Abstract
Study design:
Longitudinal, prospective within-subject design.
Objectives:
(1) To determine the effects of long-term body-weight-supported treadmill training (BWSTT) on functional walking ability and perceived quality of life in persons with chronic incomplete spinal cord injury (SCI) and (2) to investigate whether training adaptations are maintained following cessation of the BWSTT programme.
Setting:
Hamilton, Ontario, Canada.
Methods:
A group of 14 individuals with chronic (mean 7.4 years postinjury) incomplete SCI (ASIA B & C) participated in thrice-weekly sessions of BWSTT for a period of approximately 12 months (144 sessions). Functional walking ability and indices of subjective well-being were evaluated during the training programme and over an 8-month follow-up.
Results:
In total, 13 subjects successfully completed the 144 training sessions in the required study period (max. 15 months). Adherence to the thrice-weekly training frequency was 78.8%. All subjects improved in treadmill walking ability (54% reduction in required external body-weight support (BWS), 180% increase in treadmill walking speed, 335% increase in distance walked/session) and six subjects improved their capacity to walk over ground. There were accompanying increases in satisfaction with life and satisfaction with physical function, both of which were significantly correlated with improvements in treadmill walking ability. All but one subject returned for follow-up assessment 8 months post-training; while there was a slight decline in treadmill walking performance, over ground walking scores remained relatively stable. The only change in subjective well-being in the follow-up was a slight decrease in satisfaction with physical function.
Conclusion:
Thrice-weekly BWSTT for 12 months was an effective stimulus to improve treadmill walking ability and indices of subjective well-being in persons with chronic incomplete SCI and most of these improvements were maintained for up to 8 months following the cessation of training.
Similar content being viewed by others
Introduction
There is a growing body of literature supporting the benefits of body-weight-supported treadmill training (BWSTT) as a means of improving functional walking ability in persons with spinal cord injury (SCI). Studies in both the acute1, 2, 3, 4 and chronic3, 5, 6, 7 SCI population have shown that functional walking ability can be improved with BWSTT in patients with motor-incomplete (American Spinal Injury Association Classification (ASIA) C or D) paraplegia or tetraplegia. These results are certainly encouraging, but a number of issues need to be resolved before BWSTT becomes accepted as a standard form of rehabilitation after SCI. These issues include the determination of the optimal training volume, standardization of the assessment of ‘functional ambulation’ and an understanding of the long-term maintenance of any gains in functional ambulation after discontinuation of BWSTT. Equally important, but rarely addressed, is an understanding of the impact of BWSTT on the subjective well-being of persons with SCI, especially in those who do not progress to independent walking and whether the cessation of BWSTT has negative effects on these psychological outcomes.
To date, published studies of BWSTT used a minimum of 3–5 times/week training and training durations tended to be somewhere between 3 and 5 months.1, 2, 4, 5 While higher training frequencies may be easier to implement within the clinical setting during in-patient rehabilitation, for community-dwelling individuals with chronic SCI, a commitment of >3 times/week might not be feasible due to the specific transportation and health barriers unique to this population.8 If BWSTT is to be offered as a rehabilitative option to persons with SCI after discharge from hospital, it will be important to establish whether training frequency or total training volume is the key determinant of success of the intervention.
Since the majority of persons with incomplete SCI identify walking as one of their primary goals,9 one would predict that any improvement in functional ambulation as a result of BWSTT could have substantial impact on aspects of subjective well-being such as quality of life (QOL), psychological well-being and perceptions of handicap. To date, however, no BWSTT study has incorporated any measures of subjective well-being into their outcome measures. Guest et al10 noted a decrease in depression scores following 32 sessions of functional electrical stimulation (FES)-assisted walking, but no follow-up assessments were made. Recent work from our laboratory found that 9 months of twice-weekly exercise training in persons with SCI resulted in improvements in perceived QOL, but these improvements were gone by 3-months post-training.11, 12 Moreover, this post-training decrease in perceived QOL paralleled a decrease in exercise adherence, suggesting that continued exercise adherence is essential for the maintenance of exercise-induced improvements in subjective well-being in persons with SCI. If these results are to be generalized to the literature on BWSTT, it becomes important that we understand the degree to which gains in functional ambulation are maintained once BWSTT ceases.
