Abstract
Study design:
Descriptive study.
Objective:
To examine the individual heart rate–oxygen uptake (HR–VO2) relationship during exercise in persons with tetraplegia (TP).
Setting:
Rehabilitation Centre Heliomare, Wijk aan Zee, The Netherlands.
Methods:
The HR–VO2 relationship was determined in untrained subjects with motor complete TP (C5 or C6, n=10 and C7 or C8, n=10) during a discontinuous graded exercise hand cycle test. The mean HR and VO2 of the final 60 s of 2-min exercise blocks were used for calculation of the individual correlation coefficient and the standard error of the estimate (SEE).
Results:
Two subjects of the C5–C6 group were not able to complete the test. Individual Pearson's correlation coefficients (r) ranged from 0.68 to 0.97 and SEE from 2.6 to 22.4% VO2-Reserve (VO2R). The mean Pearson's r and SEE were 0.81±0.12 and 10.6±5.6% VO2R in the C5–C6 group and 0.91±0.07 and 7.0±3.2% VO2R in the C7–C8 group, respectively. Two subjects of the C5–C6 group and six subjects of the C7–C8 group attained a linear HR–VO2 relationship with an acceptable SEE (⩽6.0%) and r (>0.90).
Conclusions:
The HR–VO2 relationship appeared linear in only eight out of 18 subjects. An individual analysis of the HR–VO2 relationship is necessary to determine whether HR can be used to quantify exercise intensity. The use of HR to prescribe training intensity should be reconsidered in persons with TP.
Sponsorship:
This study is supported from a grant by ZON-MW.
Similar content being viewed by others
Introduction
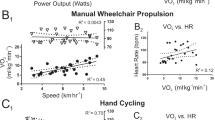
In able-bodied persons, heart rate (HR) and oxygen uptake (VO2) are linearly related and therefore exercise training intensity can be prescribed, based on HR. This is an advantage because the measurement of VO2 during training is complicated, whereas HR can be easily recorded. In persons with a spinal cord injury (SCI), HR has also been used to prescribe training intensity,1 as well as to indicate physical strain in daily activities.2, 3, 4 The guidelines of the American College of Sports Medicine (ACSM) for training of able-bodied persons – 50–85% heart rate reserve (HRR)5 – have also been applied in training studies with persons with paraplegia (PP)6 as well as tetraplegia (TP).7, 8 These guidelines may be valid for persons with PP, as several studies9, 10, 11, 12, 13, 14 showed a strong individual linear HR–VO2 relationship in persons with PP. In individuals with TP however, this may be different as a result of the disturbed sympathetic innervation, which may affect the HR–VO2 relationship.
The sympathetic innervation of the heart derives from Th1 to Th4 and therefore spinal cord lesions at or above Th4 may lead to inappropriate cardioacceleration.15 The increase in HR during exercise in these persons is mostly due to withdrawal of vagal parasympathetic stimulation.16 As a consequence, maximal HR in individuals with TP is often restricted to about 130 beats per minute (b.p.m.).1 Moreover, normal cardiovascular responses to exercise (eg vasoconstriction in relatively inactive tissues and increased blood flow to active muscle) are diminished as a consequence of the disturbed sympathetic nervous system.15 In a study of Hjeltnes et al17 in persons with TP, it was indeed shown that, compared to able-bodied, mean blood pressure (BP) and oxygen tension (PO2) in arterial blood were reduced during graded exercise. Furthermore, as a consequence of the disturbed sympathetic innervation, autonomic dysreflexia (AD) may occur in subjects with a lesion level at or above Th6.18 AD may result in an uncontrolled elevation of BP, and during exercise, this may lead to sudden changes in HR and eventually a higher HRpeak and VO2peak.19
Apart from the disturbed sympathetic innervation, persons with TP have a low physical capacity as a consequence of the low active muscle mass and inactivity of the venous muscle pump. Because of the disturbed sympathetic innervation and the low physical capacity, it is questionable whether HR can be used for monitoring exercise intensity in persons with a high-level PP or TP.
When looking more closely at studies investigating the HR–VO2 relationship in persons with PP, hardly any subjects with a complete Th1–Th4 lesion – with possibly disturbed sympathetic innervation of the heart – were included.9, 10, 12, 14 Moreover, only a few studies have focused on the HR–VO2 relationship in persons with TP13, 20, 21 and only one focused on the individual relationship.20 The available studies all use hand rim wheelchair or arm crank exercise to investigate the HR–VO2 relationship.
