Abstract
Design:
A prospective inception cohort study with an observational analytic design in a spinal cord injury (SCI) centre hospital.
Objective:
To assess changes in trabecular and compact bone of the tibia and radius prospectively in subjects with SCI.
Subjects:
In total, 10 individuals with an acute SCI.
Methods:
Trabecular and compact bone density of the tibia and radius by peripheral quantitative computerised tomography.
Results:
Analysis of the individual gradients of the curve coefficient showed changes in trabecular bone between −0.19 and −2.46 and in cortical bone between +0.07 and −0.93 in the tibia within 34 months after the SCI. Both trabecular and cortical bone showed a group mean loss of 99 mg/cm3. No changes were observed in the radius.
Conclusion:
There is a major decrease in tibia mineral density over 3 years; however, no change is observed for the radius mineral content. Large interindividual differences existed in the patterns of loss in the tibia bone substance after SCI. These patterns indicate that there is no steady state of bone mineral density following 3 years of spinal cord injury.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a condition known to be associated with osteopenia; a decrease in bone mass below the level of injury. Osteopenia leads in some individuals to osteoporosis with an increased risk of fractures.1,2,3,4,5,6,7 Several authors report that approximately 2 years after the spinal cord injury, a new steady state between bone resorption and formation is re-established. However, this steady state is reached after the patient has lost a significant amount of bone minerals. At 16 months after SCI, bone mineral density (BMD) around the knee is comparable with the values seen in individuals at more than 5 years following SCI.8 Biering-Sørensen et al9 observed bone development longitudinally and report that the decrease in bone mineral content (BMC) of the lower extremities occurs rather uniformly. Another study of this group identified that SCI individuals with fractures of the lower extremities sustained after the injury show lower BMC compared to individuals without fractures.10 One of our previous studies11 observed a loss in trabecular and cortical bone, which was at first sight in line with previously reported results.9,10 However, we found a large intersubject variability through qualitative analysis of the individual patterns of change. Finsen et al12 report contradictory findings. They compared 19 SCI individuals with a median duration of SCI of 4 years with a control group. From this cross-sectional study design the authors derived considerable individual variations in BMD and in the degree of difference in BMD between SCI patients and controls. Furthermore, the degree of osteopenia in the affected limbs seemed to increase with the time of injury and no signs of steady state were corroborated.12
Whole bones are composed of cortical and trabecular bone tissue. This classification of bone tissue is based on relative density. Apparent bone density has a profound influence on the stress–strain behaviour of bone, which is markedly different between these two types of bone tissue. The major physical difference between trabecular and cortical bone is the increased porosity of trabecular bone.13
One of the clinical effects of osteoporosis in paraplegia is spontaneous fracture of long bones.14,15,16 The usual history of trauma and the classical signs of fracture are absent in these patients. Frequently, minor trauma is the cause of fracture.17,18 Frisbie19 attempted to quantify the risk of lower extremity fracture in paraplegia by retrospective analysis of medical records. In total, 33% of the patients in this study sustained 76 fracture events, resulting in 103 fractures (82% in the long bones of the lower extremity). Frisbie19 concluded that there is a markedly increased risk of lower extremity fracture following SCI and that this risk seems to be raised further with ageing. A study of Vestergaard et al20 included 438 SCI patients in which the overall fracture rate (2%/year) was higher than in the normal population (1%/year). Following the SCI the rate increased to a plateau from the third year onward. Before the SCI occurred in these subjects, however, their fracture rate was equal to that of the normal controls.20
Hence, the natural course of bone loss is not known with regard to SCI and injury duration. This prospective study was designed to elucidate the natural course of bone loss in individuals of the SCI population through a time-sequential assessment of the phenomena of bone loss associated with SCI. The aim of this study was to find an answer to the following two questions: First, do changes in BMD following an SCI reach a ‘steady state’ after more than 2 years postinjury? Second, are there high interindividual variations of change in BMD following an SCI? The bony organs chosen were the tibia and the radius.