There are only three published studies which report on the maintenance of improvements in functional ambulation following BWSTT,4, 7, 13 and despite significant differences in subject characteristics, training parameters and assessment of functional ambulation, a general conclusion is that upon cessation of BWSTT, maintenance of walking ability is completely dependent upon continued ambulation practice (either over ground or on the BWS treadmill). Thus, for individuals who do not progress to over ground walking capability and do not have access to a BWS treadmill, it is possible that any gains in functional walking skills (and possibly QOL) made during BWSTT might be lost in the months following training.
The purpose of this study was twofold: (1) to examine the effects of 12 months of thrice-weekly BWSTT on functional walking ability and perceived QOL in persons with chronic SCI (>1 year postinjury) and (2) to determine the maintenance of these adaptations 8 months following cessation of the BWSTT programme.
Methods
Participants
Participants were recruited via contact with medical staff at the Central West Ontario Regional SCI Rehabilitation Program at Chedoke Hospital in Hamilton and through local advertisement. A total of 11 male and three female participants agreed to participate in the study and provided informed written consent. The study was approved by the Research Ethics Board of Hamilton Health Sciences. All participants had sustained a traumatic incomplete SCI a minimum of 12 months prior to entering the study (mean=7.4±6.9 years) and all but two had some motor function, as indicated by an ASIA score of C.14 Exclusion criteria were as follows: cardiac pacemaker, unstable angina or documented heart disease, uncontrolled cardiac dysrhythmia, chronic obstructive lung disease, uncontrolled autonomic dysreflexia, recent nontraumatic fracture, tracheostomy, bilateral hip and knee flexion contractures greater than 20°, drug addiction, age greater than 60 years, or persons greater than 40 years who failed phase 1 of a progressive incremental exercise tolerance test and severe muscle shortening or severe skin ulcerations. Descriptive characteristics of the study sample are presented in Table 1.
Training intervention
All training took place on the Woodway Loco-system (Woodway USA, Inc., Foster, CT, USA) treadmill, which allows for a chosen proportion of the individual's body weight to be supported via an overhead system with weight counterbalance. On each training day, participants were fitted with a specialized harness (which could be secured to overhead pulley cables) prior to being wheeled onto the treadmill for training and a minimum of two therapists assisted the individual through the walking gait during the treadmill sessions.
During the first training session, a level of BWS was chosen for each participant so that they could maintain an upright trunk and their knees did not buckle. If the BWS was set too low, participants tended to sit in the harness, which did not facilitate proper gait. The treadmill training strategy focused on proper weight shifting and weight bearing during the loading phase and on the maintenance of an upright torso. The initial sessions comprised of walking bouts of 5–15 min, according to tolerance. Treadmill speed was chosen based on participant comfort and safety. Most participants began training with 60% body weight support or greater and walked at treadmill speeds of 0.6 km/h or less. Over the course of training, both the %BWS and the treadmill speed were modified on an individual basis to increase the training intensity, following the accepted strategy of first unloading a portion of the BWS, then increasing the speed of the treadmill at each level of BWS.2
The study protocol consisted of three training sessions per week until 144 sessions were completed – approximately 12 months. Participants completed 3 bouts of treadmill walking during each session and the duration of walking during each bout was gradually increased according to participant tolerance. Attendance during the training study was recorded and adherence was defined as the total number of training sessions attended divided by the total number of possible training sessions, in percent. Participants were considered compliers with the intervention if they were able to complete the required 144 sessions in a maximum of 15 months. After 6 months of training, participant 11 was not able to maintain the attendance requirement of three sessions per week and her data will not be included in the results of this study. Of the 13 participants who completed the training study, 12 were able to return for follow-up testing.
Follow-up assessment
Following completion of the BWSTT study, participants were invited to attend once-weekly BWSTT and/or twice-weekly fitness training (arm ergometry and resistance training) within the rehabilitation centre and attendance was recorded. A follow-up assessment was conducted approximately 8 months (37±2.1 weeks) after completion of the BWSTT study. Adherence to the BWSTT and/or fitness training was defined as the total number of sessions attended divided by the number of possible sessions, in percent.
Assessment of functional walking
Functional walking was assessed in two ways: (1) by measuring the walking speed, distance walked and %BWS provided during a typical treadmill session and (2) using a modified version of a scale developed by Wernig et al3, 7 to evaluate over ground walking abilities (see Table 2).
