Abstract
Study design:
Case report and review of the literature.
Objective:
To report an unusual case of a spinal intradural extramedullary cavernous angioma (CA), located at the cauda equina, and to compare it with the previously published 22 surgically treated cases in the literature.
Setting:
Ankara, Turkey.
Method:
A 67-year-old man presented with a 4-month history of back pain and sciatica and a 4-week history of progressive lower extremity paresthesia, difficulty walking, and loss of bladder and bowel sphincter control. Neurological examination revealed bilateral hypoesthesia below the T12 dermatome with spastic paraparesis. Magnetic resonance imaging (MRI) of the cauda equina revealed a heterogeneous enhancing intradural extramedullary mass obliterating the spinal canal and expanding the spinal cord. T12 laminectomy and total tumor removal were performed without additional neurological deficit. Pathological examination confirmed the diagnosis of a CA.
Result:
The patient's neurological status improved during postoperative recovery. He was ambulatory without assistance and regained full sphincter control on the eighth postoperative week.
Conclusion:
CAs of the spinal cord are extremely rare lesions. Typically, they present with low back pain and sciatica, neurological deficits, or as a subarachnoid hemorrhage. These lesions have characteristic features on MRI and should be considered in the differential diagnosis of intradural spinal lesions. Following a thorough literature review of reported cases, the authors propose that for patients presenting with severe preoperative neurological signs, immediate microsurgical tumor excision or decompression increases the chance of neurological improvement.
Similar content being viewed by others
Introduction
Cavernous angiomas (CAs), or cavernomas, are vascular malformations consisting of vascular spaces lined with a single endothelial layer without neural or glial elements.1 These lesions belong to a group of intracranial vascular malformations that are developmental malformations of the vascular bed. Spinal CAs are typically located in the vertebral body; cases of intradural extramedullary CAs are exceedingly rare.2 To date, there have been only 22 surgically treated cases of intradural extramedullary CAs reported (Table 1). Here, we present a case report of a patient with a lower thoracic intradural extramedullary CA. The patient underwent surgical resection of the tumor, and the literature was reviewed to discuss the clinical, radiological, and therapeutic features of these uncommon lesions.
Case report
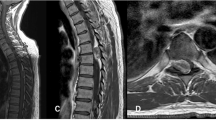
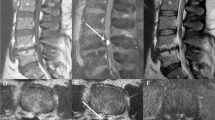
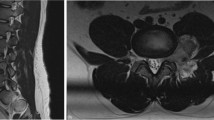
A 67-year-old man with a 4-month history of back pain and sciatica and a 4-week history of progressive lower extremity paresthesia, difficulty walking, and loss of bladder and bowel sphincter control was admitted to the hospital. Neurological examination revealed bilateral hypoesthesia below the T12 dermatome. Lower extremity paresis was present with 3/5 muscle strength and increased patellar and Achilles reflexes associated with bilateral extensor plantar responses. Magnetic resonance imaging (MRI) of the spine revealed a heterogeneous enhancing intradural extramedullary mass obliterating the spinal canal and expanding the spinal cord at the T12–L1 level; the lesion was hyperintense on T1 and hypointense on T2-weighted images (Figure 1a–c).
A T12 laminectomy was performed and the tense dura was opened. A 1.5 × 3 cm, dark-bluish mass was evident between the adherent nerve roots, which displaced the cord to the right side. After dissecting the arachnoid membranes, the mass remained closely adherent to a single thin nerve root that was encapsulated within the lesion. The mass was completely excised after sacrificing this root. Histopathological examination confirmed a CA with numerous small vessels and large dilated sinusoidal spaces lined with a single cell layer. The vascular channels were immediately adjacent to each other, without intervening nervous tissue (Figure 2). The course of postoperative recovery was uneventful, and the patient's motor strength improved to 4/5 immediately following the operation. The patient was discharged after 5 days without pain. Return of sphincter control and motor strength was close to normal at postoperative week 8.