Methods
Subjects and protocol
A total of 12 subjects with SCI were initially investigated within 5 weeks following the accident that resulted in SCI (t1). Approximately 3½ years after the accident (42±5.9 months), 10 subjects were measured again (t2). All participants signed a statement of informed consent as approved by the Review Board of the University Hospital Balgrist after receiving oral and written information about the research. All subjects had a traumatic SCI. At t2, two subjects were removed from the study because they had moved too far away from the Spinal Cord Injury Center, University Hospital Balgrist. A summary of the 10 subjects completing the study is given in Table 1.
The qualitative and quantitative analysis was performed with the 10 subjects who completed the study, nine males and one female. The subjects were aged 40.9±19.7 years at t2.
Study design
Because of the expected heterogeneity of the population involved, a prospective cohort study with an observational analytic design was chosen.
Bone measurements
Bone density measurements were performed with a Densiscan 1000 (Scanco Medical, CH-8303 Bassersdorf, Switzerland) on the left tibia and on the left radius (unless these bones had been fractured). Two stacks of CT scans were analysed: (1) in the distal tibia epiphysis close to the ankle joint, and (2) in the distal radius epiphysis close to the wrist. To ensure that the CT scans were always made at the same angle relative to the bone axis the extremity involved was measured in an anatomically formed radiolucent cast.
The basic methodology employed in quantitative computed tomography (QCT) scanning involves the computation of the cross-sectional distribution of X-ray attenuation in a body by back-projecting the X-ray transmission measurements acquired at many angles around the body until the spatial arrangement of the absorbing structures can be determined.21 With the information available in QCT scans, it is possible to isolate BMD changes in both cortical and trabecular compartments.13 A detailed description of the examination protocol has been described elsewhere.22,23
Two parameters were derived and calculated for a general characterisation of the measured bone:
Trabecular bone: to determine this bone parameter, the inner core of the bone was assessed. The core area contains only trabecular bone.
Compact bone (ie, cortical bone): this parameter represents the average bone density at the diaphyseal measuring site (bone mass divided by total cross-sectional area of the bone). Reproducibility in routine patient measurements was determined earlier to vary around 0.30% for the radius and tibia with pQCT.22,24
The first pQCT bone measurements were performed at week 5 after accident (t1), the last measurement 40.8±5.9 months after the first measurement (t2). Four subjects who lived in the vicinity of the hospital had repeated measurements between these time points as well (Figure 2). For logistic reasons this was not possible for the other subjects.
Statistical analysis
Two-tailed paired t-tests (P=0.05) were performed on BMD data (absolute values and percentage of initial values) to test for significant differences over the course of the study (average interval between paired BMD, 40.8±5.9 months). Statistical analysis was performed with the SAS statistical package running on a PC. Results were considered significant at P⩽0.05 except where stated otherwise. Data are presented as mean±SD unless otherwise stated. As there was only one female, no division was made according to gender.
To be able to compare the individuals with each other, the bone density for each individual at t2 (40.8±5.9 months) was calculated from the repeated measurements. Furthermore, the slope of the decrease in bone density between t1 and t2 was determined and compared between individuals (Table 1 and Figure 2).
Thus, both visual inspection and statistical analysis were used for the analysis of the data from each single case.25 To estimate the amount of individual change in bone parameter development, results for each individual were calculated as percentage change of initial values. These percentages were compared qualitatively against each other.
Pearson's correlations were used to evaluate the relationships between tibia bone parameter development and age, level of lesion and initial BMD value respectively.
Results
Characteristics of the group are shown in Table 1.
Tibia trabecular bone
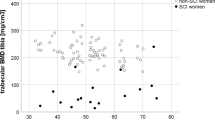
The group of 10 SCI individuals showed a significant decrease of trabecular tibia bone within 40.8 (±5.9) months between first and last measurements following the SCI. This loss is apparent both in absolute values and in percentage of initial value (P=0.002). Mean values±SD at t1 and t2 are summarised in Figure 1.