Subjective well-being
Depression
Depressive symptomatology was assessed with the Centre for Epidemiological Studies Depression Scale (CES-D15), which was designed for use in community samples. Respondents indicated how often, over the past week, they experienced each of the 20 symptoms described in the CES-D (eg, ‘I felt sad’). Responses were made on a 4-point scale ranging from 0 (rarely or none of the time) to 3 (most or all of the time) and were then summed. Higher sums indicate greater depressive symptomatology and sums ⩾16 indicate an increased risk of experiencing clinical depression.16 The CES-D has demonstrated a high degree of reliability and validity15 and has been shown to be sensitive to change in studies of people with SCI.16, 17
Life satisfaction
The 5-item Satisfaction With Life Scale (SWLS18) was used to measure ‘overall goodness’ of the participants' lives. Respondents indicated the extent to which they agreed with each item (eg ‘I am satisfied with my life’) using a scale ranging from 1 (strongly disagree) to 7 (strongly agree). Responses were summed with higher scores indicating higher overall life satisfaction. This widely used measure has good psychometric properties19 and has been frequently used in studies of people with SCI.20
Perceived health
A single item from the Medical Outcomes Study Short-Form Health Survey (SF-3621) was used to assess general health perceptions. This item asked participants to rate their general health on a 5-point scale ranging from Excellent to Poor. Responses were reverse scored such that higher scores indicated better perceived health.
Instrumental activities of daily living
There is currently no accepted measure of perceived ability to perform activities of daily living for individuals with SCI. A modified version of the Instrumental Activities of Daily Living (IADL) scale22 was used in the present study. Participants were asked about how much help they need during various ADLs and points were allocated according to the degree of perceived independence. The maximum score is 16 (independence) and the minimum score is 0 (maximum dependence). The IADL was rated as ‘acceptable’ by a large majority in a sample of individuals with SCI (in response to a request for their opinion about completing the scale23).
Study design and data analyses
A longitudinal, prospective within-subject design was used. Changes in functional walking ability were assessed every 36 sessions (∼3 months) during the BWSTT programme and approximately 8 months following its cessation (follow-up assessment). The average walking speed, %BWS and total distance walked per session were determined at each time point. BWSTT and/or fitness training frequency during the follow-up period were compared to BWSTT frequency during the training period.
Measures of subjective well-being were administered in face-to-face interviews by a trained research assistant. Assessments were made every 36 sessions, but one-way, repeated measures ANOVAs were conducted only on the baseline and postintervention measurement points, rather than across all measurement points. This analytical approach was used because the study was insufficiently powered to detect the modest differences that would be expected to occur between 3-month measures. Given that longer exercise interventions produce greater change in subjective well-being,24 it was hypothesized that significant, training-related improvements would most likely be detected at study end. Finally, correlations between changes in subjective well-being and measures of functional walking ability and/or exercise adherence were examined using Pearson's product-moment correlations.
Since not all subjects came back for follow-up testing (see Subject Adherence section), statistical analyses were conducted in two ways: (1) including all subjects who completed the 144 BWSTT training sessions (n=13) and (2) including those subjects who completed both the 144 BWSTT training sessions and the 8-month follow-up (n=10–12).
Results
Subject adherence
Only one of the 14 subjects did not complete the 144 BWSTT sessions in the required time period. The remaining 13 participants had a compliance of 78.8±7.8% (range 66.7–93.4% of possible sessions completed). Of these 13 participants, 12 underwent follow-up testing approximately 8 months post completion of the BWSTT programme (see below).
Training-induced changes in functional walking ability
All subjects improved their treadmill walking ability over the course of the 144 sessions of BWSTT, as evidenced by decreases in the amount of BWS as well as increases in the speed and distance walked per treadmill session (see Figure 1). The thrice-weekly training resulted in a decrease in the required %BWS (from 73.1±10.3% at baseline to 19.5±12.2% at study end; P<0.01), an increase in treadmill walking speed (0.5±0.3 km/h at baseline to 1.4±0.8 km/h at study end; P<0.01) and increased distance walked per treadmill training session (221.4±186.8 m at baseline to 961.7±463.8 m at study end; P<0.01). Changes in treadmill walking speed and distance walked per session are presented in Figure 2.
