Abstract
Study Design: Case report.
Objectives: To report a case of a thoracic intramedullary spinal cord metastasis of ovarian tumor in a 59-year-old woman.
Setting: Shiga, Japan.
Case Report: A case of a thoracic intramedullary spinal cord metastasis of ovarian tumor in a 59-year-old woman is reported. She received abdominal ovariectomy for the ovarian adenocarcinoma 4 years before she suffered from back pain and showed neurological symptoms. The thoracic intramedullary lesion was confirmed by preoperative magnetic resonance imaging. She showed complete paralysis before operation. The excision of the tumor was achieved through the posterior approach. Histologically, the diagnosis of metastasis of adenocarcinoma was made.
Conclusion: Although she did not show any postoperative neurologic recovery, her general condition was good and there was no evidence of recurrence 24 months after surgery.
Similar content being viewed by others
Introduction
Intramedullary spinal cord metastasis is uncommon, but it has been encountered with increasing frequency with the advent of improved magnetic resonance imaging and chemotherapy.1 Imaging studies have become quite sensitive, but they are still nonspecific for this intramedullary lesion. The open surgical biopsy is the only method of establishing the diagnosis. The present case of ovarian metastasis has been surviving for 24 months after the excision of the tumor without evidence of recurrence. The case study is described here.
Case report
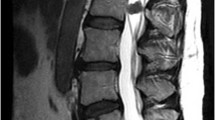
This 59-year-old woman presented with a 2-month history of low back pain and right lower extremity pain. She suffered progressive deterioration, resulting in gait disturbance and bladder dysfunction, so she entered our hospital on emergency. She suffered from stage IIIc ovarian tumor with peritoneal implants and received abdominal ovariectomy followed by chemotherapy 4 years previously. The histological diagnosis of adenocarcinoma was made. Neurologic examination at admission revealed complete paralysis of the lower extremities, with anesthesia below L1 level. Plain X-ray of the spine was normal. By a lumbar tap, the cerebrospinal fluid showed a clear colorless fluid, with a protein content of 35 mg/dl. Magnetic resonance (MR) imaging was performed with a 1.5 T magnet and surface coil (Signa Horizon, GE Medical Systems, Milwaukee, WI, USA). T1-weighted (450/14/2 [repetition time/echo time/excitations]) sagittal spin-echo images with a 4 mm section thickness were obtained before and after an intravenous injection of gadolinium. T1-weighted (550/14/2) axial spin-echo images were obtained using the same section thickness. T2-weighted (3500/105/4) sagittal fast spin-echo images with a 4 mm section thickness were also obtained. The T2-weighted image showed the intramedullary high-intensity lesion that extended to the rostral side from the Th10 level (Figure 1a). This high-intensity lesion might be caused by edematous swelling of the spinal cord. T1-weighted MR imaging of the thoracic spine after an intravenous injection of gadolinium showed an enhancing intramedullary spinal cord lesion at the Th10 segment (Figure 1b). The lesion showed ring enhancement at the right side on the axial enhanced T1-weighted image (Figure 1c). A myelogram demonstrated a subtle enlargement of the spinal cord at the Th10 level. The computed tomographic scan and 99mTc scintigraphy could not detect any other metastatic site intracranially, intra-abdominally, elsewhere in the spine, or in the breast. The excision of the tumor was performed to establish the diagnosis, expecting a longer survival.
