Abstract
Current data on the concordance of KRAS, BRAF, PIK3CA mutation status or PTEN expression status between primary tumors and metastases in colorectal cancer (CRC) are conflicting. We conducted a systematic review and meta-analysis to examine concordance and discordance of the status of these four biomarkers between primary tumors and corresponding metastases in CRC patients. The biomarker status in primary tumors was used as the reference standard. Concordance data for KRAS, BRAF, PIK3CA and PTEN were provided by 43, 16, 9 and 7 studies, respectively. The pooled concordance rate was 92.0% (95% CI: 89.7%–93.9%) for KRAS, 96.8% (95% CI: 94.8%–98.0%) for BRAF, 93.9% (95% CI: 89.7%–96.5%) for PIK3CA and 71.7% (95% CI: 57.6%–82.5%) for PTEN. The pooled false positive and false negative rates for KRAS were 9.0% (95% CI: 6.5%–12.4%) and 11.3% (95% CI: 8.0%–15.8%), respectively. KRAS, BRAF and PIK3CA mutations are highly concordant between primary tumors and corresponding metastases in CRC, but PTEN loss is not. Nine percent of patients with wild-type KRAS in primary tumors who received anti-EGFR treatment had mutant KRAS in metastases, while 11.3% patients with mutant KRAS primary tumors had wild-type KRAS in the metastases. These 11.3% patients currently do not receive potentially beneficial anti-EGFR treatment.
Similar content being viewed by others
Introduction
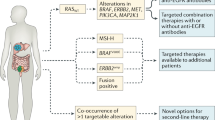
The Epidermal Growth Factor Receptor (EGFR) is a cell transmembrane tyrosine kinase receptor that has a role in cancer cell proliferation and survival. Monoclonal antibodies (MoAbs) that target and inhibit EGFR function are commonly used in colorectal cancer treatment1. Two such MoAbs that target the extracellular domain of EGFR are cetuximab and panitumumab and these have proved effective in combination with chemotherapy or as single agents against metastatic colorectal cancer (mCRC)1. Unfortunately, resistance to MoAb treatment is common and in a recent study only 10–20% of the unselected mCRC patients benefitted from the treatment1. The resistance is partly ascribed to oncogenic activations of intracellular signaling pathways downstream of EGFR, including the RAS/RAF/MAPK and PI3K/PTEN/AKT pathways1. In the RAS/RAF/MAPK pathway, KRAS or BRAF mutations are present in 35–45% and in 4–15% of mCRC, respectively2. In the PI3K/PTEN/AKT pathway, PIK3CA mutations and loss of PTEN expression occur in 10–18% and 19–42% of mCRC, respectively2. PIK3CA mutations may coexist with either KRAS or BRAF mutations within the same tumor2, whereas mutations in KRAS and BRAF appear to be mutually exclusive3.
To date, KRAS codon 12 or 13 mutations in exon 2 have been widely demonstrated as a major predictive biomarker for resistance to the anti-EGFR MoAb treatment in patients with mCRC. Patients with mutant KRAS mCRC demonstrate lower objective response rates, decreased progression-free survival and worse overall survival compared with patients with wild-type KRAS mCRC4. With reference to these findings, the European Medicines Agency and subsequently the US Food and Drug Administration have restricted the use of anti-EGFR MoAbs to patients with wild-type KRAS mCRC. However, the occurrence of KRAS mutations only accounts for approximately 30–40% of nonresponsive patients4. In patients with wild-type KRAS mCRC, it remains unclear why a large number of patients are still not responsive to the treatment. The study by Douillard et al5 suggested that RAS mutations (KRAS and NRAS), in addition to KRAS exon 2 mutations, may be a reason why some patients without KRAS exon 2 mutations are not responsive to anti-EGFR MoAbs treatment. Recently, other oncogenic mutations, such as BRAF6,7, PIK3CA mutations6 and loss of PTEN expression7, have been presented as promising predictors for treatment resistance in these patients, although their predictive value has not yet been established. An additional explanation for the resistance to anti-EGFR MoAbs in patients with wild-type KRAS mCRC is discordance of KRAS mutation status between primary tumors and corresponding metastases. Crucially, this suggests that selecting patients for anti-EGFR MoAb treatment based on the characteristics of the primary tumor and not their metastases may not be optimal.
