Abstract
Introduction: Bowel management is a significant source of concern for patients with spinal cord injury (SCI) and may significantly alter quality of life. The effect of colostomy formation on both quality of life and time taken for bowel care is well recorded. We report our experience of intestinal stoma formation in SCI patients.
Methods: Medical records from the spinal unit, operating theatres and stoma clinics were reviewed to identify SCI patients for whom a stoma had been formed. Patients were interviewed using a standard questionnaire. Average age at injury was 29 years (range 6–62 years). Mean time from injury to stoma formation was 17 years (range 0–36.25 years) and the mean period of poor bowel function prior to stoma was 8 years (range 1.5–25).
Results: The average time spent on bowel care per week decreased from 10.3 h (range 3.5–45) prior to stoma formation to 1.9 h (range 0.5–7.75) afterwards (P<0.0001, paired t-test). In all, 18 patients felt that a stoma gave them greater independence and quality of life was described as much better by 25 patients. Complications occurred in 14 patients – eight described leakage of mucus and occasionally blood and pus per rectum, three developed parastomal hernias and three developed bowel obstruction.
Conclusion: Elective stoma formation is a safe and well-accepted treatment for the management of chronic gastrointestinal symptoms in patients with SCI.
Similar content being viewed by others
Introduction
Increased longevity among patients with spinal cord injury (SCI) has resulted in chronic problems becoming a significant source of disability. Chronic gastrointestinal problems such as abdominal distension, megacolon, incontinence and difficulty with bowel evacuation are significant problems. Recent research suggests that bowel management is a significant source of concern for patients and may significantly alter quality of life.1,2,3 The failure of conservative measures to treat these chronic problems in some patients has led to the use of elective surgical treatments such as anterior sacral root stimulation,4,5 antegrade colonic lavage6,7,8 and stoma formation.9,10 The effect of colostomy formation on both quality of life11 and time taken for bowel care9,10 is well recorded, including data from our own group.
We report our increased experience of intestinal stoma formation in SCI patients with data from the largest reported series to date. We also reviewed the incidence of complications in these patients, particularly among earlier patients in the series.
Patients and methods
Medical records from the spinal unit, operating theatres and stoma clinics were reviewed and cross-referenced to identify SCI patients for whom a stoma had been formed. Between March 1986 and March 2002 there were 35 such patients of whom three had died. None of the deaths were related to the stoma surgery. The notes of the remaining 32 patients (27 male, 5 female) were examined and this information was collated with responses to a standard questionnaire (Figure 1).
A total of 28 patients had an LIF colostomy, two had an RIF ileostomy and two had a colostomy followed later by an ileostomy.
Average patient age at injury was 28.9 years (range 6–62 years). The mean time from injury to stoma formation was 17.1 years (range 0–36.25 years) and the mean period of poor bowel function prior to stoma was 8 years (range 1.5–25). The level of neurological injury, where known, was cervical in 10 patients, thoracic in 18 and lumbar in three. The cause of injury in males was traumatic in all bar one patient who suffered a prolapsed intervertebral disc. The causes of injury in females were arachnoiditis, disc prolapse, transverse myelitis, a spinal astrocytoma, and a progressive congenital disorder.
The indications for surgery were constipation in 23, faecal incontinence in four, sepsis in two, malignancy in one, pain in one and perineal trauma at the time of injury in one.
Results
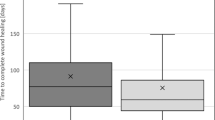
The average time spent on bowel care per week decreased (Figure 2) from 10.3 h (range 3.5–45) prior to stoma formation to 1.9 h (range 0.5–7.75) afterwards (P<0.0001, paired t-test). All patients felt that their bowel care was easier after stoma formation.
Not all patients answered every question and hence the totals represent the numbers of answers for each question. In all, 18 patients felt that a stoma gave them greater independence and 12 felt that it made no difference. One patient felt that his independence was decreased by a stoma as he became dependent on his partner, despite a significant decrease in time spent on bowel care (n=31). Quality of life after stoma formation was described as much better by 25 patients, better by five and worse by one patient (n=31).
In total, 25 patients wished that they had been offered a stoma earlier, although five patients did not (n=30). No patient wished for a stoma reversal, even the patient whose quality of life was worse.