Histological appearance of CA showing irregular, immediately adjacent, cavernous vascular spaces. The walls of the vascular spaces are lined by a single layer of endothelium and show thickening from fibrous and hyaline material. Note absence of nervous tissue between the vascular spaces (hematoxylin and eosin × 40)
Review of the literature
Table 1 provides a summary of the 23 reported surgically treated cases of spinal intradural extramedullary CAs, including the present report.1, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 The ages of the patients are between 22 and 67 years, with an average of 43.3 year (Table 1). 65.2% of the patients presenting with intradural extramedullary spinal CAs are males. Most of the lesions (including the present case) were located in the lower thoracic region; only three cases involved the cervical region. The clinical symptoms were most often the result of local compression of the nerve roots and/or the spinal cord. Progressive radiculopathy or myelopathy were the major symptoms in nine cases, and five patients had complete loss of sphincter control. Acute pain and sensorimotor deficits were present in 13 cases and subarachnoid hemorrhage was observed in nine of the cases. As a unique case, one patient diagnosed with a cauda equina CA had symptoms of elevated intracranial pressure resulting from hydrocephalus.11 Intraoperatively, 18 cases were found to be adherent to the nerve roots or the spinal cord. Total excision was achieved in 17 cases with preservation of neural tissue, and incomplete resection was performed in cases where the lesion was tightly adherent to the spinal cord. 69.5% of cases resulted in excellent postoperative recoveries; exceptions included patients with severe neurological deficits such as sphincter dysfunction, and patients presenting with strongly adherent spinal cord lesions.
Discussion
CAs are benign vascular lesions of the central nervous system and represent 5–16% of spinal vascular anomalies, usually located within the vertebral bodies.20 However, approximately 3% of CAs are located intradurally, usually intramedullary but occasionally extramedullary.1, 2 An intradural extramedullary CA was first reported by Hadlich et al,21 as an autopsy finding. Later, Turner and Kernohan22 described a second case (also during autopsy). Including the present study, 23 cases of spinal intradural extramedullary CAs have now been reported in the literature.
CAs are well demarcated lesions. They consist of irregular sinusoidal vascular spaces lacking intervening neural or glial tissue,14, 22, 23 and are lined by a single layer of endothelium.22, 23 These lesions may arise from blood vessels of the nerve roots, the inner surface of the dura mater, and the pial surface of the spinal cord. This relationship likely explains the close adherence of the lesion to the spinal nerve roots or the spinal cord. In 19 of the cases, the cavernoma was adherent to a spinal nerve root and in three cases (including our case), the root was encapsulated within the lesion (Table 1). Therefore, we suggest that this vascular malformation most likely originated from the abnormal development of periradicular vessels.
Subarachnoid hemorrhage may present as the initial symptom of this highly vascular neoplasm,8, 9, 13, 15 as significant bleeding from this malformation occurs in more than 25% of cases.1 This may, in part, be the result of the marked vascularity of this lesion coupled to its restricted mobility, resulting from entrapment of spinal nerve roots, within the dynamic vertebral canal.19
Intradural extramedullary spinal CAs have characteristic features different from other spinal cord tumors and vascular malformations on MRI.24 The presence of mixed subacute and chronic hemorrhage, evident by mixed high- and low-signal intensity components may be characteristics of these lesions.25 The presence of a webbed core of mixed signal intensity circumscribed by a border of hypointensity (macrophage uptake of hemosiderin) in T1- and T2-weighted images is highly suggestive of CA.25 Spinal angiography does not reveal these lesions.17
Macroscopically, the lesions are well demarcated and total excision was possible in 19 of 23 cases, even though the lesions were closely attached to nerve roots. In the two cases described by Pagni et al10 and Nozaki et al,19 the mass was excised along with the attached thin nerve root, as encapsulation within the lesion made it impossible to preserve, despite careful microsurgical dissection. As in these two cases reported previously,10, 19 resection of the thin nerve root in the current report did not compromise good postoperative recovery.
Conclusions
Intradural extramedullary spinal CAs are extremely rare. They may initially present as low back pain with sciatica, neurological deficits, or as a subarachnoid hemorrhage. The clinical outcome depends largely on the patient's preoperative neurological status, and optimal treatment consists of total excision of the lesion with careful microsurgical technique. Based on a through review of the cases reported in the literature, it is thought that patients presenting with severe preoperative neurological signs will have the best chance of neurological improvement with microsurgical excision of the tumor or decompression.
Duality of interest
None declared.
References
Mastronardi L, Ferrantel L, Scarpinati M, Gigliardi FM, Celli P, Fortuna A . Intradural extramedullary cavernous angioma: case report. Neurosurgery 1991; 29: 924–926.
Harrison MJ, Eisenberg MB, Ullman JS, Oppenheim JS, Camins MB, Post KD . Symptomatic cavernous malformations affecting the spine and spinal cord. Neurosurgery 1995; 37: 195–205.
Roger H, Paillas JE, Bonnal J, Vigorous M . Angiomes de la moelle et des racines. Acta Neurol Psych Belgium 1951; 7: 491–495.
