Abstract
Objectives:
We evaluated the outcomes of augmentation ileocystoplasty in video-urodynamics (V-UDS) and questionnaires related to bowel and urinary function.
Methods:
In 22 meningomyelocele (MMC) patients (11 male and 11 female, a mean age at surgery 14.4 years) who underwent augmentation ileocystoplasties, V-UDS was performed before and at a median of 15 months (6–120 months) after the surgery and the questionnaires were answered at a median of 7.1 years (1.1–14.5 years) after surgery.
Results:
Concomitant procedures of urethral sling in four, cecostomy in four and ureteral reimplantation in two were performed at augmentation ileocystoplasty. V-UDS showed a significant improvement after the surgery in bladder capacity, bladder compliance and detrusor overactivity. Vesicoureteral reflux (VUR) disappeared after the surgery in 16 of 19 ureters with VUR. Although questionnaire for urinary condition using International Consultation on Incontinence Questionnaire–Short Form demonstrated that 80% of patients were completely free from urinary incontinence after surgery, more than a half of patients had persistent or deteriorated bowel function such as urgency of bowel movement and fecal incontinence in questionnaires for bowel function. Even with complaints in bowel function, more than 80% of MMC patients had a high level of satisfaction with augmentation enterocystoplasty in overall quality of life (QOL).
Conclusions:
Benefits of augmentation ileocystoplasty were maintained in urodynamic parameters as well as urinary continence. Although augmentation ileocystoplasty generally provides high QOL for MMC patients refractory to conservative therapies, an advance of fecal management can make MMC patients’ QOL superior to a current state.
Similar content being viewed by others

Introduction
Management of lower urinary tract function in meningomyelocele (MMC) patients aims at preventing urinary tract infection (UTI), preserving renal function and achieving socially acceptable continence. Since the introduction of clean intermittent catheterization (CIC) as a safe method of bladder emptying for patients with voiding dysfunction,1 a urinary management of MMC patients has been dramatically improved. Currently, many MMC patients, who perform CIC and take anticholinergic pharmacotherapy and intravesical injection of botulinum toxin2, 3 as conservative therapies, obtain low-pressure urinary storage with adequate capacity and socially acceptable continence between catheterization. However, a small group of MMC patients still remains refractory to conservative therapies, including maximal anticholinergic medication and others. In the cases refractory to conservative therapies, poor bladder compliance or detrusor overactivity usually causes persistent ureteral reflux or hydronephrosis, while urethral sphincter incompetence and poor bladder storage function lead to persistent urinary incontinence. Augmentation enterocystoplasty is a procedure suitable for these MMC patients in whom conservative medical therapies have failed.4, 5
Although many papers revealed excellent clinical results of augmentation enteroplasty in patients with neurogenic bladder refractory to conservative therapies,4, 5, 6, 7 there have been few studies describing urodynamic results of augmentation enterocystoplasty and long-term satisfaction with bowel and urinary condition at postsurgery. In fact, as augmentation enterocystoplasty involves the incorporation of a bowel segment into the bladder, MMC patients may suffer from unstable bowel function after the surgery despite of a significant improvement of urinary condition such as urinary incontinence and UTI.
In the present study, we evaluated outcomes of augmentation ileocystoplasty in video-urodynamics (V-UDS) and questionnaires related to bowel and urinary function.
Patients and methods
A total of 22 MMC patients (11 male and 11 female, a mean age at surgery 14.4 years), who underwent augmentation ileocystoplasty at Hokkaido University Hospital between April 1991 and December 2005, were enrolled in the study. A minimum follow-up of 1 year since bladder augmentation was necessary for patients to be included in the study.
The present study is designed in two parts. In the first part, a retrospective review of V-UDS at pre- and postsurgery was performed. Preoperative evaluation consisted of history and physical examination, voiding diary, laboratory studies, cystoscopy, upper urinary tract imaging including ultrasound or excretory urography and V-UDS. Postoperative evaluations were performed with urinalysis, ultrasonography and laboratory studies, and then V-UDS at postsurgery was basically scheduled at more than 6 months after the surgery and the most recent follow-up visit as necessary. The methods of urodynamics were referred to documents of international continence society.8 V-UDS consisted of simultaneous measurement of intravesical, intraabdominal and detrusor pressure, cystography and voiding cystourethrogram. Cystometry was accomplished with room temperature radiographic contrast material at a filling rate of 30–50 ml min−1.