At baseline, only three of the 14 subjects had scores greater than zero on the modified version of the Wernig walking scale. Following training, there were six subjects with scores greater than zero, with one subject being able to walk >5 steps independently, without any assistive devices. These results are depicted in Table 3.
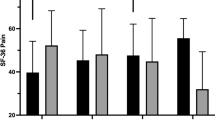
Training-induced changes in subjective well-being
Table 4 presents descriptive statistics for each measure of subjective well-being. There were significant improvements in life satisfaction (P=0.05) and satisfaction with physical function (P=0.03) following BWSTT, but no significant change in depression, perceived health or perceived ability to perform IADL. The percentage of change in life satisfaction was significantly correlated with %change in body weight support (r=−0.59, P=0.02) and percent change in satisfaction with physical function was positively correlated with %change in distance walked (r=0.51, P=0.04). No other correlations were significant.
Follow-up assessment
In contrast to the relatively high compliance with the thrice-weekly training programme, adherence to the available once-weekly BWSTT sessions during the follow-up period was only 31.7±26. 8% (range 0.0–82.9%). The adherence to combined once-weekly BWSTT and twice-weekly fitness training was even lower, at 22.5±26.5% (range 0.0–71.4%).
The required %BWS for treadmill training increased from the post-training assessment to the 8-month follow-up (from 19.5±12.2 to 34.9±14.4; P<0.01), but remained below pretraining values (73.1±10.3; P<0.01; Figure 1). The individual changes in %BWS were not correlated to BWSTT adherence during the follow-up period. There were no changes in preferred walking speed on the treadmill between the 12-month and follow-up assessments (1.4±0.8 km/h at both). Overall, there were no changes in mean over ground walking score from 12 months to follow-up (see Table 3).
Turning to the measures of subjective well-being (see Table 4), there was a significant decrease in satisfaction with physical function (P=0.03) that was unrelated to changes in %BWS or treadmill speed. None of the other indices of subjective well-being changed significantly during the follow-up period.
Analyses were undertaken to see if percent changes in subjective well-being between 12 months and follow-up assessments were related to exercise adherence. Exercise adherence (BWSTT alone or combined with fitness training) during the follow-up period had significant positive correlations with %change in perceived ability to perform ADL (r=0.75 (see Figure 3) or r=0.70, respectively).
Correlation between BWSTT adherence during the follow-up period (% of possible sessions attended) and %change in perceived ability to perform ADL from 12 months to follow-up. IADL: Instrumental Activities of Daily Living22
Discussion
In light of the current interest in BWSTT as an intervention to improve functional walking in people with incomplete SCI, this study was undertaken to examine the effects of 12 months of thrice-weekly BWSTT on both functional walking ability and subjective well-being in persons with chronic incomplete SCI. To our knowledge, this is the longest duration prospective study of BWSTT conducted to date in the SCI population. The participants all had chronic injuries (mean=7.4 years postinjury) and all were wheelchair-dependent at the outset of the study. Of the 14 subjects who started the training, 11 had no standing or walking capability at all, even with the help of therapists. This makes our subjects a little less functional in comparison to several previous BWSTT studies of persons with incomplete SCI in which the vast majority of participants had some walking ability.1, 4, 5, 7, 13 Despite the poorer baseline walking abilities of our participations, all of them improved in treadmill walking performance following the ∼12-month of training, as indicated by decreases in %BWS and increases in treadmill speed and distance walked per session. Of interest, the changes in treadmill walking performance of the two ASIA B subjects were almost identical to the mean changes seen by the entire study sample. At the end of the training, four participants could walk on the treadmill with no BWS at all and the number of subjects with modified Wernig walking scores greater than zero increased from 3 (pre-training) to 6. In conjunction with these positive changes in ambulatory capacity, we saw improvements in life satisfaction and satisfaction with physical functioning following the training period, as well as some indication of possible relationships between changes in ambulatory capacity and changes in subjective well-being. Again, the two subjects with motor-complete SCI (ASIA B) were within one standard deviation of the group means.