Current data on the concordance of KRAS, BRAF, PIK3CA mutation status and PTEN expression status between primary tumors and metastases are conflicting. Take KRAS mutations as an example, some studies8,9,10 showed 100% concordance between primary CRC tumors and corresponding metastases. In contrast to these data, others have reported 4–30% discordance11,12,13,14. These inconsistent results between studies probably reflect the heterogeneity in methods, sample sizes, technical skills, the wide variety of metastatic sites or tumor biology (i.e., the genetic heterogeneity of the tumor cell population in the primary tumor, or changes in mutation status during progression of CRC). Therefore, it is still uncertain whether KRAS mutation status in primary tumor correctly reflects the KRAS mutation status of corresponding metastases. It also raises the question of whether mutation status of the primary tumor is sufficient to predict the response to anti-EGFR MoAbs.
In the present study, we performed a systematic review and meta-analysis to examine the overall concordance and discordance rates of the KRAS, BRAF, PIK3CA mutations status and PTEN expression status between primary CRC tumors and corresponding metastases.
Results
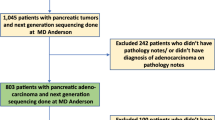
Literature search results
A total of 2096 records were retrieved from MEDLINE and EMBASE databases. After excluding duplicates and screening of titles and abstracts, 65 citations were left for full text screening. Among these 21 were excluded according to inclusion criteria, leaving 44 relevant articles. Searching of ASCO did not identify any further eligible studies, while reference list checking of reviews and included studies identified 2 additional studies. In total, 46 relevant studies4,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51 were identified. Details are presented in figure 1.
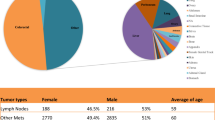
Mutation status concordance was reported in 43 studies for KRAS4,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51, in 16 studies for BRAF7,13,14,15,16,17,18,24,25,26,27,33,34,41,43,48, in 9 studies for PIK3CA13,14,15,18,25,27,34,48,49 and in 8 studies for PTEN7,13,17,31,32,34,47,48. The majority of studies (40/43) tested the KRAS mutations on codons 12 and 134,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,27,29,30,34,35,36,37,38,39,41,42,43,44,45,46,47,48,49,50,51. Eight of 16 studies tested the BRAF mutations on exon 157,13,14,17,18,33,34,41 and 5 of 9 studies tested the PIK3CA mutations on exon 9 and/or exon 2013,14,18,25,34. Seven studies reported concordance information for lymph node metastases7,14,26,28,36,37,49 and 11 studies for liver metastases9,10,11,12,27,29,37,38,42,48,49. Details are shown in Table 1 (Appendix 1).
Methodological quality of included studies
The reporting quality score of included studies varied considerably, from 6 to 21 of a maximum score of 22 using STROBE criteria. Considering methodological quality, all the included studies were identified as being of good quality in terms of the reference standard that was selected; and in terms of keeping all the patients received the same standard. Case-control study design was avoided in 42 studies4,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,36,37,38,39,41,42,43,46,47,48,49,50,51 while the study design was unclear or not reported in the remaining 4 studies35,40,44,45. Only 2 studies7,37 (2/46) reported assessor blinding, whereas the rest4,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,38,39,40,41,42,43,44,45,46,47,48,49,50,51 did not explicitly reported whether test readers were blinded or not. One study12 (1/46) had pre-specified threshold for KRAS mutations. In total, 27 out of the 46 included studies fulfilled 6 or more of the 11 methodological quality items7,8,9,10,11,12,13,14,16,17,18,19,20,21,23,25,27,29,34,36,37,41,42,48,49,50,51.
Concordance and discordance between primary tumors and corresponding metastases
The pooled rates of mutation presence did not differ significantly between primary tumors and corresponding metastases for KRAS mutations (40.3%, 95% CI: 37.0%–43.8% vs. 39.9%, 95% CI: 36.5%–43.4%; p = 0.330), BRAF mutations (6.1%, 95% CI: 4.0%–9.4% vs. 5.7%, 95% CI: 3.4%–9.3%; p = 0.362), PIK3CA mutations (13.5%, 95% CI: 9.3%–19.2% vs. 13.8%, 95% CI: 9.8%–19.1%; p = 0.392) and loss of PTEN expression (41.0%, 95% CI: 26.7%–61.3% vs. 57.0%, 95% CI: 33.6%–66.8%; p = 0.373).
