Abstract
Study design:
Case report.
Objectives:
To report a case with giant cell tumor (GCT) of C6 vertebra, in which three-dimensional (3-D) full-scale modeling of the cervical spine was useful for preoperative planning and intraoperative navigation.
Setting:
A university hospital in Japan.
Case report:
A 27-year-old man with a GCT involving the C6 vertebra presented with severe neck pain. The C6 vertebra was collapsed and the tumor had infiltrated around both vertebral arteries (VAs). A single-stage operation combining anterior and posterior surgical procedures was scheduled to resect the tumor and stabilize the spine. To evaluate the anatomic structures within the surgical fields, we produced a 3-D full-scale model from the computed tomography angiography data. The 3-D full-scale model clearly showed the relationships between the destroyed C6 vertebra and the deviations in the courses of both VAs. Using the model, we were able to identify the anatomic landmarks around the VAs during anterior surgery and to successfully resect the tumor. During the posterior surgery, we were able to determine accurate starting points for the pedicle screws. Anterior iliac bone graft from C5 to C7 and posterior fixation with a rod and screw system from C4 to T2 were performed without any complications. Postoperatively, the patient experienced relief of his neck pain.
Conclusion:
The 3-D full-scale model was useful for simultaneously evaluating the destruction of the vertebral bony structures and the deviations in the courses of the VAs during surgery for GCT involving the cervical spine.
Similar content being viewed by others
Introduction
Although giant cell tumors (GCTs) of bone have a benign histology, they are locally aggressive tumors. GCT rarely arises in the spine; only 1.3–2.9% of all GCTs of bone involve vertebra above the sacrum.1, 2 Surgical treatment for GCT involving the vertebral column has been considered highly dangerous because of the presence of neurovascular structures. Previous reports have indicated that wide and complete excision of spinal GCTs is often difficult and that the recurrence rate following surgery is 11–42%.1, 3, 4
Among the GCTs involving the spine, complete removal of the tumor from the cervical spine is particularly challenging if a vertebral artery (VA) lies close to the neoplasm. Anterior tumor resection from the cervical spine is generally difficult because vertebral bodies are frequently collapsed by infiltrating tumor, and anatomical landmarks in the operative fields are often difficult to identify. In several reported cases of GCT involving the cervical spine, the authors decided against total excision of the tumor owing to the potential risk of VA injury.5, 6
In the present report, we describe our experience with surgical treatment of a patient with a GCT involving the C6 vertebra. Before the surgery, we produced a three-dimensional (3-D) full-scale model of the cervical spine from the computed tomography (CT) angiography data using the rapid prototyping (RP) technique. The model clearly showed the anatomical relationship between the destroyed vertebral bony structures and deviations in the paths of the VAs. This information greatly assisted our efforts to excise the tumor and stabilize the spine.
Case report
A 27-year-old man was admitted to our hospital with neck pain of 6 months duration. Four months previously, after his neck pain increased in the absence of trauma, the patient consulted doctors at another hospital. Radiological examination revealed that he had a fracture of the C6 vertebra, and additional CT examination suggested that the fracture might be pathological. A needle biopsy established a diagnosis of GCT. The patient underwent selective arterial embolization of the tumor as an alternative to surgery. Following the third embolization, which was performed 2 months before his admission to our hospital, the patient felt severe pain in his upper and lower extremities accompanied by motor weakness in his left leg and sensory loss in his right trunk and leg. His motor weakness gradually recovered, but the patient refused further embolization treatments and was referred to our hospital for surgical treatment of the tumor.
On admission, the patient had severe neck pain and needed a Philadelphia collar for sitting. Hypalgesia was present in the right trunk and leg below the level of the T1 segment. Muscle power was almost normal. Deep tendon reflexes were increased in his lower extremities, and he had a spastic gait.
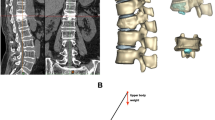
Cervical spine radiographs showed a pathological fracture of C6. Mid-sagittal reconstruction of the CT images showed that almost all areas of the C6 vertebral body were osteolytic (Figure 1). Axial CT images at the C6 pedicle level showed bilateral destruction of the transverse foramina (Figure 1) and tumor infiltration into the left C6 pedicle and lamina (Figure 1, arrow). Enhanced CT showed that the tumor had also infiltrated around both VAs and that both VAs were shifted laterally (Figure 1, arrowheads). Magnetic resonance images showed tumor infiltration into the spinal canal and close to the dura mater at the C6 level, but compression of the spinal cord was not seen.