Given the fact that BWSTT is a costly and labour-intensive therapy and that access to BWS treadmills is limited at best, a secondary purpose of this study was to determine the maintenance of any improvements in either functional walking ability or subjective well-being in the 8-month period following cessation of BWSTT. This was considered to be especially relevant in this study since more than half of our participants did not become independent walkers (even with assistance) following the training. To our knowledge, only three prior studies have investigated the maintenance of any gains in locomotor ability following BWSTT. From this limited source of data, it would appear that if BWSTT is successful in resulting in independent locomotor ability (with or without assistive devices), any gains that were achieved over the course of training are maintained for up to 6 years later.4, 7, 13 Persons who do not progress to independent or fully unloaded walking, however, tend to lose the gains achieved over the course of training in the months following.
In the present study, all participants were given the opportunity to continue with BWSTT at a frequency of once per week following completion of the training programme, although adherence to this training option was very low. At the follow-up assessment, we found that while there appeared to be a slight decrease in locomotor ability (as seen by an increase in mean %BWS), there was no significant change in over ground walking scores in those subjects who had become independent walkers. The fact that one subject's walking score dropped from 9 to an 8 was due to the subject preferring to use a cane for the follow-up walk (which allowed him to walk much further). To interpret these data we need to consider two things: first, why was adherence to BWSTT so much lower in the follow-up period compared to the training programme? Second, is BWSTT still considered to be successful if independent walking is not achieved?
The difference in exercise adherence between the 12-month BWSTT study and the follow-up period was quite striking; adherence to the available training sessions dropped by more than half during follow-up compared with the training programme. We believe that there are several possible reasons for this decline in adherence. First, once the 12-month study period was over, the parking/transportation costs of participants coming to our rehabilitation centre were no longer reimbursed. This could have created enough of a financial barrier to significantly limit attendance. Second, several of our subjects had put school and/or career on hold while in the study but resumed these activities afterward. This meant that they had less time available to devote to their training and scheduling conflicts often limited their ability to attend training sessions. A final consideration related specifically to those individuals who progressed to over ground walking; they may have no longer felt the need to do BWSTT and could practice walking on their own. Nevertheless, despite suboptimal adherence levels, it is important to note that the training-induced gains in both locomotor ability and overall life satisfaction were generally maintained at follow-up. These findings highlight the potentially enduring effects of BWSTT.
Traditionally, BWSTT success has been evaluated purely on the basis of how much improvement occurs in locomotor ability. While this is obviously of considerable importance (to both the patients and the therapists), the benefits of BWSTT may extend far beyond the ability to ambulate. In addition to the findings reported here, we have previously found significant changes in muscle morphology (fibre type distribution), increased muscle fibre areas, improved blood lipid profile and increased glucose tolerance in subjects after only 6 months of thrice-weekly BWSTT.25, 26 Taken together, these adaptations would be predicted to decrease the risk of acquiring Type II diabetes and/or cardiovascular disease. We also have evidence that BWSTT has positive effects on the cardiovascular system, as we have noted improvements in the autonomic regulation of heart rate variability and increased lower leg blood flow.27 The positive changes in the muscular and cardiovascular systems occurred in all of our subjects (including the two with ASIA B), regardless of whether independent walking was achieved. These benefits certainly should not be ignored, especially since Type II diabetes and cardiovascular disease are prevalent secondary complications in the SCI population.28, 29, 30
In addition to the physiological benefits of BWSTT, this type of therapy carries with it a significant potential to improve subjective well-being. In the present study, significant increases emerged in overall life satisfaction as well as satisfaction with physical function. Although we did not find significant improvements in depression or ability to perform ADL, we suspect that these null findings were due to floor and ceiling effects, respectively. Specifically, at baseline, none of our participants had elevated scores on the CES-D (ie ⩾16) and 75% of our sample had IADL scores ⩾13 out of 16. With little room for improvement, it would be improbable to show significant improvements on these variables.