Marked differences were observed when looking qualitatively at the individual patterns of loss of tibia trabecular bone, both in absolute values and in percentage change from the initial value. The largest loss measured amounted to 83%, the smallest was 7.8% (Table 1). The individual gradients of the trajectory for subjects with more than two time points indicate that in those subjects bone loss persist during the first 3 years after SCI (Figure 2).
All three subjects with multiple measurements show a continuous loss in tibia bone substance during the 3 years of measurement.
Tibia compact bone
A significant decrease in compact bone (P=0.015). resulted between the first and last measurements (Figure 1). Individual patterns showed a large variability of bone mineral changes; a decrease of 40% was observed, however, a small increase of 3% was detected in one individual (Tables 1 and 2; Figure 2). The individual gradients of the trajectory for subjects with more than two time points indicate that in some subjects bone loss continued for more than 3 years (Figure 2).
Radius trabecular bone
There was no change in radius trabecular bone observable during the monitoring period for the whole group. Individual patterns of change vary between 10% loss and 14% increase of this bone parameter.
Radius compact bone
There was no change in radius compact bone observable during the monitoring period. Individual patterns of change vary between 3.5% loss and 4.5% increase of this bone parameter.
Individual volumetric bone densitometry values for trabecular and compact bone (in mg/cm3) are summarised in Table 2. The parameter development in terms of percentage change from initial values (%IV) for the 4 years following the SCI is expressed in Table 1 for the tibia.
Correlations between tibia bone parameter development and age, level of lesion and bone curve coefficient
No significant correlation was found between tibia bone parameter development and age, level of lesion and initial BMD value, respectively.
Discussion
The aim of this study was, firstly, to evaluate the changes in BMD following a SCI of more than 3 years duration using a pQCT scanner and, secondly, to explore individual differences in BMD changes following an SCI. To our knowledge, this is the first study that analyses the trabecular and compact bone parameters of a group of SCI individuals longitudinally for a period of more than 3 years.
Bone mass loss following the SCI may be expected to reduce bone strength. However, there seems to be a contradiction between the assumption that a steady state in bone formation is reached after 2 years following the SCI and the observation that fracture rate in SCI increases up to the third year onward after SCI. Within around 3½ years following an SCI, a significant decrease of tibia trabecular bone and cortical bone was observed. There was no sign of a new steady state in bone formation in the lower extremity after 2 years following the SCI. The loss in trabecular and cortical bone within the first 2 years is in line with previously reported results.9,10 However, the observed changes for the two bone parameters in this study reveal a large intersubject variability. Furthermore, some individuals showed BMD values during 4 years of SCI, which lie well above the initial values of other subjects. This finding infers the assumption that there might be a considerable individual variability in loss of bone substance following a traumatic SCI. Hence, it seems important to study responses in bone substance following an SCI in case study designs, since these designs may better reveal unusual or uncommon responses. In a mixed population of normal individuals and patients with osteopenia or osteoporosis, it has been possible to differentiate between fast and slow bone loser within a few months.26 From the results of this study, it can be hypothesized that there are ‘fast loser’ and ‘slow loser’ individuals in a newly injured SCI population as well. Further research should substantiate this assumption and should determine the factors responsible for these differences in bone parameter development.
The steepness of the loss of BMD does not correlate with the level of lesion, with the age or with the absolute initial BMD value of the subjects. This finding is at variance with previously reported results where moderate correlations between age and bone mineral density for three femoral sites were observed.27 However, because of the large variance in the data for both ambulatory and SCI populations used in this cross-sectional study, it was difficult to discern with any certainty age or duration trends. Some prior cross-sectional studies have not demonstrated bone loss ongoing with chronic immobilization,1,9,10 whereas several other studies suggest the opposite.11,28,29,30 These results underpin the need for more longitudinal data, as in this study, for determination of true changes with time for individuals with a newly acquired SCI.