In the last decade, hand cycling (Figure 1) has become a very popular alternative for daily outdoor wheelchair use in the Netherlands, also among persons with TP. These systems were found to be more efficient and less straining than hand rim wheelchair propulsion22, 23 and can be used also in early rehabilitation and in fragile individuals. Moreover, it seems possible to attain significantly higher peak VO2, power output (PO) and HR-values in hand cycling compared to wheelchair propulsion.22 Therefore, hand cycling seems to be very appropriate for training and testing of persons with TP.
The aim of this study is to examine the individual HR–VO2 relationship in individuals with TP to answer the question: Can HR be used to quantify exercise intensity in persons with TP during hand cycling?
Methods
Subjects
Twenty subjects (with TP), aged between 21 and 64 years participated in this study. Ten subjects were classified as having a high-level cervical lesion (C5 or C6) and 10 were classified as having a low-level cervical lesion (C7 or C8) (Table 1). All subjects had motor complete lesions, classified on the American Spinal Injury Association (ASIA) impairment scale24 as A or B. Seven subjects of the high lesion group and one subject of the low lesion group used an electric-powered wheelchair. The other subjects all used manual wheelchairs. All participants were considered to be untrained to moderately trained (no more than 2 h of sport participation weekly during the last 3 months). Four subjects were not experienced in hand cycling at all (Table 1). Before testing, all participants were medically screened by a physician. Exclusion criteria were: Serious overuse injuries of the upper extremities or other impairments, which do not allow performing physical activity (pressure sores), bladder infection and other medical conditions, use of β-blockers and cardiovascular diseases. The subjects were closely monitored on symptoms of AD before and during the execution of the test. Symptoms of AD18, 25 are extreme hypertension, abnormal high or low HR. Above lesion level: pounding headache, initially pallor, flushed skin, excessive sweating, nasal stuffiness and anxiety. Below lesion level: pallor, goose bumps and cold skin. If any of the symptoms would occur, the test was terminated and not included in the analysis. Approval was obtained from the Medical Ethics Committee of the VU University Medical Center in Amsterdam and all subjects signed an informed consent form. Subject 7, 15 and 16 were in the final stage of the clinical rehabilitation and the other subjects were measured after rehabilitation.
Design and protocol
To determine the individual relationship between HR and VO2, subjects with TP performed a standardised discontinuous graded exercise hand cycle test on a motor-driven treadmill. The medical examination before the test included ASIA scoring, BP measurement and medication use. Before subjects started the test, they were asked to empty their bladder to prevent the occurrence of symptoms of AD. Oxygen uptake (VO2, l/min), carbon dioxide output (VCO2, l/min) and ventilation (Ve, l/min) were continuously measured using a computerised breath-by-breath gas analysing system (Oxycon Delta, Viasys, Bilthoven, The Netherlands). HR (b.p.m.) was recorded with a HR monitor (Polar Sport tester, Polar Electro Inc., Kempele, Finland). Before the graded exercise hand cycle test, resting values for metabolic and HR parameters were measured during 5 min of sitting rest. Subsequently, the subjects familiarised with hand cycling on the treadmill during 2 min. In these minutes, the velocity of the treadmill and cadence of the hand cycle were adjusted to the ability of the subject within the range of 4–7 km/h and a cadence of approximately 60 r.p.m. After a 3 min rest following the familiarisation period, the subjects performed the discontinuous graded exercise test. Exercise bouts of 2 min were followed by 30 s of rest. In each exercise step, PO was increased with increments of 2.00–5.25 W, depending on the estimated individual capacity. This process continued until exhaustion or until the subject indicated that he/she wanted to stop. Average HR and VO2-values over the last 60 s of each exercise bout were used for analysis. If the last uncompleted block exceeded more than 60 s, the HR and VO2-value were included as well. The highest VO2-value attained over 60 s during the test was defined as the VO2peak. Respiratory exchange ratio (RER) was calculated as the ratio between VCO2 and VO2. Rating of perceived exertion (RPE)26 on the 10-point Borg scale was assessed immediately after the end of the graded exercise hand cycle test. PO was increased – through a pulley system that was positioned behind the treadmill and connected to the rear wheel axle of the hand cycle by a rope22 – by adding extra weight (Fadd in N). External PO was calculated from rolling resistance (Froll), added load (Fadd) and treadmill belt velocity (v) according to:

Froll was determined in a separate drag test with the subject sitting passively in the hand cycle.27
Hand cycle
Subjects were tested using their own rigid frame wheelchair and attach-unit hand cycle (Figure 1). If the subject did not own one, the rehabilitation centre provided a hand cycle. All hand cycles were equipped with a synchronous crank system and a bullhorn steer (Double Performance, Gouda, The Netherlands). The crank axis of the steering was positioned as low as possible.
