Abstract
Study design:
Case report.
Objective:
To report a rare lesion of intramedullary cervical tuberculoma.
Setting:
Department of Neurosurgery, Southwest Hospital, Third Military Medical University, Chongqing, The People's Republic of China.
Case report:
A 15-year-old boy presented with pain in the neck and shoulder. Examination showed mild left hemiplegia and pinprink hyperalgesia on the left side up to C3 level. Chest X-ray and CT scan showed patch and dot lesions indicating old tuberculous lesions and MRI showed a ring-enhancing intramedullary lesion at C3/4 level. Tuberculoma resection and antituberculous therapy was given. There was satisfactory recovery clinically.
Conclusion:
Intramedullary cervical tuberculoma is a rare, coexisting systemic tuberculosis and MRI scan helps in obtaining a correct diagnosis; combining surgery with anti-tuberculosis therapy is the treatment of choice.
Similar content being viewed by others
Introduction
Although tuberculosis can be treated, it is still an important health problem in developing countries including China. In recent years, it has also proved to be a common opportunistic infection in individuals of developed countries who test positive for human immunodeficiency virus (HIV). Tuberculosis of the central nervous system (CNS) is rare, with an incidence of only 0.5–2% of patients with systemic tuberculosis.1 Tuberculoma of the CNS is unusual, whereas intramedullary tuberculomas are rare.1, 2, 3, 4, 5 We report a case of intramedullary cervical tuberculoma that was cured by a combination of operation and antituberculous chemotherapy.
Case history
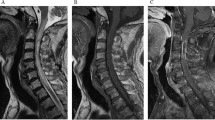
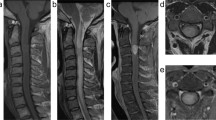
A 15-year-old male presented with onset of radicular pain of neck–shoulder for 1 year. The boy complained of weakness of the left arm and left leg for 4 months. On examination, he had weakness in the left arm and left leg of MRC Grade 4, pinprink hyperalgesia on the left side up to C3 level, increased tendon reflexes in the left arm and the left leg, and his left plantar response was extensor. Temperature sensation was normal. His lumbar puncture revealed pressure of 150 mmH2O, white blood cell count for cerebrospinal fluid (CSF) of 0.002 × 109/l, protein content of 0.81 g/l, sugar content of 4.5 mmol/l, chloride content of 130.9 mmol/l, and erythrocyte sedimentation rate of 40 mm/h. Anti-acid staining and the polymerase chain reaction (PCR) of Mycobacterium tuberculosis DNA for CSF were negative. His chest X-ray and CT scan revealed patch and dot lesions indicating old tuberculosis lesions (Figure 1). The purified protein derivative (PPT) test revealed no abnormality. MRI scan of the cervical spine on T2WI revealed an isointense to hypointense signal at C3/4 level and edema signal surrounding the lesion from medulla oblongata to T3 segment, MRI scan on T1WI revealed an isointense signal at C3/4 level and ring-enhancing intramedullary lesion involving the whole circumference of the cervical spinal cord after gadolinium-diethylenetriaminepentaacetic acid (Gd-DTPA) administration (Figure 2). The diagnosis of intramedullary glioma or ependymoma was made by the radiologist. Tuberculoma was suspected, so preoperative anti-tuberculous therapy and injectable dexamethasone was given.
He underwent C3–C4 laminectomy. The dura mater and arachnoid membrane were normal. The lesion was causing segmental enlargement of the cord and replacing the cord circumferentially. It was firm in consistency, peripherally vascular, yellowish and cheesy in the centre. The lesion was excised totally. Postoperatively, the boy was put on injection streptomycin 0.75 g daily for 1 month intramuscularly, isoniazid 300 mg orally, and rifampicin 450 mg orally for another 12 months. He was continued on steroids. Histopathological examination of the lesion confirmed typical tubercular granuloma (Figure 3). There was temporary weakness in the left arm and left leg of MRC Grade 3 postoperatively. At discharge, at the end of 2 weeks, he had recovered his strength to the preoperative state and postoperative MRI revealed resolution of tuberculoma (Figure 4). He continued making steady improvement in his neurological status. At 8-months follow-up there was full neurological recovery and he went back to school.
Discussion
China has 1.4 million new cases of tuberculosis every year.6 Intramedullary spinal cord tuberculoma is a rare entity. Jenning3 found only one intramedullary tuberculoma among 5344 patients with pulmonary tuberculosis.
Tuberculomas develop following haematogenous dissemination of bacilli from an infection elsewhere in the body, usually lung. There is a slight male preponderance for intramedullary spinal cord tuberculoma (M:F, 1.5:1). Duration of symptoms at presentation varies from 3 to 20 months (mean 11.5 months).5 The present case had evidence of systemic tuberculosis. Although the diagnosis of tuberculoma is usually made based on pathology, systemic examination combined with radiological imaging may arrive at a better preoperative understanding of the diagnosis. Sharma et al5 reported associated tuberculosis elsewhere in the body in four out of 10 patients which is the largest series of intramedullary tuberculoma by now.