It was interesting to note that the changes in satisfaction with life and physical function were only weakly correlated with the extent to which subjects improved their walking ability. This observation is consistent with most exercise studies, which typically show no relationship between subjective and objective indices of well-being among people with disease or disability.31 Apparently, subjects' own perceptions of their improvements – whether big or small – have a far greater impact on subjective well-being than experimenter-measured improvements.24 Our finding that subjects considered their lives to be better regardless of whether they improved their over ground walking highlights the value of small functional improvements to an individual with SCI. Improvements that may not be considered scientifically or statistically significant can still have a tremendous impact on the perceived QOL for a person with a SCI.7, 32
Notwithstanding the positive results presented here, it is important to acknowledge an important limitation of this study. A randomized controlled design was not employed due to the relatively small number of subjects recruited and the high potential for drop-out among subjects who were randomized to a control group. We were also concerned about the ethical implications of a randomized design; in one of our previous exercise trials, people with an SCI were more likely to become clinically depressed after random assignment to a control group.8 While this might present the possibility that the changes we observed were not due to the training intervention at all, we consider the likelihood of this to be extremely remote since our participants were on average more than 7 years postinjury and would not be expected to experience spontaneous improvements in walking ability. It might also be argued that the observed improvements in satisfaction with life and physical function were not due to the training intervention either. However, in a control group of participants in a previous SCI exercise training study, these dimensions of subjective well-being either worsened or did not change.8, 12 Thus, we consider it unlikely that subjective well-being improved spontaneously in the present investigation.
In conclusion, despite the fact that some individuals did not improve their ability to ambulate over ground, 12 months of thrice-weekly BWSTT effectively improved treadmill walking ability and indices of subjective well-being in our cohort of persons with chronic incomplete SCI. Further, we have shown that the improvements in treadmill walking ability and subjective well-being were, for the most part, maintained for at least 8 months following completion of the training intervention, even with very limited access to BWSTT in this follow-up period. This study represents the longest prospective trial of BWSTT in an outpatient population and the high adherence to the thrice-weekly training frequency certainly highlights its appeal as an intervention. Traditionally, BWSTT has been advocated only for those individuals who have residual motor function in their lower legs (ASIA C classification), as these persons have the greatest potential to become independent ambulators. However, our study contributes to the accumulating evidence that BWSTT has benefits that extend beyond improvements in functional walking ability, suggesting that a greater segment of the SCI population could potentially profit from this novel intervention.
References
Behrman AL, Harkema SJ . Locomotor training after human spinal cord injury: a series of case studies. Phys Ther 2000; 80: 688–700.
Nymark J et al. Body weight support treadmill gait training in the subacute recovery phase of incomplete spinal cord injury. J Neuro Rehab 1994; 12: 119–138.
Wernig A, Muller S, Nanassy A, Cagol E . Laufband therapy based on ‘rules of spinal locomotion’ is effective in spinal cord injured persons. Eur J Neurosci 1995; 7: 823–829.
Wirz M, Colombo G, Dietz V . Long term effects of locomotor training in spinal humans. J Neurol Neurosurg Psychiatry 2001; 71: 93–96.
Protas EJ et al. Supported treadmill ambulation training after spinal cord injury: a pilot study. Arch Phys Med Rehabil 2001; 82: 825–831.
Visintin M, Barbeau H . The effects of body weight support on the locomotor pattern of spastic paretic patients. Can J Neurol Sci 1989; 16: 315–325.
Wernig A, Nanassy A, Muller S . Maintenance of locomotor abilities following Laufband (treadmill) therapy in para- and tetraplegic persons: follow-up studies. Spinal Cord 1998; 36: 744–749.
Martin KA et al. Sustaining exercise motivation and participation among people with spinal cord injury: lessons learned from a 9-month intervention. Palaestra 2002; 18: 38–40.
Davies H . Hope as a coping strategy for the spinal cord injured individual. Axone 1993; 15: 40–46.
Guest RS, Klose KJ, Needham-Shropshire BM, Jacobs PL . Evaluation of a training program for persons with SCI paraplegia using the Parastep 1 ambulation system: part 4. Effect on physical self-concept and depression. Arch Phys Med Rehabil 1997; 78: 804–807.
Ditor DS, Latimer AE, Martin Ginis KA, Arbour KP, McCarntey N, Hicks AL . Maintenance of exercise participation in individuals with spinal cord injury: effects on quality of life, stress and pain. Spinal Cord 2003; 41: 446–450.
Hicks AL et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003; 41: 34–43.
Field-Fote EC . Combined use of body weight support, functional electric stimulation and treadmill training to improve walking ability in individuals with chronic incomplete spinal cord injury. Arch Phys Med Rehabil 2001; 82: 818–824.
Ditunno Jr JF, Young W, Donovan WH, Creasey G . The international standards booklet for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Paraplegia 1994; 32: 70–80.