Mid-sagittal reconstruction of a CT image of the cervical spine (left) shows the collapse of the C6 vertebra. CT at the level of the C6 pedicle (right, upper) shows that almost all areas of the C6 vertebral body are osteolytic. The arrow shows tumor infiltration into the left lamina. Enhanced CT at the mid-vertebral level of C6 (right, lower) shows tumor infiltration around both VAs (arrowheads)
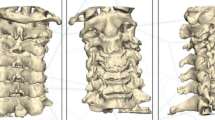
To better evaluate the local anatomical structures in this patient, we produced a 3-D full-scale model of the cervical spine from the CT angiography data using the RP technique, employing the binder jet method.7 Our 3-D full-scale model clearly showed destruction of the C6 vertebra (Figure 2, asterisk) and the deviations in the courses of both VAs (Figure 2, arrowheads). We then performed a simulation of surgery using this model, inserting pedicle screws at C4, C5, T1 and T2 bilaterally (Figure 3). CT images of the simulated screw insertions showed that the insertion points of the left screws were positioned too far laterally, causing these screws to penetrate the medial wall of the transverse foramen uncomfortably close to the left VA (Figure 3, arrowheads). The results of the surgery simulation demonstrated the necessity of positioning the insertion points of the screws more medially during the actual surgery.
Simulation of surgery was performed using the 3-D full-scale model (left). Pedicle screws were inserted at C4, C5, T1 and T2 and fixed with a 4.75 mm diameter rod. CT images of the model at C4 (right, upper) and C5 (right, lower) levels show the path of the screws. On the left side, the screws were deviated toward the lateral side, penetrating the wall of the transverse foramen uncomfortably close to the left VA (arrowheads)
Our resection of the tumor and stabilization of the spine consisted of a single-stage operation combining anterior and posterior surgical procedures. Starting with a posterior approach, we performed a fenestration at the left C6 lamina and excised the tumor around the left C6 nerve root. We then inserted pedicle screws at C4, C5, T1 and T2 and performed a C4–T2 posterior fixation with a screw and rod system, utilizing the results of the surgery simulation to properly locate the insertion points of the screws. We then moved the patient into a supine position. Using an anterior approach, we performed a C6 corpectomy and extirpation of the tumor. Finally, we then performed a C5–C7 fusion using an autograft from the right iliac crest. During the anterior surgery, we were able to identify clearly the VAs and to resect the tumor around the VAs based upon the information provided by the 3-D full-scale model (Figure 4). Pathological examination of the extirpated tumor showed multinucleated giant cells and spindle-shaped cells, findings typical of GCT.
Postoperatively, the patient was again fitted with a Philadelphia collar for 3 months, after which time further cervical orthosis was no longer required. After surgery, the patient experienced relief from neck pain, and he returned to work 3 months after surgery. Cervical radiographs 6 months after surgery showed successful C5–C7 fusion (Figure 5) and no evidence of tumor recurrence. CT images at this time showed that the C4 and C5 pedicle screws were properly positioned (Figure 5).
Discussion
RP, a technique initially developed for industrial purposes, is increasingly being utilized in surgical planning. In the field of plastic surgery and craniofacial surgery, RP has been clinically applied to the reconstruction of cranial, mandibular and facial bones.7 In the field of trauma surgery, Brown et al8 have produced RP 3-D models of multi segmentary acetabular fractures, which they use to simulate fracture reduction and fixation with plate and screws before carrying out these procedures in the operating room. The authors reported that these 3-D models enabled them to easily evaluate the complex structures of fractured bone and to then treat the fractures with improved precision.
In the field of spine surgery, D'Urso et al9 produced 3-D full-scale models from raw CT data for five patients with complex spinal deformities and reported on the usefulness of the models for morphological assessment, intraoperative navigation and rehearsal of surgery. To the best of our knowledge, however, no reports have described 3-D models that can directly evaluate the courses of VAs inside the cervical spine. In the present case, the tumor extended close to the VAs on both sides, deviating the VA courses laterally, and caused evident destruction of both VA foramina. Anticipating that the detection of VAs within the operative field would be difficult, we produced a 3-D full-scale model from the CT angiography data to simultaneously evaluate the bony structures and the blood vessel courses. Our model clearly showed the relationships between the VAs and the vertebral destruction, facilitating our understanding of the anatomical landmarks around the VAs and thereby enabling us to excise the tumor.