In the second part, International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF) for urinary incontinence, questionnaires related to bowel function and questionnaire regarding quality of life (QOL) for augmentation ileocystoplasty were mailed after a recent follow-up. In ICIQ-SF, the three individual scores were analyzed in the study. Questionnaires for bowel function according to postoperative condition contained questions of (1) urgency of bowel movement, (2) frequency of bowel movement, (3) watery feces and (4) fecal incontinence, and then answers of (1) not at all, (2) slightly, (3) moderately, (4) a lot and (5) extremely for each question. We defined that answer described (3) moderately, (4) a lot and (5) extremely meant persistent or deteriorated bowel function after augmentation ileocystoplasty.
Augmentation ileocystoplasty was performed alone or in conjunction with continence or antireflux techniques. Methods of ileocystoplasty included techniques of Hautmann9 in 18 patients, Goodwin10 in 3 and hemi-Kock11 in 1. The length of the ileum dissected for the augmentation ileocystoplasty was approximately 40 cm in Hautmann, 20–30 cm in Goodwin and 55 cm in hemi-Kock. The terminal ileum at least 10 cm proximal to Bauhin's valve was preserved during dissection in all cases. In addition, two patients underwent a concomitant antireflux procedure with construction of a hemi-Kock afferent nipple valve with bilateral ureteroileal reimplantation in one and bilateral ureteroileal reimplantation in one documented high-grade vesicoureteral reflux (VUR). Urethral fascial sling as a concomitant continence procedure was performed in 10 patients, in whom preoperative V-UDS showed that abdominal leak point pressure (ALPP) was less than 90 cm H2O. Malone's appendicocecostomy procedure for antegrade colonic enema (MACE),12 which is used for colonic irrigations to manage fecal incontinence and constipation, was also performed in four patients.
Urodynamic parameters were presented as mean±standard deviation. Statistical analysis was performed using paired Student's t-test and Fisher's exact test. P-value less than 0.05 was considered significant.
Results
In 22 MMC patients, a median follow-up from augmentation ileocystoplasty was 5.2 years (1.1–17.5 years). Preoperative complications from medical charts were identified febrile UTI in 17 patients (77%) and urinary incontinence in 20 (91%). Postoperatively, bowel obstruction occurred in two patients (9%) and one of them undertook the surgical repair. There was no febrile UTI episode after augmentation ileocystoplasty and ultrasonography during follow-up showed no deterioration of hydronephrosis. One patient (5%) developed bladder stone, which was successfully extirpated with endoscopic surgery, while there was no complication of metabolic derangement or bladder perforation during follow-up.
V-UDS
Postoperative V-UDS was performed at a median of 15 months (6–120 months) after the surgery. The results of V-UDS at pre- and postaugmentation ileocystoplasty are summarized in Table 1. V-UDS showed a significant improvement after the surgery in bladder capacity, bladder compliance and detrusor overactivity. VUR disappeared after augmentation ileocystoplasty in 16 of 19 ureters (84%) with VUR preoperatively. Additionally other three ureters showed improvement of VUR after the surgery.
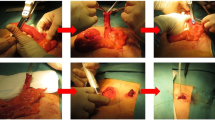
Figure 1 shows representative charts of V-UDS in a 14-year-old girl at pre- and postaugmentation ileocystoplasty. Preoperatively, cystography revealed that bladder deformity with bilateral high-grade VUR, and urodynamic parameters showed high detrusor pressure with low bladder compliance. This patient undertook augmentation ileocystoplasty alone. Postoperative V-UDS at 9 months revealed disappearance of VUR and improvement of urodynamic parameters.
Representative video-urodynamics (V-UDS) charts at (a) pre- and (b) postaugmentation ileocystoplasty. V-UDS at postaugmentation ileocystoplasty showed that disappearance of VUR and improvement of urodynamic parameters compared to preaugmentation ileocystoplasty. Pves, intravesical pressure; Pdet, detrusor pressure.
Questionnaire
The rate of questionnaire reply was 68% (15 of 22 patients) and these questionnaires were answered at a median of 7.1 years (1.1–14.5 years) after surgery.
Questionnaire for urinary condition using ICIQ-SF demonstrated that 80% of patients were completely free from urinary incontinence after surgery. In QOL regarding urinary incontinence, the section of ‘Impact’ revealed that more than 90% of patients were satisfied with urinary continence condition after the surgery (Figure 2).