Floris V . Angiomie angiomatosi del sistema nervoso. Lav Neuropsich 1958; 27: 159–179.
Hirsch JF, Pradat P, David M . Cavernous angioma of the cauda equina. Neurochirurgie 1965; 11: 323–327 (Fr).
Pansini A, Lo Re F . Laro caso di angiocavernoma della cauda. Mem Soc Tos Um Chir 1966; 27: 679–696.
Ortner WD, Kubin H, Pilz P . Ein zervikales kavernoeses angiom. Fortschr Roengtenstr 1973; 118: 475–476.
Heimberger K, Schnaberth G, Koos W, Pendl G, Auff E . Spinal cavernous haemangioma (intradural-extramedullary) underlying repeated subarachnoid hemorrhage. J Neurol 1982; 226: 289–293.
Ueda S, Saito A, Inomori S, Kim I . Cavernous angioma of the cauda equina producing subarachnoid hemorrhage. Case report. J Neurosurg 1987; 66: 134–136.
Pagni CA, Canevero S, Forni M . Report of a cavernoma of the cauda equina and review of the literature. Surg Neurol 1990; 33: 124–131.
Ramos Jr F, de Toffol B, Aesch B, Jan M . Hydrocephalus and cavernoma of the cauda equina. Neurosurgery 1990; 27: 139–142.
Mori K, Ishii H, Tomita Y, Nakajima K, Morimoto K, Maeda M . Intradural-extramedullary spinal cavernous angioma – case report. Neurol Med Chir (Tokyo) 1991; 31: 593–596.
Acciarri N, Padovani R, Pozzati E, Gaist G, Manetto V . Spinal cavernous angioma: a rare cause of subarachnoid hemorrhage. Surg Neurol 1992; 37: 453–456.
Sharma R, Rout D, Radhakrishnan VV . Intradural spinal cavernomas. Br J Neurosurg 1992; 6: 351–356.
Bruni P, Massari A, Greco R, Hernandez R, Oddi G, Chiappetta F . Subarachnoid hemorrhage from cavernous angioma of the cauda equina: case report. Surg Neurol 1994; 41: 226–229.
Cervoni L, Celli P, Gagliardi FM . Cavernous angioma of the cauda equina: report of two cases and review of the literature. Neurosurg Rev 1995; 18: 281–283.
Rao PG, Bhaskar G, Hemaratnan A, Srinivas TV . Spinal intradural extramedullary cavernous angiomas: report of four cases and review of the literature. Br J Neurosurg 1997; 11: 228–232.
Duke BJ, Levy AS, Lillehei KO . Cavernous angiomas of the cauda equina: case report and review of the literature. Surg Neurol 1998; 50: 442–445.
Nozaki K, Inomoto T, Takagi Y, Hashimoto N . Spinal intradural extramedullary cavernous angioma: case report. J Neurosurg Spine 2003; 99: 316–319.
Flavigna A, Righesso Neto O, dos Santos JA, Ferraz FA . Cavernous angioma of the cauda equina: case report. Arq Neuropsiquiatr 2004; 62: 531–534.
Hadlich R . Ein fall von Tumor Cavernosus des Rueckenmarks mit besonderer Beruecksichtigung der neueren Theorien ueber die Genesis des kavernom. Virchows Arch 1903; 172: 429–441.
Turner OA, Kernohan JW . Vascular malformation and vascular tumors involving the spinal cord. Arch Neurol 1941; 46: 444–463.
Wang AM, Morris JH, Fischer EG, Peterson R, Lin JCT . Cavernous hemangioma of the thoracic spinal cord. Neuroradiology 1988; 30: 261–264.
Rigamonti D, Drayer BP, Jhonson PC, Hadley MN, Zabramski J, Spetzler RF . The MRI appearance of cavernous malformations (angiomas). J Neurosurg 1987; 67: 518–524.
Fontaine S, Melanson D, Cosgrove R, Bertrand G . Cavernous hemangiomas of the spinal cord MR imaging. Radiology 1988; 166: 839–841.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Er, U., Yigitkanli, K., Simsek, S. et al. Spinal intradural extramedullary cavernous angioma: case report and review of the literature. Spinal Cord 45, 632–636 (2007). https://doi.org/10.1038/sj.sc.3101990
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101990
Keywords
This article is cited by
-
Extra-Axial Dural-Based Foramen Magnum Cavernous Malformation: a Rara Avis. Case Report and Literature Review
SN Comprehensive Clinical Medicine (2023)
-
Spinal intradural extramedullary cavernous hemangioma
Neuroradiology (2018)