The pooled concordance rate was 92.0% (95% CI: 89.7%–93.9%) for KRAS (Appendix 2), 96.8% (95% CI: 94.8%–98.0%) for BRAF (Appendix 3), 93.9% (95% CI: 89.7%–96.5%) for PIK3CA (Appendix 4) and 71.7% (95% CI: 57.6%–82.5%) for PTEN (Appendix 5) (Table 2). When we just focused on KRAS codon 12 and 13 mutation status, the pooled concordance was 92.0% (30 studies, 1760 pairs; 95% CI: 88.5%–94.5%; I2 = 41.9%).
The pooled false positive and false negative rates were 9.0% (95% CI: 6.5%–12.4%) and 11.3% (95% CI: 8.0%–15.8%) for KRAS (Figure 2), 5.9% (95% CI: 3.5%–9.8%) and 34.0% (95% CI: 17.5%–55.7%) for BRAF, 9.1% (95% CI: 5.4%–16.8%) and 25.2% (95% CI: 13.5%–42.0%) for PIK3CA and 26.0% (95% CI: 4.2%–73.9%) and 16.3% (95% CI: 8.4%–29.4%) for PTEN (Table 2).
For KRAS, we further explored the mutational details in individual cases of discordance, where this had been reported. Ten studies7,12,13,15,16,20,24,25,26,27,48,51 provided KRAS mutational information on a total of 57 discordant cases including 19 with wild-type KRAS in primary tumor but mutant KRAS in their metastases, 31 cases with mutant KRAS in primary tumors but wild-type KRAS in their metastases and the rest (7 cases) showed a different mutation sub-type between the primary tumor and metastases. The most common mutation in primary tumor and metastases were G13D (7/38) and G12D (9/26), respectively. Details are presented in Figure 3.
Subgroup analyses according to metastases sites and testing methods
Subgroup analyses according to the site of metastases or testing methods were performed for concordance of KRAS, BRAF and PIK3CA status (Table 3). The pooled concordance of the genetic mutation or expression status in liver or lymph node metastases and primary CRC was 93.0% (95% CI: 87.4%–96.3%) and 73.4% (95% CI: 65.1%–80.3%) for KRAS, 98.6% (95% CI: 91.0%–99.8%) and 93.6% (95% CI: 86.0%–97.2%) for BRAF, 97.7% (95% CI: 72.3%–99.9%) and 85.5% (95% CI: 73.5%–92.6%) for PIK3CA.
The pooled concordance of KRAS status was 81.1% (95% CI: 69.3%–89.1%) for AS-PCR, 91.6% (95% CI: 89.0%–93.5%) for sequencing, 91.6% (95% CI: 25.0%–99.7%) for SSCP, 92.5% (95% CI: 72.0%–98.3%) for ASO and 97.3% (95% CI: 87.4%–99.4%) for PCR-RFLP. The pooled concordance of BRAF status was 97.4% (95% CI: 95.8%–98.3%) for sequencing and 93.0% (95% CI: 80.5%–97.7%) for AS-PCR (Table 3). The pooled concordance of PIK3CA status was 94.0% (95% CI: 86.3%–97.5%) for sequencing and 95.9% (95% CI: 89.5%–98.4%) for SSCP.
Discordance of KRAS status was also explored through subgroup analysis of metastasis location. The pooled false positive and false negative rates were 8.0% (9 studies, 408 pairs; 95% CI: 3.2%–18.4%; I2 = 40.3%) and 9.7% (95% CI: 4.5%–19.5%; I2 = 35.0%) for liver metastases and 24.6% (6 studies, 78 pairs; 95% CI: 10.1%–48.7%; I2 = 38.2%) and 25.5% (6 studies, 91 pairs; 95% CI: 10.8%–49.4%; I2 = 40.7%) for lymph node metastases.
Sensitivity analysis and publication bias
Robust pooled results for KRAS, BRAF, PIK3CA and PTEN concordance (Table 4) were shown in sensitivity analyses when excluding studies that collected tissue after the initiation of chemo-therapy, studies fulfilling less than 6 of the 11 methodological quality criteria, studies with sample-size less than 50 and studies reporting concomitant KRAS and BRAF mutations. Significant publication bias was observed among studies for KRAS concordance (z = −9.64, p < 0.001), while no publication bias was observed among studies for BRAF (z = −3.53, p > 0.1), PIK3CA (z = −1.55, p > 0.1) or loss of PTEN expression (z = −1.43, p > 0.1).
