted depression: a prospective study. J Psychiatr Res 35: 83–94.
Zobel AW, Schulze-Rauschenbach S, von Widdern OC, Metten M, Freymann N, Grasmader K et al (2004). Improvement of working but not declarative memory is correlated with HPA normalization during antidepressant treatment. J Psychiatr Res 38: 377–383.
Zwanzger P, Baghai TC, Padberg F, Ella R, Minov C, Mikhaiel P et al (2003). The combined dexamethasone–CRH test before and after repetitive transcranial magnetic stimulation (rTMS) in major depression. Psychoneuroendocrinology 28: 376–385.
Acknowledgements
We thank Ms Kazuko Sakai for her substantial assistance. This study was supported in part by a grant from the Mitsubishi Pharma Corporation and by a research grant from the Ministry of Health, Labor, and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kunugi, H., Ida, I., Owashi, T. et al. Assessment of the Dexamethasone/CRH Test as a State-Dependent Marker for Hypothalamic-Pituitary-Adrenal (HPA) Axis Abnormalities in Major Depressive Episode: A Multicenter Study. Neuropsychopharmacol 31, 212–220 (2006). https://doi.org/10.1038/sj.npp.1300868
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300868
Keywords
This article is cited by
-
Glucocorticoid Receptor Down-Regulation Affects Neural Stem Cell Proliferation and Hippocampal Neurogenesis
Molecular Neurobiology (2023)
-
Bidirectional relationship between heroin addiction and depression: Behavioural and neural studies
Current Psychology (2022)
-
Gradient of electro-convulsive therapy’s antidepressant effects along the longitudinal hippocampal axis
Translational Psychiatry (2021)
-
Ex vivo glucocorticoid receptor-mediated IL-10 response predicts the course of depression severity
Journal of Neural Transmission (2021)
-
Depressive Symptoms Mediate the Relationship between Emotional Cutoff and Type 2 Diabetes Mellitus
International Journal of Behavioral Medicine (2019)