Results of International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF) for urinary incontinence. ICIQ-SF demonstrated that 80% of patients were completely free from urinary incontinence after surgery. The section of ‘Impact’ for quality of life (QOL) regarding urinary incontinence revealed that more than 90% of patients were satisfied with continence condition after the surgery.
According to bowel function in symptoms of bowel movement, frequency bowel movement and fecal incontinence, only 20–27% of MMC patients did not have any complaints even after augmentation ileocystoplasty. However, 46–60% of MMC patients with augmentation ileocystoplasty had persistent or deteriorated bowel function, including urgency of bowel movement (53%), frequency bowel movement (46%) and fecal incontinence (60%). There was slightly less impact in watery feces after augmentation ileocystoplasty compared to other bowel symptoms (Figure 3).
Results of questionnaire for bowel function. Many meningomyelocele (MMC) patients with augmentation ileocystoplasty had persistent or deteriorated bowel function, including (a) urgency of bowel movement (53%), (b) frequency of bowel movement (46%), (c) watery feces (39%) and (d) fecal incontinence (60%).
Even with complaints in bowel function, more than 80% of MMC patients had a high level of satisfaction with augmentation enterocystoplasty in overall QOL (Figure 4).
Discussion
We evaluated outcome of augmentation ileocystoplasty in V-UDS and long-term outcome of questionnaires related to bowel and urinary function in the present study. Augmentation ileocystoplasty was effective in V-UDS, including a significant improvement in bladder capacity, bladder compliance and detrusor overactivity as well as disappearance of VUR even without ureteral reimplantation. Questionnaire revealed that more than 90% of MMC patients were postoperatively satisfied with urinary continence with long-term follow-up, while 39–60% of MMC patients with augmentation ileocystoplasty had urgency of bowel movement, frequency bowel movement and fecal incontinence. Despite complaints of bowel function, however, augmentation ileocystoplasty generally provides high QOL for MMC patients refractory to conservative therapies. Based on the present study, we believe that an advance of fecal management can make MMC patients’ QOL superior to a current state.
The goal of treatment neurogenic bladder is to prevent upper urinary tract deterioration and improve urinary incontinence. Along with wide acceptance of CIC as a safe and reliable method of urinary management for voiding disturbance,1 the treatments of MMC patients have been improved and urodynamics has been performed to detect the incidence of a high risk of upper urinary deterioration. In fact, vesical leak point pressure of more than 40 cm H2O,13 maximal urethral closure pressure of more than 50 cm H2O,14 and the presence of detrusor-sphincter dyssynergia15 have been important risk factors for upper urinary deterioration in MMC patients. In the MMC patients with these prognostically unfavorable patterns, we usually introduce early treatment of CIC and anticholinergics to prevent upper urinary deterioration, as well as to achieve urinary continence. However, some MMC patients refractory to conservative therapies require bladder augmentation because of upper urinary deterioration and unacceptable urinary incontinence. Many papers reported that augmentation enterocystoplasty provides benefits of urodynamic parameters in patients with neurogenic bladder.4, 5, 7 In the present study, postoperative V-UDS showed a significant improvement after the surgery in bladder capacity, bladder compliance and detrusor overactivity. In addition, preoperative VUR were resolved or improved in all, and none had febrile UTI after the augmentation cystoplasty.
In the present study, V-UDS was performed just in a median of 15 months after the surgery, which was much shorter than follow-up period (vs a median follow-up of 5.2 years). In regular follow-up, urinalysis, ultrasonography and laboratory studies were evaluated, and we previously confirmed that we usually did not have significant changes in V-UDS during long-term follow-up after augmentation enterocystoplasty, unless MMC patients had febrile UTIs, changes of urinary incontinence or changes of the upper urinary tracts or the bladder in ultrasonography. That is why regular V-UDS is not performed at our hospital during long-term follow-up after confirming a significant improvement in V-UDS at around 1 year after the surgery, unless significant clinical episodes happen.