Discussion
In clinical practice, analysis of KRAS mutations are usually performed on the primary tumor to determine patient eligibility for anti-EGFR MoAbs treatment, often because tissue samples from the metastasis is not available. However, current data on the concordance of KRAS mutation status between primary tumors and corresponding metastases are conflicting. Therefore, the question of whether KRAS mutation status of the primary tumor is sufficient to predict the response to anti-EGFR MoAbs has been a controversial issue to date. In the present study, we performed a systematic review and meta-analysis to examine the overall concordance and discordance rates of KRAS and three other promising predictive biomarkers (BRAF, PIK3CA mutations and PTEN expression) between primary tumors and corresponding metastases. We found that the frequency of KRAS, BRAF, PIK3CA mutations and loss of PTEN expression did not differ significantly between primary tumors and corresponding metastases. Additionally, analysis of matched primary tumors and metastases showed a high concordance rate for KRAS (92.0%), BRAF (96.8%) and PIK3CA mutations (93.9%) but not for loss of PTEN expression (71.7%).
Although high concordance of KRAS status was observed between primary tumors and their metastases, discordance is still a concern, occurring in 9.0% of wild -type primary tumors and 11.3% in mutant primary tumors. Essentially, 9.0% of patients with wild-type KRAS primary tumors who receive the anti-EGFR MoAbs treatment actually have mutated KRAS in the metastases and 11.3% of patients with mutant KRAS primary tumors who have wild-type KRAS in the metastases will not receive potentially beneficial treatment. Most previous studies examined KRAS mutational status in only a single corresponding metastatic site. The representativeness of KRAS mutational status detected in only a single corresponding metastasis in the discordance cases is questionable52. Insufficient published data made it impossible to explore this question here.
In addition to KRAS, discordance rates of BRAF, PIK3CA mutation status and PTEN expression status were also analyzed. The status of these three biomarkers is not currently considered in clinical practice but given the higher concordance rate and lower rate of false positives for BRAF compared to KRAS, even though the rate of false negatives was higher, perhaps it is worth considering whether other biomarkers can be incorporated into the clinical decision making process.
Data for KRAS, BRAF and PIK3CA concordance were available for us to perform subgroup analyses according to metastases sites (liver or lymph nodes). A high concordance rate was observed between primary tumors and liver metastases for these three biomarkers. However, the concordance rate in lymph node metastases was notably lower, especially for KRAS or PIK3CA mutations, in addition to BRAF which had slightly poorer concordance in lymph node compared to liver metastases. This potentially indicates that lymph node metastases are unsuitable for genetic mutation analysis. Our pooled results are in line with Bass and colleagues' narrative review of this topic52.
Variation of the accuracy among different testing methods may be another reason for the discordance. Subgroup analyses based on testing methods for KRAS, BRAF and PIK3CA mutations showed that concordance varied among different testing methods. The most widely used method among included studies was sequencing, which is a classic method and has proven to be a reliable method. Results from this study showed that concordance for KRAS, BRAF and PIK3CA from sequencing were similar to their respective overall concordance, which suggested that sequencing was a stable method in testing mutations status of these three biomarkers or reflects the great contribution that sequencing makes to the total as it was the most frequently used method. Results from KRAS and PIK3CA suggested that SSCP may also a stable test method. However, AS-PCR showed the lowest concordance for both KRAS and BRAF. Interestingly, PCR-RFLP assessment showed the highest concordance (97.3%) for KRAS status (n = 2 studies). Poor quality of testing methods may contribute somewhat to discordance in our results, however they are unlikely to explain all heterogeneity.
In addition to metastasis location or gene mutation testing methods, other potential explanations for discordance exist. Improper tumor sampling may cause a high proportion of normal cells or necrotic tissue to be included4, tumor cells may have departed from the primary tumor before the acquisition of KRAS mutations or heterogeneity of cell type and therefore of biomarker status may exist in the primary tumor. The initiation of anti-EGFR MoAb treatment could also induce novel mutations and cause discordance53. As information on these factors were not available, sensitively analysis was performed based on the time of tissue collection (before or after MoAb treatment), study quality, sample size and whether there were concomitant mutations of KRAS and BRAF. Subgroup results varied little from the main pooled concordance estimates where more than four studies were available to pool. The exception being for PTEN with approximately 10% higher concordance reported in studies of better methodological quality compared to the main pooled result.