The sagittal MR image of the thoracic spine on the T2-weighted image (a) shows the edematous swelling of the spinal cord and the heterogeneous lesion (arrowheads), including high and low intensities. The intramedullary high-intensity lesion (arrows) is extended to the rostral side from the Th10 level. The sagittal (b) and axial (c) MR images of the thoracic spine on T1-weighted images following injection of gadolinium demonstrate an abnormal intramedullary lesion (arrows) at the Th10 vertebral level with a rim enhancement on the right side
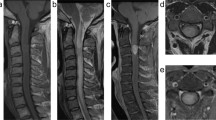
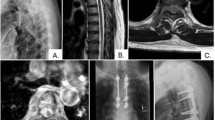
The patient was positioned prone using the Andrews spinal surgery table. After the laminectomy of Th10, and partial laminectomy of Th9 and Th11, the intact underlying dura were opened longitudinally. We found the smooth normal surface of the cord. After we made a longitudinal slight cut on the dorsal surface of the cord, an irregular brown intramedullary lesion was detected (Figure 2). The tumor margin was indistinct from surrounding cord with spotted small hematoma, but no cysts were noted. A piece-by-piece subtotal resection of the tumor was accomplished by microsurgical technique with a curette and a cavitron ultrasonic surgical aspirator (2.5 mm internal diameter). Histologically, the tumor cells were medium to large and were polygonal in shape with ovoid and dark chromatin. The lesion was identified as a poorly differentiated adenocarcinoma that was similar to primary lesion (Figure 3). Postoperatively, she was treated by radiation therapy. The back was immobilized in an orthosis for 3 months. T1-weighted MR imaging of the thoracic spine after the operation showed a reducing intramedullary spinal cord lesion at the Th10 segment (Figure 4). She did not show any neurologic recovery, but now, 24 months after surgery, her general condition is good and there is no evidence of recurrence. She lives in her home using a wheelchair, and we are following her in an out patient clinic.
Discussion
The intramedullary spinal cord is an unusual site of metastatic cancer. The autopsy study of 627 patients with systemic cancer disclosed 13 patients with intramedullary spinal cord metastasis. Lung and breast were the most commonly associated primary cancers, accounting for 54 and 13% of cases, respectively.1 Central nervous system metastasis is rare in patients with ovarian cancer. We could find only one case report of an ovarian cancer with metastatic spread to the intramedullary spinal cord.2 They diagnosed the lesion to be intramedullary spinal cord metastasis on the basis of the clinical presentation and characteristic MR imaging findings. The patient received steroid and radiation, but expired 6 months after the discovery of the intramedullary spinal cord metastasis.
The surgical treatment for the intramedullary spinal cord metastasis is still controversial, since the patients tend to do so poorly on length of survival.3 It was said that the average length of survival in patients of intramedullary spinal cord metastasis followed until death was only 19.5 weeks.1 In selected patients with well-circumscribed margin and limited primaries, gross total resection might improve the length and quality of survival.4 Also, the open biopsy is necessary to establish a definitive diagnosis. In general, the prognosis of stage IIIc ovarian cancer is poor. In this case, we could get a long survival period after surgery. This might be explained by the fact that we performed excision of the single spinal cord metastasis at the operation adding radiation.
References
Connolly Jr ES, Winfree CJ, McCormick PC, Cruz M, Stein BM . Intramedullary spinal cord metastasis: report of three cases and review of the literature. Surg Neural 1996; 46: 329–338.
Thomas AW, Simon SR, Evans C . Intramedullary spinal cord metastases from epithelial ovarian carcinoma. Gynecol Oncol 1992; 44: 195–197.
Grem JL, Burgess J, Trump DL . Clinical features and natural history of intramedullary spinal cord metastasis. Cancer 1985; 56: 2305–2314.
Findlay JM, Bernstein M, Vanderlinden RG, Resch L . Microsurgical resection of solitary intramedullary spinal cord metastasis. Neurosurgery 1987; 21: 911–915.
Acknowledgements
We thank Dr Toshio Kimura for his kind help and helpful discussions.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Isoya, E., Saruhash, Y., Katsuura, A. et al. Intramedullary spinal cord metastasis of ovarian tumor. Spinal Cord 42, 485–487 (2004). https://doi.org/10.1038/sj.sc.3101572
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101572
Keywords
This article is cited by
-
Surgical treatment of spinal intradural carcinoma metastases
Acta Neurochirurgica (2012)
-
Upper cervical intramedullary spinal metastasis of ovarian carcinoma: a case report and review of the literature
Journal of Medical Case Reports (2011)