Ureteral implantation is not performed routinely as a concomitant procedure of augmentation ileocystoplasty at our hospital, because we believe that VUR in MMC patients is basically associated with high detrusor pressure and VUR will resolve by a decrease of detrusor pressure. In fact, according to VUR observed in 19 ureters of 44 preoperatively, VUR in 16 ureters disappeared after augmentation ileocystoplasty, although ureteral implantation was performed in only 4 ureters of two patients. This result is compatible with the previously reported result, which showed that bladder augmentation alone should provide complete reflux resolution in most cases of neurogenic bladder.16 Thus, ureteral implantation may not be necessary as a concomitant procedure in bladder augmentation. However, we need further investigation whether ureteral implantation should be done as concomitant procedure of augmentation enterocystoplasty, because life-long influence of the persisted VUR has not been known yet.
According to treatment of urinary incontinence, a fascial sling procedure is performed in principle as a concomitant procedure for MMC patients at our hospital, if ALPP is less than 90 cm H2O. Since some MMC patients have urethral sphincter incompetence as well as detrusor overactivity, urodynamics is very important examination before augmentation enterocystoplasty. Actually, postoperative ICIQ-SF demonstrated that 80% of patients were completely free from urinary incontinence after the surgery, and more than 90% of patients were satisfied with continence condition after the surgery.
Since most MMC patients also have some symptoms of bowel dysfunction, the questions of whether augmentation ileocystoplasty affects bowel habits are important for MMC patients with augmentation ileocystoplasty. It has been reported that patients who underwent enterocystoplasty had some symptoms of subsequent bowel function, and worsening bowel dysfunction was one of major complications of augmentation ileocytoplasty, which was associated with poor patient's satisfaction.17, 18, 19 This study has the limitations because preoperative bowel symptoms had not been assessed with the same questionnaire as used in the present study. However, this study revealed that 39–60% of MMC patients actually had significant bowel dysfunction after augmentation ileocystoplasty. Although more than 80% of MMC patients still had a high level of satisfaction with augmentation ileocystoplasty in overall QOL, we should consider again a management of bowel dysfunction associated with resection of the distal ileum, because most bile acids are absorbed by an active process in the distal ileum. Underlying mechanisms of chronic diarrhea and fecal urgency after ileal neobladder are believed to be due to decreasing bile acids absorption.20 Bowel dysfunction after distal ileum resection is caused by cathartic actions of bile acids in the colon as they inhibit sodium reabsorption, resulting in increased water loss. Preservation of the terminal ileum, which may be more than 15 cm in length proximal to Bauhin's valve during dissection, and less length of the dissected ileal segment could be important to reduce the incidence of bowel dysfunction. It also has been reported that preoperative screening with 23-selena 25 homotaurocholic acid may be useful to predict patients at increased risk for postoperative bile acids diarrhea.20 At follow-up period after the surgery, cholestyramine, which can be bind to bile acids in the colon, was introduced as a useful drug to relieve bile acid chronic diarrhea.
MACE procedure was introduced for one of the treatments for bowel dysfunction and many excellent results were reported.12, 21, 22 In the present study, although MACE procedure was performed in four patients as concomitant surgery of augmentation ileocystoplasty, questionnaire for bowel symptoms and QOL showed MACE procedure unfortunately had no benefit compared to patients without MACE procedure. This result may be implicated in small number of patients in the present study. Further study is necessary to evaluate the impact of MACE for bowel symptoms and patients’ QOL.
In conclusion, the present study revealed that benefits of augmentation ileocystoplasty were maintained in urodynamic parameters with a median follow-up of 15 months as well as urinary continence with a median follow-up of 7.1 years. Although augmentation ileocystoplasty generally provides high QOL for MMC patients refractory to conservative therapies, 39–60% of MMC patients with augmentation ileocystoplasty had urgency of bowel movement, frequency bowel movement and fecal incontinence. We believe that an advance of fecal management can make MMC patients’ QOL superior to a current state.
References
Lapides J, Diokno AC, Silber SJ, Lowe BS . Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol 1972; 107: 458–461.
Altaweel W, Jednack R, Bilodeau C, Corcos J . Repeated intradetrusor botulinum toxin type A in children with neurogenic bladder due to myelomeningocele. J Urol 2006; 175: 1102–1105.
Riccabona M, Koen M, Schindler M, Goedele B, Pycha A, Lusuardi L et al. Botulinum-A toxin injection into the detrusor: a safe alternative in the treatment of children with myelomeningocele with detrusor hyperreflexia. J Urol 2004; 171: 845–848; discussion 848.
Quek ML, Ginsberg DA . Long-term urodynamics followup of bladder augmentation for neurogenic bladder. J Urol 2003; 169: 195–198.