A key limitation in this work is the inability to generalize findings to other sites of metastasis because very few studies reported subgroup information on concordance between primary tumor and lung or brain metastases. Another limitation of our findings relates to mutational subgroups of PTEN expression or genetic mutations of BRAF or PIK3CA. Limited studies, compared KRAS mutational status, which prevented subgroup analysis for these. Furthermore, we identified significant publication bias for studies reporting KRAS concordance, indicating that the concordance values may not be as high as suggested by the studies here.
At present only the mutational status of KRAS is used as a predictive marker for EGFR inhibitor therapy52. Our results show good concordance between KRAS status in primary tumors and metastases indicating that the majority of patients will receive appropriate treatment. However, cases of discordance do clearly occur and are not uncommon and patients may therefore not be receiving the best or most appropriate treatment. The narrative review by Baas and colleagues suggested that discordance was uncommon and that additional testing is not justified, where no tissue already exists for the metastasis, because of increased risk of infection, increased costs of additional testing and the fact that the mutation status of one metastasis is no guarantee for the status of other tumors52. Despite the validity of these comments, the number of patients potentially affected by this issue is not insignificant at approximately 10% of those with CRC metastases. As with many issues in medicine, we must find a balance between the burden on patients or potential risk of further testing and the number of potential false positives.
In conclusion, high concordance rates were observed in KRAS, BRAF and PIK3CA mutation status but not in PTEN expression status between primary tumors and corresponding metastases. Liver metastases had a high concordance with primary tumor for KRAS, BRAF and PIK3CA mutation status while lymph node metastases showed a low concordance rate for these three biomarkers. Mutation concordance values were comparable with sequencing, SSCP, ASO and PCR-RFLP, indicating stability, while AS-PCR may be less reliable in this context.
Despite high concordance, discordance rates were not negligible for the four biomarkers examined. Future clinical decisions will need to consider that 9.0% of patients with wild-type KRAS primary tumors who currently receive the anti-EGFR MoAbs treatment have mutated KRAS in the metastases and 11.3% patients with mutant KRAS primary tumors who actually have wild-type KRAS in the metastases and currently do not receive anti-EGFR treatment. As yet, it is unclear whether to recommend testing for other mutations or change of policy on treatment allocation. Comprehensive studies are required to address the issue of concordance and weigh up all the potential harms and benefits to patients of additional biopsy testing and anti-EGFR treatment, or not, in respect of metastatic gene mutation status.
Methods
Search strategy and selection criteria
We conducted an electronic literature search of PubMed and EMBASE from their respective inception to October 2014, with different combinations of the following keywords: “colon cancer”, “rectal cancer”, “colorectal cancer”, “CRC”, “primary”, “KRAS”, “BRAF”, “PIK3CA” and “PTEN”. In addition, we searched the abstract database of American Society of Clinical Oncology (ASCO) by using the previously mentioned terms. We subsequently manually searched the bibliographies of included studies and recent narrative reviews for additional studies. We applied no language restrictions. We considered both published and unpublished studies for inclusion, including those published in abstract form only.
We included all studies that reported concordance of any one of KRAS, BRAF, PIK3CA mutation status or PTEN expression status in primary tumors and corresponding metastases in colorectal cancer. Two reviewers (WXY & YZY) independently reviewed titles, abstracts and full texts of all citations that were likely to meet the predefined selection criteria. Any discrepancies were resolved by consensus or by consulting with a third reviewer. For multiple publications from the same study, we selected the most recent and complete versions of studies.
Quality assessment and data extraction
Two reviewers (WXY & YJQ) independently extracted data using a predefined data abstraction form and critiqued the quality of the studies, with a third reviewer (MC) consulted in case of disagreement. For each study and for each of the four biomarkers, where reported, we constructed 2 × 2 tables to display the number of patients with mutations or normal/wild-type tumors present during assessment of primary or metastatic cancer. Thus, we could examine the proportion of cases where the genetic profile had changed from mutated to wild-type or vice-versa. In addition, the following data were extracted from each study: study characteristics (such as first author's name, year of publication, study design and number of patients enrolled), patients' characteristics (such as mean or median age, percent of male participants and histology), sites of metastases for biomarker testing, biomarker testing method and items necessary to assess study quality.