Statistics
For each participant, a linear regression analysis was performed and Pearson's correlation coefficient (r) was calculated, using the paired data of VO2 and HR values of each exercise block. The actual error of the predicted VO2 from the regression equation is commonly10, 14 reflected by the SEE, expressed in the units of measurement. To determine the accuracy of the VO2 prediction in the individual regression equations, the SEE was calculated according to:

where is the SD of the individual data points and r is the individual HR–VO2 Pearson's correlation coefficient.
Because absolute values of SEE(VO2) do depend on the individual range of VO2 (ie range between VO2 rest and VO2 peak: VO2R=VO2peak−VO2rest), SEE is also expressed as a percentage of the individual VO2R. The SEE of VO2R, given a certain HR, can be interpreted the same way as the SD and the 95% confidence interval of the predicted value can be calculated. For example, a recommended range of training intensity of 60–85% HRR (is comparable to 60–85% VO2R28) would allow an HR corresponding with 72% HRR (or VO2R) and SEE⩽6% HRR (or VO2R) to actually train within this range. Statistical analyses were performed with SPSS 12.01 for Windows.
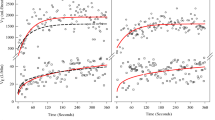
Results
In Table 2, the physiological characteristics are presented for all subjects divided over the C5–C6 and the C7–C8 lesion group. All subjects attained the VO2peak during the last exercise bout. It was found that 17 out of 20 subjects reached an RER above 1.00. Subjects 1 and 14 reached an RER of 0.97 and subject 6 an RER of 0.93. Eleven subjects scored an RPE of 6 or lower on the 10-point Borg scale. Two subjects (15 and 16) had a very low physical capacity and were able to complete only three exercise intervals of the peak capacity test. Because of the low number of data points, these subjects were excluded from the analysis. Table 3 shows Pearson's r and SEE of the paired HR and VO2 for the remaining participants (n=18). Individual data points and regression lines of representative subjects of the C5–C6 group and the C7–C8 group are shown in Figure 2. Pearson's r ranged from 0.68 to 0.97 (mean 0.81±0.12) for the C5–C6 group and from 0.79 to 0.97 (mean 0.91±0.07) for the C7–C8 group. The results of the SEE(VO2) showed mean values of 57±25 ml/min in the C5–C6 group and 67±39 ml/min in the C7–C8 group. The SEE(%VO2R) showed mean values of 10.6±5.6% in the C5–C6 group and 7.0±3.2% in the C7–C8 group, respectively. The mean r for the whole group was 0.87±0.10 and the SEE(%VO2R) was 8.6±4.6%.
In Table 3, it is shown that two subjects of the C5–C6 group and six subjects of the C7–C8 group attained a SEE⩽6.0%VO2R. All these subjects showed Pearson's r of 0.90 or higher. In Table 4 mean values of POpeak, HRpeak, HRR, VO2peak and VO2R of subjects with SEE⩽6.0% (n=8) and SEE>6.0%VO2R (n=10) are shown. These two groups showed no significant differences.
Discussion
The aim of this study was to examine the individual HR–VO2 relationships in subjects with TP to answer the question whether HR can be used to quantify exercise intensity in persons with TP. We found a satisfactory linear relationship in eight out of 18 subjects, indicating that HR is useful in some, but not all persons with TP.
Strength of the HR–VO2 relationship
According to the ACSM guidelines, a training intensity is prescribed as a range5; for example, training hard within 60–85% HRR or VO2R. With an estimated training intensity of 72% HRR or VO2R and an SEE of 6%VO2R, it can be assumed with 95% confidence that the actual training intensity is between 60 and 84%. Therefore, in our opinion, an SEE of ±6%VO2R is acceptable as it keeps training intensity within the required range. Eight out of 18 subjects had an SEE lower than the cutoff value of 6% and are assumed to have a satisfactory linear HR–VO2 relationship. All these eight subjects also had a correlation coefficient of 0.90 or higher.