Because MRI has been employed widely, early discovery for this kind of lesion may be possible, though the MRI picture varies with the stage of the tuberculoma formation. In the early phase of intramedullary tuberculoma, there is a great inflammatory reaction with an abundance of giant cells and a poor collagenous capsule with variable surrounding edema. At this stage, the tuberculomas seem to be isointense on both T1Wl and T2Wl and enhancing homogeneously on contrast. Later, the capsule becomes richer in collagen, resulting in ring enhancement.1, 7 Pathological changes include non-caseating granuloma, cascating granuloma with a solid centre and caseating granuloma with liquid centre.7 MRI describes three types of tuberculoma pictures: tuberculous lesion appears isointense on T1WI with cord expansion, and isointense to hypointense on T2WI, and ring enhancement with hypointense centre on Gd-DTPA MR scan. The present case was at about this stage. With the development of caseation, the centre becomes bright and gives an appearance of ‘target sign’.7, 8 The ‘target sign’ was thought to be a characteristic sign on the radiological image.5 Sharma et al5 reported all their lesions showed marked enhancement on gadolinium injection and central hypointensity with peripheral ring enhancement was seen in five out of eight cases. Hanci et al9 reported a case of intramedullary spinal cord tuberculous abscess, which showed a well-circumscribed, cystic-appearing intramedullary mass with ring enhancement on MRI; T2WI showed peripheral hypointensity and central hyperintensity.
Spinal tuberculosis infection more commonly presents with tuberculous spondylitis or arachnoiditis.10 Gupta et al11 presented eight cases of intramedullary tuberculoma, but only one of these cases was confirmed by open biopsy sampling and pathological examination. Ratliff10 reported an intramedullary tuberculoma with an inferior area of syringomyelia, with no clearly demarcated lesion on MRI. This is in contrast to the well-circumscribed, firm masses described by Rhoton et al12 and Kayaoglu et al.13 Sharma et al5 reported a tuberculoma similar in appearance to intramedullary spinal cord tumour on MRI, so appearance of intramedullary spinal tuberculosis on MRI varies. Although clinical symptoms and presentation of intramedullary spinal tuberculoma are usually indistinguishable from other spinal cord lesions and the intramedullary spinal tuberculoma is a rare entity, it must be considered in the differential diagnosis of spinal cord compression especially for patients with a history of systemic tuberculosis. The MRI features of tuberculomas are distinct from other intramedullary lesions and are reliable enough to start antituberculous therapy.8 Some of these lesions may resolve completely with antituberculous therapy only,14 but may expand during chemotherapy.15 Preoperative antituberculous therapy for 1–2 weeks may avoid spreading of intraoperative tuberculosis. Careful dissection and resection could get good recovery for intramedullary tuberculoma with mass effect and paradoxical enlargement of the tuberculoma at its late stage.15, 16 Postoperative whole-course antituberculous chemotherapy is mandatory.
References
Torii H, Takahashi T, Shimizu H, Watanabe M, Tominaga T . Intramedullary spinal tuberculoma (Case report). Neurol Med Chir (Tokyo) 2004; 44: 266–268.
Koyama T, Nishimura I, Ozaki F . Intramedullary granuloma – a case report. Spine Spinal Cord 1990; 3: 85–88.
Jenning FL . Tuberculoma of the spinal cord. Ann Intern Med 1934; 7: 1240–1243.
Miyamoto J, Sasajima H, Owada K, Odake G, Mineura K . Spinal intramedullary tuberculoma requiring surgical treatment – case report. Neurol Med Chir (Tokyo) 2003; 43: 567–571.
Sharma MC, Arora R, Deol PS, Mahapatra AK, Sinha AK, Sarkar C . Intramedullary tuberculoma of the spinal cord: a series of 10 cases. Clin Neurol Neurosurg 2002; 104: 279–284.
China Tuberculosis Control Collaboration. The effect of tuberculosis control in China. Lancet 2004; 364: 417–422.
Jinkins JR, Gupta R, Chung KH, Rodriguez-Cebojal J . MR imaging of central nervous system tuberculosis. Radiol Clin North Am 1995; 33: 771–786.
Parmar H, Shah J, Patkar D, Varma R . Intramedullary tuberculomas. MR findings in seven patients. Acta Radiol 2000; 41: 572–577.
Hanci M, Sarioglu AC, Uzan M, Islak C, Kaynar MY, Oz B . Intramedullary tuberculous abscess. Spine 1996; 21: 766–769.
Ratliff JK, Connolly ES . Intramedullary tuberculoma of the spinal cord: case report and review of the literature. J Neurosurg (Spine) 1999; 90: 125–128.
Gupta RK, Gupta S, Kumar S, Kohli A, Mishra UK, Gujral RB . MRI in intraspinal tuberculosis. Neuroradiology 1994; 36: 39–43.
Rhoton EL, Ballinger Jr WE, Quisling R, Sypert GW . Intramedullary spinal tuberculoma. Neurosurgery 1988; 22: 733–736.
Kayaoglu CR, Tuzun Y, Boga Z, Erdogan F, Gorguner M, Aydin IH . Intramedullary spinal tuberculoma. A case report. Spine 2000; 25: 2265–2268.
Thacker MM, Puri AI . Concurrent intramedullary and intracranial tuberculomas. J Postgrad Med 2004; 50: 107–109.
Nomura S, Akimura T, Kitahara T, Nogami K, Suzuki M . Surgery for expansion of spinal tuberculoma during antituberculous chemotherapy: A case report. Pediatr Neurosurg 2001; 35: 153–157.
Citow JS, Ammirati M . Intramedullary tuberculoma of the spinal cord: Case report. Neurosurgery 1994; 35: 327–330.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lin, J., Feng, H., Ai, S. et al. Intramedullary cervical tuberculoma. Spinal Cord 44, 809–812 (2006). https://doi.org/10.1038/sj.sc.3101896
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101896
Keywords
This article is cited by
-
Intra-medullary tuberculoma of the spinal cord presenting with typhoid and paraplegia: a case report
Journal of Medical Case Reports (2012)