The mean follow-up after stoma formation was 4.6 years (range 0.25–15.75)
Complications
There were no surgically related deaths in this series. Complications occurred in 14 patients (43.75%). Eight patients described leakage of mucus and occasionally blood and pus per rectum. In five patients this was profuse or persistent enough to warrant excision of the distal portion of bowel. One patient within this group developed a faecal fistula postoperatively that required further surgery and eventual total colectomy with formation of an end ileostomy.
Three patients developed parastomal hernias. One of them underwent a repair but has subsequently developed an asymptomatic recurrence.
Two patients developed bowel obstruction, one of whom required a laparotomy.
One patient undergoing a laparoscopically assisted Trephine colostomy had the distal end of bowel brought out to the abdominal surface and the proximal end closed inadvertently. She required a laparotomy to repair the situation.
Discussion
Previous publications describe the formation of an intestinal stoma in SCI patients for management problems, including chronic gastrointestinal symptoms,10 decubitus ulcers,9 anal cancer,10 rectal cancer,10 trauma,11 bowel obstruction,11 and rectovesical fistula.11 The majority of patients in this series (27 of 32) underwent formation of a stoma to manage chronic gastrointestinal symptoms. Two patients had severe perianal sepsis and one had an anal cancer. This is the largest published series of elective surgery for chronic gastrointestinal problems in SCI patients.
As in previous reports this series confirms a statistically significant decrease in time spent on bowel care after stoma formation. Many patients commented that prior to surgery attention to bowel care was followed by a significant period of fatigue. This was not a feature after stoma formation.
The average period of poor bowel function in this series was 8 years and it may be suggested that stoma formation should be offered at an earlier stage than is current practice. Five patients would not have wished to be offered a stoma earlier. The average time spent on bowel care before (9.8 versus 10 h/week) and after (2.25 versus 1.8 h/week) surgery, in these five patients was not significantly different from the other patients. This suggests that differences in time spent on bowel care are not the reason for this decision, although care should be taken in evaluating the result due to the small numbers in one group. However, this need not deter the clinician from earlier discussion of stoma formation with patients who have bowel management problems.
There was no formal algorithm for proposing a stoma in these patients. However, the main cause for referral to the surgeons was the amount of time spent on bowel care sometimes in combination with other symptoms such as abdominal pain. Colonic transit times were not evaluated as it was felt that they would not aid the decision-making process. Increasingly, patients are self-selecting by requesting stoma formation, having seen the positive impact on other patients with similar problems. There were no formal contraindications and each case was considered on its own merit.
Complication rates after stoma formation in SCI patients vary. Craven and Etchells3 report mucoid discharge as the only long-term complication. Stone et al9 report both early and long-term complication rates of 15%. Early and long-term complication rates in this series were 6 and 37.5%, respectively. Although these are significant, it is hoped that our increasing experience of stoma formation in these patients will lead to a decrease in the complication rate.
Rigorous attention to detail when performing a Trephine colostomy will help to avoid using the distal end of the colon as an end stoma.12
Two patients had an episode of bowel obstruction. In one case this occurred in the initial postoperative period at the site tunnel immediately proximal to the stoma. This was resolved at laparotomy. The second case occurred late in a patient who had a laparotomy and LIF colostomy formation. The presumed adhesional small bowel obstruction settled with conservative management. With the increasing use of the Trephine and laparoscopic techniques for stoma formation the development of adhesions may well be decreased.
Eight patients described leakage of mucus and occasionally blood and pus per rectum. Although none of these patients has been assessed endoscopically, it is probable that they have symptomatic diversion colitis. This is a well-recognised entity that often runs a subclinical course.13,14 The commonest presentation in symptomatic patients with SCI is mucus discharge per rectum.15
Definitive management of symptomatic patients with diversion colitis involves an anastomosis to restore the faecal stream,15 something that is not often practical in the patient with SCI. Patients in this series with persistent or profuse discharge underwent excision of the defunctioned segment with no prior attempt at medical management. However, recent data suggest that medical management of this problem is possible. Administration of short-chain free fatty acid enemas,16 which provide recognised nutrients for the colonocyte,17 have been effective and the use of steroid enemas has also met with some success.18 Hence, more radical surgery may be avoided in fixture patients with similar symptoms by early medical management.