Well-trained athletes with a PP in studies of Goosey et al10 and Tolfrey et al14 showed much higher mean Pearson's r-values of 0.97±0.02 and 0.99±0.01, respectively, as well as a lower SEE of 3.4±1.4 and 2.6±1.0% HRpeak, respectively, than subjects in the current study (see Table 3). Two other studies showed lower Pearson's r-values in subjects with PP, ranging from 0.85–0.999 to 0.74–0.99.12 Both studies concluded that a linear relationship exists, whereas the correlation coefficients, at least in some subjects, were rather low. The mean Pearson's r-values of our study are comparable with McLean et al20 during arm cranking (mean r=0.85) and higher than values presented by Coutts et al21 and Schmid et al13 (r=0.65 and 0.69, respectively) during wheelchair propulsion. McLean et al20 concluded that HR should not be used for prescribing exercise for individuals with TP because HR and VO2 are too variable to accurately reflect the work being carried out. Unfortunately, none of these authors presented their data with an SD or SEE.
The above-mentioned studies indicate that a linear relationship exists in persons with a PP below Th4,9, 10, 12, 14 but not in (all) persons with TP.13, 20, 21 In the current study, the HR–VO2 relationship was found to be linear in only eight out of 18 subjects. The unstable relationship in the other 10 subjects may be explained by the disturbed sympathetic innervation or other factors related to the low physical capacity and muscle mass involved.
The disturbed sympathetic system
Persons with TP have a low HRpeak and consequently often also a small HRR (HRpeak–HRrest). Our results show that a small HRR or low HRpeak, for example, in subjects 4, 6 and 10 (Figure 2a), does not necessarily result in a lower correlation coefficient or a higher SEE, as is shown in Table 4. This is not in agreement with Mc Lean et al,20 who explained the higher HR–VO2 correlation in the supine position compared to the sitting position, by the significant higher range over which the HR can accelerate.
The severity of cardiovascular dysfunction after SCI correlates well with the severity of injury to the spinal motor and sensory pathways scored with the ASIA.29 Nevertheless, in subjects with ASIA B and possibly even in ASIA A, there is still a chance of survival of some autonomic fibres that extend below injury level. It is unclear from our results what the influence of the disturbed sympathetic system on HR or blood flow and O2 transport to the muscles might have been in our subjects. From the study of Hjeltnes et al,17 however, it appeared that the observed arterial PO2 was low, but not the limiting factor during increased work loads in individuals with motor complete TP.
AD could also be responsible for a disturbed HR–VO2 relationship owing to a sudden rise or fall in HR-values. However, subjects were screened before and throughout the test for symptoms of AD and no symptoms occurred. AD should be prevented because in some cases extremely high BP-values can even lead to death from cardiac dysfunction or a stroke.18
Physical capacity
Two subjects (15 and 16) had to be excluded from further analysis because they were not able to complete more than three blocks, despite very small increments per bout (2 W). A very low physical capacity is often seen in these subjects, especially in (untrained) persons with a C5–C6 lesion. Consequently, the influence of a measurement error (an outlier) or normal fluctuations in VO2 will be relatively large, when only few data points are spread out over a small VO2R. This may be a possible explanation for the lower correlation in some subject (13 and 20, see also Figure 2d). Subjects 12 and 17 (Figure 2c), both with a relatively large VO2R, are the only subjects from the C5–C6 group with an acceptable Pearson's r.
However, our results show that a large VO2R (eg subject 1 in Figure 2b) does not always results in a satisfactory linear relationship as is shown in our results: No significant differences in POpeak, VO2peak and VO2R were found between the eight subjects with satisfying Pearson's r and SEE and the other 10 subjects, as is shown in Table 4. On the other hand, it seems that an extremely low physical capacity and VO2R always coincidence with an unstable HR–VO2 relationship.
Limitations of the study
It was beyond the scope of the current study to clarify the influence of the disturbed sympathetic system on the individual HR–VO2 relationship in persons with TP. However, it would be interesting in future to investigate the influence of the sympathetic system on the HR–VO2 relationship during exercise as well: by measuring BP, catecholamine concentration13 and blood gas, as was performed by Hjeltnes et al17or by analysing the beat-to-beat HR variability30 or BP variability.31
Moreover, it should be remarked that in this study we have not looked into the reproducibility of the found regression equations. It may be possible that the day-to-day variability has an influence on the individual regression equations. Even in able-bodied people intraindividual variability can be substantial between days.32
Practical implications
Results of this study showed that HR is useful in some, but not all, individuals with TP to monitor training intensity. The Borg scale may be a possible alternative, indicating the overall perceived exertion. However, the rather low RPE values at the end of the test and the reported local (arm) muscle soreness as reason for stopping indicate that using the Borg scale to monitor training intensity has severe limitations for persons with TP. Another option to monitor training intensity is continuously monitoring of PO and subsequently training at %POpeak. For hand cycling commercially available power measuring crank systems used in cycling, may be suitable. However, to our knowledge, the validity and reliability has not been tested in hand cycling at low PO levels seen in persons with TP.