Radloff LS . The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measure 1977; 1: 385–401.
Fuhrer MJ, Rintala DH, Hart KA, Clearman R, Young ME . Depressive symptomatology in persons with spinal cord injury who reside in the community. Arch Phys Med Rehabil 1993; 74: 255–260.
Schulz R, Decker S . Long-term adjustment to physical disability: the role of social support, perceived control and self-blame. J Pers Soc Psychol 1985; 48: 1162–1172.
Diener E, Emmons RA, Larsen RJ, Griffin S . The satisfaction with life scale. J Pers Assess 1985; 49: 71–75.
Pavot W, Diener E . Review of the satisfaction with life scale. Psychol Assess 1993; 5: 164–172.
Dijkers MP . Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 867–876.
Ware Jr JE, Sherbourne CD . The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473–483.
Lawton MP, Moss M, Fulcomer M, Kleban MH . A research and service oriented multilevel assessment instrument. J Gerontol 1982; 37: 91–99.
Andresen EM, Fouts BS, Romeis JC, Brownson CA . Performance of health-related quality-of-life instruments in a spinal cord injured population. Arch Phys Med Rehabil 1999; 80: 877–884.
Lox CL, Martin KA, Petruzello SJ . The Psychology of Exercise: Integrating Theory and Practice. Holcomb Hathaway, Publishers, Inc.: Scottsdale 2003.
Phillips SM et al. Body weight support treadmill training improves blood glucose regulation in persons with incomplete spinal cord injury. J Appl Physiol 2004; 97: 716–724.
Stewart BG et al. Body weight supported treadmill training-induced changes in muscle phenotype, blood lipids and ambulatory capacity in individuals with incomplete spinal cord injury. Muscle Nerve 2004; 30: 61–68.
Ditor DS, Kamath MV, MacDonald MJ, Bugaresti J, McCartney N, Hicks AL . The effects of body-weight supported treadmill training on heart rate variability and blood pressure variability in individuals with SCI. J Appl Physiol 2005; in press.
Bauman WA, Adkins RH, Spungen AM, Waters RL . The effect of residual neurological deficit on oral glucose tolerance in persons with chronic spinal cord injury. Spinal Cord 1999; 37: 765–771.
DeVivo MJ, Krause JS, Lammertse DP . Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1411–1419.
Karlsson AK . Insulin resistance and sympathetic function in high spinal cord injury. Spinal Cord 1999; 37: 494–500.
Lichtenberger CM, Martin Ginis KA, MacKenzie CL, McCartney N . Body image and depressive symptoms as correlates of self-reported versus clinician-reported physiologic function. J Cardiopulmon Rehabil 2003; 23: 53–59.
Martin Ginis KA, Hicks AL . Exercise research issues in the spinal cord injured population. Exer Sport Sci Rev 2005; 33: 49–53.
Acknowledgements
We gratefully acknowledge the support of the Ontario Neurotrauma Foundation (ONF) for providing both the operating funds for this study and studentships for M Adams and L Giangregorio. We also express sincere thanks to all of the volunteer trainers and the study participants for their dedication to this research.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hicks, A., Adams, M., Martin Ginis, K. et al. Long-term body-weight-supported treadmill training and subsequent follow-up in persons with chronic SCI: effects on functional walking ability and measures of subjective well-being. Spinal Cord 43, 291–298 (2005). https://doi.org/10.1038/sj.sc.3101710
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101710
Keywords
This article is cited by
-
The effects of active upper-limb versus passive lower-limb exercise on quality of life among individuals with motor-complete spinal cord injury
Spinal Cord (2022)
-
Body weight-supported gait training for patients with spinal cord injury: a network meta-analysis of randomised controlled trials
Scientific Reports (2022)
-
The Effects of Physical Exercise on Depression for Individuals with Spinal Cord Injury: a Systematic Review
Current Physical Medicine and Rehabilitation Reports (2022)
-
Quality of life and psychological outcomes of body-weight supported locomotor training in spinal cord injured persons with long-standing incomplete lesions
Spinal Cord (2020)
-
Functional magnetic resonance imaging (fMRI) of the sensorimotor cortex in spinal cord injury patient after intensive rehabilitation
Research on Biomedical Engineering (2020)