Conclusion
Elective stoma formation is a safe and well-accepted treatment for the management of chronic gastrointestinal symptoms in patients with SCI. We feel that this alternative does not mean a failure of care and should be made available at an earlier stage than is currently the case. Complication rates in this series were high but new strategies for stoma formation and management in the SCI patient should help to reduce them in the future.
References
Glickman S, Kamm M . Bowel dysfunction in spinal cord injury patients. Lancet 1996; 347: 1651–1653.
Han TR, Kim JH, Kwon BS . Chronic gastro-intestinal problems and bowel dysfunction in patients with spinal cord injury. Spinal Cord 1998; 36: 485–490.
Craven ML, Etchells J . A review of outcome of stoma surgery on spinal cord injured patients. J Adv Nurs 1998; 27: 922–926.
Macdonagh RP et al. Control of defaecation in patients with spinal cord injury by stimulation of sacral anterior nerve roots. BMJ 1990; 300: 1494–1497.
Chia YW et al. Microchip implants on the anterior sacral nerve roots in patients with spinal trauma. Does it improve bowel function? Dis Colon Rectum 1996; 39: 690–694.
Malone PS, Ransley PG, Kiely EM . Preliminary report of the antegrade continence enema. Lancet 1990; 336: 1217–1218.
Robertson RW, Lynch AC, Beasley SW, Morreau PN . Early experience with the laparoscopic ACE procedure. Aust NZ J Surg 1999; 69: 308–310.
Hill J, Stott S, MacLennan I . Antegrade enemas for the treatment of severe idiopathic constipation. Br J Surg 1994; 81: 1490–1491.
Stone JM, Wolfe VA, Nino-Murcia M, Perkash I . Colostomy as treatment for complications of spinal cord injury. Arch Phys Med Rehabil 1990; 71: 514–518.
Kelly SR et al. The role of the intestinal stoma in patients with spinal cord injury. Spinal Cord 1999; 37: 211–214.
Randell N et al. Does a colostomy alter quality of life in patients with spinal cord injury? A controlled study. Spinal Cord 2000; 39: 279–282.
Nylund G, Oresland T, Hulten L . The trephine stoma: formation of a stoma without laparotomy. Eur J Surg 1997; 163: 627–629.
Glotzer DJ, Glick ME, Goldman H . Proctitis and colitis following diversion of the fecal stream. Gastroenterology 1981; 80: 438–441.
Ma CK, Gottlieb C, Haas PA . Diversion colitis: a clinico-pathological study of 21 cases. Hum Pathol 1990; 21: 429–436.
Frisbie JH et al. Diversion colitis in patients with myelopathy: clinical, endoscopic and histopathological findings. J Spinal Cord Med 2000; 23: 142–149.
Harig JM, Soergel KH, Komorowski RA, Wood CM . Treatment of diversion colitis with short-chain-fatty acid irrigation. N Engl J Med 1989; 320: 23–28.
Cummings JH et al. Short-chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut 1987; 28: 1221–1227.
Senagore AJ, MacKeigan JM, Scheider M, Ebron JS . Short-chain fatty acid enemas: a cost effective alternative in the treatment of non-specific proctosigmoiditis. Dis Colon Rectum 1993; 35: 923–927.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Branagan, G., Tromans, A. & Finnis, D. Effect of stoma formation on bowel care and quality of life in patients with spinal cord injury. Spinal Cord 41, 680–683 (2003). https://doi.org/10.1038/sj.sc.3101529
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101529
Keywords
This article is cited by
-
Effect of neurogenic bowel dysfunction symptoms on quality of life after a spinal cord injury
Journal of Orthopaedic Surgery and Research (2023)
-
Minor microbial alterations after faecal diversion do not affect the healing process of anus-near pressure injuries in patients with spinal cord injury - results of a matched case-control study
Spinal Cord (2023)
-
Impact of Neurogenic Lower Urinary Tract Dysfunction on Bowel Symptoms
Current Bladder Dysfunction Reports (2023)
-
Guideline for the management of neurogenic bowel dysfunction in spinal cord injury/disease
Spinal Cord (2022)
-
Fecal diversion does not support healing of anus-near pressure ulcers in patients with spinal cord injury—results of a retrospective cohort study
Spinal Cord (2022)