Conclusion
From our data, it appears that the HR–VO2 relationship was found to be linear in eight out of 20 individuals with an acceptable SEE(%VO2R)⩽6.0% and a r>0.90. Therefore, HR can be used in some, but not all, individuals with TP to monitor training intensity. No single reason such as a low HRR as a consequence of the disturbed autonomic nervous system, AD or the limited physical capacity could be indicated to explain the HR–VO2 relationship. It is therefore likely that a combination of these factors is responsible for the lack of a linear HR–VO2 relationship. Our results, however, did not allow elucidating the underlying mechanisms why some subjects have, and others do not have, a useful HR–VO2 relationship. It is concluded that the use of HR as an indicator of training intensity should be reconsidered in persons with TP: An individual analysis of the HR–VO2 relationship is necessary to determine whether HR can be used to prescribe exercise intensity. Further research should focus on the test–retest reliability and alternative indicators of training intensity such as percentage peak PO should be explored.
References
Figoni SF . Exercise management for persons with chronic diseases and disabilities. In: Durstine JL, Moore GE (eds). Spinal Cord Disabilities: Paraplegia and Tetraplegia. 2nd edn. Human Kinetics: Champaign, IL, USA, 2003, pp 247–253.
Dallmeijer AJ, van der Woude LH, Hollander AP, van As HH . Physical performance during rehabilitation in persons with spinal cord injuries. Med Sci Sports Exerc 1999; 31: 1330–1335.
Janssen TW, van Oers CA, Veeger HE, Hollander AP . Relationship between physical strain during standardised ADL tasks and physical capacity in men with spinal cord injuries. Paraplegia 1994; 32: 844–859.
Kilkens OJ, Post MW, van der Woude LH, Dallmeijer AJ, van den Heuvel WJ . The wheelchair circuit: reliability of a test to assess mobility in persons with spinal cord injuries. Arch Phys Med Rehab 2002; 83: 1783–1788.
Pollock ML et al. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness in healthy adults. Med Sci Sports Exerc 1998; 30: 975–991.
Hooker SP, Wells CL . Effects of low- and moderate-intensity training in spinal cord-injured persons. Med Sci Sports Exerc 1989; 21: 18–22.
DiCarlo SE . Effect on arm ergometry training on wheelchair propulsion endurance of individuals with quadriplegia. Phys Ther 1983; 63: 1104–1107.
Hopman TE, Dallmeijer AJ, Snoek G, van der Woude LHV . The effect of training on cardiovascular responses to arm exercise in individuals with tetraplegia. Eur J Appl Physiol 1996; 74: 172–179.
Bar-on ZH, Nene AV . Relationship between heart rate and oxygen uptake in thoracic level paraplegics. Paraplegia 1990; 28: 87–95.
Goosey-Tolfrey VL, Tolfrey K . The oxygen uptake–heart rate relationship in trained female wheelchair athletes. J Rehab Res Dev 2004; 41: 415–420.
Hjeltnes N . Oxygen uptake and cardiac output in graded arm exercise in paraplegics with low level spinal lesions. Scand J Rehab Med 1977; 9: 107–113.
Hooker SP, Greenwood JD, Hatae DT, Husson JS, Matthiesen TL, Waters AR . Oxygen uptake and heart rate relationship in persons with spinal cord injury. Med Sci Sports Exerc 1993; 25: 1115–1119.
Schmid A et al. Catecholamines, heart rate, and oxygen uptake during exercise in persons with spinal cord injury. J Appl Physiol 1998; 85: 635–641.
Tolfrey K, Goosey-Tolfrey VL, Campbell IG . Oxygen uptake–heart rate relationship in elite wheelchair racers. Eur J Appl Physiol 2001; 86: 174–178.
Glaser RM . Arm exercise training for wheelchair users. Med Sci Sports Exerc 1989; 21: S149–S157.
Freyschuss U, Knutsson E . Cardiovascular control in man with transverse cervical cord lesions. Life Sci 1969; 8: 421–424.