Previously published biomechanical analyses have shown that pedicle screw fixation is the most rigid fixation method of the cervical spine.10 However, several authors have expressed concern that inserting pedicle screws into the C3–C6 pedicles would be associated with an unacceptable risk of VA injury.11, 12 In a study of their experiences with the insertion of 669 pedicle screws into the cervical spine, Abumi et al10 reported that 45 screws (6.7%) penetrated the pedicle, causing injury to the VA in one patient.
In the present case, we performed simulation of the surgical pedicle screw insertion at C4 and C5 using our 3-D full-scale model. Through this simulation, we were able to determine accurately the starting points for the pedicle screws before the actual surgery, and we did successfully insert the screws. This experience confirmed that simulation of surgery using a 3-D full-scale model can improve the accuracy and safety of reconstructive surgery of the cervical spine.
References
Savini R, Gherlinzoni F, Morandi M, Neff JR, Picci P . Surgical treatment of giant-cell tumor of the spine. The experience at the Istituto Ortopedico Rizzoli. J Bone Joint Surg Am 1983; 65: 1283–1289.
Goldenberg RR, Campbell CJ, Bonfiglio M . Giant-cell tumor of bone. An analysis of two hundred and eighteen cases. J Bone Joint Surg Am 1970; 52: 619–664.
Sanjay BK, Sim FH, Unni KK, McLeod RA, Klassen RA . Giant-cell tumours of the spine. J Bone Joint Surg Br 1993; 75: 148–154.
Turcotte RE, Biagini R, Sim FH, Unni KK . Giant cell tumor of the spine and sacrum. Chir Organi Mov 1990; 75 (Suppl 1): 104–107.
Erdogan B, Volkan Aydin M, Sen O, Sener L, Bal N, Yalcin O . Giant cell tumour of the sixth cervical vertebrae with close relationship to the vertebral artery. J Clin Neurosci 2005; 12: 83–84.
Michalowski MB et al. Giant cell tumor of cervical spine in an adolescent. Med Pediatr Oncol 2003; 41: 58–62.
Ono I, Abe K, Shiotani S, Hirayama Y . Producing a full-scale model from computed tomographic data with the rapid prototyping technique using the binder jet method: a comparison with the laser lithography method using a dry skull. J Craniofac Surg 2000; 11: 527–537.
Brown GA, Firoozbakhsh K, DeCoster TA, Reyna Jr JR, Moneim M . Rapid prototyping: the future of trauma surgery? J Bone Joint Surg Am 2003; 85 (Suppl 4): 49–55.
D'Urso PS et al. Spinal biomodeling. Spine 1999; 24: 1247–1251.
Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K . Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine 2000; 25: 962–969.
Roy-Camille R, Mazel C, Saillant G, Benazet JP . Rationale and techniques of internal fixation in trauma of the cervical spine. In: Errico T, Bauer RD, Waugh WT (eds). Spine Trauma. JB Lippincott: Philadelphia 1991, pp 163–169.
Albert TJ, Vacarro A . Postlaminectomy kyphosis. Spine 1998; 23: 2738–2745.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Yamazaki, M., Akazawa, T., Okawa, A. et al. Usefulness of three-dimensional full-scale modeling of surgery for a giant cell tumor of the cervical spine. Spinal Cord 45, 250–253 (2007). https://doi.org/10.1038/sj.sc.3101959
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101959
Keywords
This article is cited by
-
3D printing-assisted extended lateral approach for displaced intra-articular calcaneal fractures: a systematic review and meta-analysis
Journal of Orthopaedic Surgery and Research (2021)
-
3D preoperative planning for humeral head selection in total shoulder arthroplasty
MUSCULOSKELETAL SURGERY (2020)
-
Multimaterial 3D printing preoperative planning for frontoethmoidal meningoencephalocele surgery
Child's Nervous System (2018)
-
Surgical simulation of circumferential osteotomy and correction of cervico-thoracic kyphoscoliosis for an irreducible old C6–C7 fracture dislocation
Acta Neurochirurgica (2009)