We assessed the methodological and reporting quality of studies by using the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool54 and the criteria for reporting observational studies proposed in the STROBE statement55, respectively, giving equal weight to all items.
Statistical analysis
We used the biomarker status in primary tumors as the reference standard and calculated agreement rate, false positive rate (wild-type or normal expression in primary tumor but mutant or loss of expression in metastases) and false negative rate (mutant or loss of expression in primary tumor but wild-type or normal expression in metastases) for each study using the above-mentioned 2 × 2 tables. The concordance was measured by agreement rate and discordance was measured by false positive rate or false negative rate. We combined rates of mutation/loss of expression, concordance and discordance using the fixed-effect model unless there was evidence of heterogeneity (p ≤ 0.1), in which case a random-effect model was used. Heterogeneity was explored by the Q-test with degree of freedom equal to the number of analyzed studies minus 1. A p value of 0.10 or below in the Q-test indicates the presence of heterogeneity across studies. We performed subgroup analyses to detect potential sources of heterogeneity according to metastases site (liver or lymph nodes) and methods used to test biomarker mutation (sequencing, allele-specific oligonucleotide hybridization [ASO], allele-specific polymerase chain reaction [AS-PCR], single-strand conformation polymorphism [SSCP], PCR-restriction fragment length polymorphism [PCR-RFLP] and other methods). For KRAS status, we also pooled the concordance of mutations on codons 12 and 13. We performed sensitivity analyses to assess the robustness of the final results by excluding studies that collected tumor tissue after the initiation of chemo-therapy, studies fulfilling less than 6 of the 11 methodological items, studies with sample-size less than 50 and studies reporting concomitant KRAS and BRAF mutations in samples of either primary tumors or metastases. We performed Egger's funnel plots to assess the possible presence of publication bias. Egger's test was performed to assess the symmetry of the funnel plot. We used STATA Version 12.0 (STATA Corporation, College Station, TX, USA) and MetaAnalyst Version Beta 3.13 (Tufts Medical Center, Boston, MA, USA) for the analyses, with a two-tailed significance level of 0.05 except for the assessment of heterogeneity (α = 0.10).
References
Van Cutsem, E. et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med 360, 1408–1417, 10.1056/NEJMoa0805019 (2009).
Bardelli, A. & Siena, S. Molecular mechanisms of resistance to cetuximab and panitumumab in colorectal cancer. J Clin Oncol 28, 1254–1261, 10.1200/jco.2009.24.6116 (2010).
Rajagopalan, H. et al. Tumorigenesis: RAF/RAS oncogenes and mismatch-repair status. Nature 418, 934, 10.1038/418934a (2002).
Garm Spindler, K. L. et al. The importance of KRAS mutations and EGF61A>G polymorphism to the effect of cetuximab and irinotecan in metastatic colorectal cancer. Ann Oncol 20, 879–884, 10.1093/annonc/mdn712 (2009).
Douillard, J. Y. et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med 369, 1023–34, 10.1056/NEJMoa1305275 (2013).
Moroni, M. et al. Gene copy number for epidermal growth factor receptor (EGFR) and clinical response to antiEGFR treatment in colorectal cancer: a cohort study. Lancet Oncol 6, 279–286, doi:http://dx.doi.org/10.1016/S1470-2045(05)70102-9 (2005).
Molinari, F. et al. Differing deregulation of EGFR and downstream proteins in primary colorectal cancer and related metastatic sites may be clinically relevant. Br J Cancer 100, 1087–1094, 10.1038/sj.bjc.6604848 (2009).
Zauber, P., Sabbath-Solitare, M., Marotta, S. P. & Bishop, D. T. Molecular changes in the Ki-ras and APC genes in primary colorectal carcinoma and synchronous metastases compared with the findings in accompanying adenomas. Mol Pathol 56, 137–140, 10.1136/mp.56.3.137 (2003).
Weber, J. C. et al. Allelotyping analyses of synchronous primary and metastasis CIN colon cancers identified different subtypes. Int J Cancer 120, 524–532, 10.1002/ijc.22343 (2007).