Hjeltnes N, Christensen CC, Rostrup M, Walberg-Hendriksson H . Altered Blood Pressure Response to Graded Exercise in Tetraplegic Subjects With Low Levels of Catecholamines. In: Hjeltnes N (ed). Thesis: Physical exercise and electrical stimulation in the management of metabolic, cardiovascular and skeletal-muscle alterations in people with tetraplegia (paper III), 1998.
Eltorai I, Kim R, Vulpe M, Kasravi H, Ho W . Fatal cerebral haemorrhage due to autonomic dysreflexia in a tetraplegic patient: case report and review. Paraplegia 1992; 30: 355–360.
Schmid A et al. Catecholamines response of high performance wheelchair athletes at rest and during exercise with autonomic dysreflexia. Int J Sports Med 2001; 22: 2–7.
McLean KP, Jones PP, Skinner JS . Exercise prescription fot sitting and supine exercise in subjects with quadriplegia. Med Sci Sports Exerc 1995; 27: 15–21.
Coutts KD, Rhodes EC, McKenzie DC . Submaximal exercise responses of tetraplegics and paraplegics. J Appl Physiol 1985; 59: 237–241.
Dallmeijer AJ, Zentgraaff ID, Zijp NI, van der Woude LHV . Submaximal physical strain and peak performance in handcycling versus handrim wheelchair propulsion. Spinal Cord 2004; 42: 91–98.
van der Woude LHV et al. Alternative modes of manual wheelchair ambulation: An overview. Am J Phys Med Rehab 2001; 80: 765–777.
Maynard Jr FM et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Mathias CJ, Frankel HL . Autonomic failure; a textbook of clinical disorders of the autonomic nervous system. In: Bannister R, Mathias CJ (eds). Autonomic Disturbances in Spinal Cord Lesions. 3rd edn. Oxford University Press: Oxford 1992, pp 839–881.
Borg GAV . Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 4: 377–381.
van der Woude LHV et al. Wheelchair ergonomics and physiology testing of prototypes. Ergonomics 1986; 29: 1561–1573.
Swain DP, Leutholtz BC . Heart rate is equivalent to %VO2Reserve, not to%VO2max. Med Sci Sports Exerc 1997; 29: 410–414.
Furlan JC, Fehlings MG, Shannon P, Norenberg MD, Krassioukov AV . Descending vasomotor pathways in humans: correlation between axonal preservation and cardiovascular dysfunction after spinal cord injury. J Neurotrauma 2003; 20: 1351–1362.
Grimm DR, De Meersman RE, Almenoff PL, Spungen AM, Bauman WA . Sympathovagal balance of the heart in subjects with spinal cord injury. Am J Physiol 1997; 272: 835–842.
Wecht JM, de Meersman RE, Weir JP, Bauman WA, Grimm DR . Effects of autonomic disruption and inactivity on venous vascular function. Am J Physiol Heart Circ Physiol 2000; 278: 515–520.
Mc Crory MA, Mole PA, Nommsen-Rivers LA, Dewey KG . Between-day and within-day variability in the relation between heart rate and oxygen consumption: effect on the estimation of energy expenditure by heart-rate monitoring. Am J Clin Nutr 1997; 66: 18–25.
Acknowledgements
This study was supported by ZON-MW (Grant number: 014-32-012), The Netherlands Organisation for Health, Research and Development, The Hague.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Valent, L., Dallmeijer, A., Houdijk, H. et al. The individual relationship between heart rate and oxygen uptake in people with a tetraplegia during exercise. Spinal Cord 45, 104–111 (2007). https://doi.org/10.1038/sj.sc.3101946
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101946
Keywords
This article is cited by
-
The ability of heart rate or perceived exertion to predict oxygen uptake varies across exercise modes in persons with tetraplegia
Spinal Cord (2021)
-
Interrater and intrarater reliability of ventilatory thresholds determined in individuals with spinal cord injury
Spinal Cord (2019)
-
The influence of protocol design on the identification of ventilatory thresholds and the attainment of peak physiological responses during synchronous arm crank ergometry in able-bodied participants
European Journal of Applied Physiology (2019)
-
The intensity and match load comparison between high spinal cord injury and non-spinal cord injury wheelchair basketball players: a case report
Spinal Cord Series and Cases (2016)
-
Validity of heart rate indexes to assess wheeling efficiency in patients with spinal cord injuries
Spinal Cord (2014)