In our sample, we did not have a sufficient number of paraplegic and tetraplegic patients to statistically compare changes in BMD between these two groups. There was only one subject presenting with tetraplegia and we could, therefore, not expect a decrease of BMD with time after SCI at the radius. Some previous studies showed a fall in BMD of the upper extremity;8,11 others did not observe any long-term changes in the upper extremity bone substance.5,9 A trabecular BMD loss following cervical SCI within 12 months of 28% and a cortical BMD loss of 3% following the SCI was reported for the radius. Subjects with paraplegia showed no loss in the upper extremity bone substance.23 The results of the current study confirm these findings. Nine of the subjects under investigation in our study were paraplegic and did not show a loss in BMD in the upper extremity.
The relatively small sample size can be regarded as one of the limitations of this study. While we feel confident that the population is reasonably representative of the paraplegic SCI population at large, it might be necessary to recruit a broader population sample for more in depth investigation of the contributing factors that might influence bone mineral substance parameters following an SCI. These factors should additionally include gender, bodily conditions and body mass, habitual loading history, spasticity status and activity level.
In conclusion, we have longitudinally followed the changes in BMD in a cohort of patients with acute SCI, demonstrating large differences in change between subjects in the tibia. No changes in the radius were observed. Paired BMD measurements at the radius and tibia, performed on average 40 months apart, were sensitive in reflecting the changes in bone status.
References
Griffiths HJ, Bushueff B, Zimmerman RE . Investigation of the loss of bone mineral in patients with spinal cord injury. Paraplegia 1976; 14: 207–212.
Bergmann P, Heilporn A, Schoutens A, Paternot J, Tricot A . Longitudinal study of calcium and bone metabolism in paraplegic patients. Paraplegia 1977–78; 15: 147–159.
Chantraine A, Nusgens B, Lapiere ChM . Bone remodelling during the development of osteoporosis in paraplegia. Calcif Tiss Int 1986; 38: 323–327.
Elias AN, Gwinup G . Immobilization osteoporosis in paraplegia. J Am Paraplegia Soc 1992; 15: 163–170.
Wilmet E, Ismail AA, Heilporn A, Welraeds D, Bergmann P . Longitudinal study of the bone mineral content and of soft tissue composition after spinal cord section. Paraplegia 1995; 33: 674–677.
Szollar SM, Martin EME, Parthemore JG, Sartoris DJ, Deftos LJ . Demineralization in tetraplegic and paraplegic man over time. Spinal Cord 1997; 35: 223–228.
Uebelhart D, Demiaux-Domenech B, Roth M, Chantraine A . Bone metabolism in spinal cord injured individuals and in others who have prolonged immobilization. A review. Paraplegia 1995; 33: 669–673.
Garland DE et al. Osteoporosis after spinal cord injury. J Orthop Res 1992; 10: 371–378.
Biering-Sørensen F, Bohr HH, Schaadt OP . Longitudinal study of bone mineral content in the lumbar spine, the forearm and the lower extremities after spinal cord injury. Eur J Clin Invest 1990; 20: 330–335.
Biering-Sørensen F, Bohr H, Schaadt O . Bone mineral content of the lumbar spine and lower extremities years after spinal cord lesion. Paraplegia 1988; 26: 293–301.
de Bruin ED, Dietz V, Dambacher MA, Stüssi E . Longitudinal changes in bone in men with spinal cord injury. Clin Rehabil 2000; 14: 145–152.
Finsen V, Indredavik B, Fougner KJ . Bone mineral and hormone status in paraplegics. Paraplegia 1992; 30: 343–347.
Hayes WC, Bouxsein ML . Biomechanics of cortical and trabecular bone: implications for assessment of fracture risk. In: Mow VC, Hayes WC (eds.) Basic Orthopaedic Biomechanics. 2nd edn. Philadelphia, New York: Lippincott-Raven Publishers 1997 pp 71, 72, 83–90.