Blaivas JG, Weiss JP, Desai P, Flisser AJ, Stember DS, Stahl PJ . Long-term followup of augmentation enterocystoplasty and continent diversion in patients with benign disease. J Urol 2005; 173: 1631–1634.
Venn SN, Mundy AR . Long-term results of augmentation cystoplasty. Eur Urol 1998; 34 (Suppl 1): 40–42.
Chartier-Kastler EJ, Mongiat-Artus P, Bitker MO, Chancellor MB, Richard F, Denys P . Long-term results of augmentation cystoplasty in spinal cord injury patients. Spinal Cord 2000; 38: 490–494.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002; 21: 167–178.
Frohneberg D, Bachor R, Egghart G, Miller K, Hautmann R . Ileal neobladder. Principles of function and continence. Eur Urol 1989; 16: 241–249.
Goodwin WE, Winter CC, Barker WF . Cup-patch technique of ileocystoplasty for bladder enlargement or partial substitution. Surg Gynecol Obstet 1959; 108: 240–244.
Weinberg AC, Boyd SD, Lieskovsky G, Ahlering TE, Skinner DG . The hemi-Kock augmentation ileocystoplasty: a low pressure anti-refluxing system. J Urol 1988; 140: 1380–1384.
Malone PS, Ransley PG, Kiely EM . Preliminary report: the antegrade continence enema. Lancet 1990; 336: 1217–1218.
McGuire EJ, Woodside JR, Borden TA, Weiss RM . Prognostic value of urodynamic testing in myelodysplastic patients. J Urol 1981; 126: 205–209.
Kobayashi S, Shinno Y, Kakizaki H, Matsumura K, Koyanagi T . Relevance of detrusor hyperreflexia, vesical compliance and urethral pressure to the occurrence of vesicoureteral reflux in myelodysplastic patients. J Urol 1992; 147: 413–415.
Bauer SB, Hallett M, Khoshbin S, Lebowitz RL, Winston KR, Gibson S et al. Predictive value of urodynamic evaluation in newborns with myelodysplasia. JAMA 1984; 252: 650–652.
Lopez Pereira P, Martinez Urrutia MJ, Lobato Romera R, Jaureguizar E . Should we treat vesicoureteral reflux in patients who simultaneously undergo bladder augmentation for neuropathic bladder? J Urol 2001; 165: 2259–2261.
Somani BK, Kumar V, Wong S, Pickard R, Ramsay C, Nabi G et al. Bowel dysfunction after transposition of intestinal segments into the urinary tract: 8-year prospective cohort study. J Urol 2007; 177: 1793–1798.
N’Dow J, Leung HY, Marshall C, Neal DE . Bowel dysfunction after bladder reconstruction. J Urol 1998; 159: 1470–1474;discussion 1474–1475.
Singh G, Thomas DG . Bowel problems after enterocystoplasty. Br J Urol 1997; 79: 328–332.
Thorstenson A, Jacobsson H, Onelov E, Holst JJ, Hellstrom PM, Kinn AC . Gastrointestinal function and metabolic control after construction of an orthotopic ileal neobladder in bladder cancer. Scand J Urol Nephrol 2007; 41: 14–19.
Lefevre JH, Parc Y, Giraudo G, Bell S, Parc R, Tiret E . Outcome of antegrade continence enema procedures for faecal incontinence in adults. Br J Surg 2006; 93: 1265–1269.
Yerkes EB, Cain MP, King S, Brei T, Kaefer M, Casale AJ et al. The Malone antegrade continence enema procedure: quality of life and family perspective. J Urol 2003; 169: 320–323.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mitsui, T., Tanaka, H., Moriya, K. et al. Outcomes of lower urinary and bowel function in meningomyelocele patients with augmentation enterocystoplasty. Spinal Cord 46, 432–437 (2008). https://doi.org/10.1038/sj.sc.3102164
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102164
Keywords
This article is cited by
-
Impact of posterior urethral diameter/external urethral sphincter diameter as a new tool to predict detrusor pressure in the voiding phase
International Urology and Nephrology (2018)
-
Neurogene Blasenfunktionsstörungen bei Patienten mit Meningomyelozele
Der Urologe (2015)
-
Evaluation and Management of Failed Bladder Augment
Current Bladder Dysfunction Reports (2012)