Comarr AE, Hutchinson RH, Bors E . Extremity fractures of patients with spinal cord injuries. Am J Surg 1962; 103: 732–739.
Eichenholtz SN . Management of long-bone fractures in paraplegic patients. J Bone Joint Surg 1963; 45-A: 299–310.
Ragnarsson KT, Heiner Sell G . Lower extremity fractures after spinal cord injury: a retrospective study. Arch Phys Med Rehabil 1981; 62: 418–423.
Freehafer AA, Mast WA . Lower extremity fractures in patients with spinal-cord injury. J Bone Joint Surg 1965; 47-A: 683–694.
Keating JF, Kerr M, Delargy M . Minimal trauma causing fractures in patients with spinal cord injury. Disabil Rehabil 1992; 14: 108–109.
Frisbie JH . Fractures after myelopathy: the risk quantified. J Spinal Cord Med 1997; 20: 66–69.
Vestergaard P, Krogh K, Rejnmark L, Mosekilde L . Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord 1998; 36: 790–796.
Stytz MR, Frieder O . Three-dimensional medical imaging modalities: an overview. Biomed Eng 1990; 18: 1–25.
Ruegsegger P . The use of peripheral QCT in the evaluation of bone remodelling. Endocrinologist 1994; 4: 167–176.
Frey-Rindova P, de Bruin ED, Stüssi E, Dambacher MA, Dietz V . Bone mineral density in upper and lower extremities during 12 months after spinal cord injury measured by peripheral quantitative computed tomography. Spinal Cord 2000; 38: 26–32.
Dambacher MA, Rüegsegger P . Knochendichtemessungen und ihre Indikationen. Orthopäde 1994; 23: 38–44.
Wagenaar RC et al. The functional recovery of stroke: a comparison between neuro-developmental treatment and the Brunnstrom-method. Scand J Rehab Med 1990; 22: 1–7.
Dambacher MA, Neff M, Kissling R, Qin L . Highly precise peripheral quantitative computed tomography for the evaluation of bone density, loss of bone density and structures. Consequences for prophylaxis and treatment. Drugs Aging 1998; 12 (Suppl 1): 15–24.
Kiratli BJ, Smith AE, Nauenberg T, Kallfelz CF, Perkash I . Bone mineral and geometric changes through the femur with immobilization due to spinal cord injury. J Rehabil Res Dev 2000; 37: 225–233.
Hangartner TN, Rodgers MM, Glaser RM, Barre PS . Tibial bone density loss in spinal cord injured patients: effects of FES exercise. J Rehabil Res Dev 1994; 31: 50–61.
Demirel G, Yilmaz H, Parker N, Onel S . Osteoporosis after spinal cord injury. Spinal Cord 1998; 36: 822–825.
Bauman WA, Spungen AM, Wang J, Pierson RN, Schwartz E . Continuous loss of bone during chronic immobilization: a monozygotic twin study. Osteoporos Int 1999; 10: 123–127.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
de Bruin, E., Vanwanseele, B., Dambacher, M. et al. Long-term changes in the tibia and radius bone mineral density following spinal cord injury. Spinal Cord 43, 96–101 (2005). https://doi.org/10.1038/sj.sc.3101685
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101685
Keywords
This article is cited by
-
Comparison of DXA-based versus CT-based indices to predict prevalent fracture history in men with spinal cord injury
Osteoporosis International (2023)
-
Osteoporosis in the lower extremities in chronic spinal cord injury
Spinal Cord (2020)
-
Bone fragility after spinal cord injury: reductions in stiffness and bone mineral at the distal femur and proximal tibia as a function of time
Osteoporosis International (2018)
-
Bone loss at the distal femur and proximal tibia in persons with spinal cord injury: imaging approaches, risk of fracture, and potential treatment options
Osteoporosis International (2017)
-
Measuring muscle and bone in individuals with neurologic impairment; lessons learned about participant selection and pQCT scan acquisition and analysis
Osteoporosis International (2016)