Etienne-Grimaldi, M. C. et al. K-Ras mutations and treatment outcome in colorectal cancer patients receiving exclusive fluoropyrimidine therapy. Clin Cancer Res 14, 4830–4835, 10.1158/1078-0432.ccr-07-4906 (2008).
Albanese, I. et al. Heterogeneity within and between primary colorectal carcinomas and matched metastases as revealed by analysis of Ki-ras and p53 mutations. Biochem Biophys Res Commun 325, 784–791, 10.1016/j.bbrc.2004.10.111 (2004).
Knijn, N. et al. KRAS mutation analysis: a comparison between primary tumours and matched liver metastases in 305 colorectal cancer patients. Br J Cancer 104, 1020–1026, 10.1038/bjc.2011.26 (2011).
Perrone, F. et al. PI3KCA/PTEN deregulation contributes to impaired responses to cetuximab in metastatic colorectal cancer patients. Ann Oncol 20, 84–90, 10.1093/annonc/mdn541 (2009).
Baldus, S. E. et al. Prevalence and heterogeneity of KRAS, BRAF and PIK3CA mutations in primary colorectal adenocarcinomas and their corresponding metastases. Clin Cancer Res 16, 790–799, 10.1158/1078-0432.ccr-09-2446 (2010).
Vakiani, E. et al. Comparative genomic analysis of primary versus metastatic colorectal carcinomas. J Clin Oncol 30, 2956–2962, 10.1200/jco.2011.38.2994 (2012).
Mariani, P. et al. Concordant analysis of KRAS status in primary colon carcinoma and matched metastasis. Anticancer Res 30, 4229–4235 (2010).
Park, J. H. et al. Analysis of KRAS, BRAF, PTEN, IGF1R, EGFR intron 1 CA status in both primary tumors and paired metastases in determining benefit from cetuximab therapy in colon cancer. Cancer Chemother Pharmacol 68, 1045–1055, 10.1007/s00280-011-1586-z (2011).
Tie, J. et al. KRAS mutation is associated with lung metastasis in patients with curatively resected colorectal cancer. Clin Cancer Res 17, 1122–1130, 10.1158/1078-0432.CCR-10-1720 (2011).
Watanabe, T. et al. Heterogeneity of KRAS status may explain the subset of discordant KRAS status between primary and metastatic colorectal cancer. Dis Colon Rectum 54, 1170–1178, 10.1097/DCR.0b013e31821d37a3 (2011).
Bossard, C. et al. Delineation of the infrequent mosaicism of KRAS mutational status in metastatic colorectal adenocarcinomas. J Clin Pathol 65, 466–469, 10.1136/jclinpath-2011-200608 (2012).
Kawamoto, Y. et al. KRAS mutations in primary tumours and post-FOLFOX metastatic lesions in cases of colorectal cancer. Br J Cancer 107, 340–344, 10.1038/bjc.2012.218 (2012).
Kim, M. J. et al. Different metastatic pattern according to the KRAS mutational status and site-specific discordance of KRAS status in patients with colorectal cancer. BMC Cancer 12, 347, 10.1186/1471-2407-12-347 (2012).
Miglio, U. et al. Mutation analysis of KRAS in primary colorectal cancer and matched metastases by means of highly sensitivity molecular assay. Pathol Res Pract 209, 233–236, 10.1016/j.prp.2013.02.006 (2013).
Mostert, B. et al. KRAS and BRAF mutation status in circulating colorectal tumor cells and their correlation with primary and metastatic tumor tissue. Int J Cancer 133, 130–141, 10.1002/ijc.27987 (2013).
Voutsina, A. et al. Combined analysis of KRAS and PIK3CA mutations, MET and PTEN expression in primary tumors and corresponding metastases in colorectal cancer. Mod Pathol 26, 302–313 (2013).
Oliveira, C. et al. KRAS and BRAF oncogenic mutations in MSS colorectal carcinoma progression. Oncogene 26, 158–163, 10.1038/sj.onc.1209758 (2007).
Vermaat, J. S. et al. Primary colorectal cancers and their subsequent hepatic metastases are genetically different: Implications for selection of patients for targeted treatment. Clin Cancer Res 18, 688–699, 10.1158/1078-0432.CCR-11-1965 (2012).
Shen, Y. Q., Ye, Y. B., Zheng, X. W., Li, C. & Chen, Q. K-ras mutations in colorectal cancer at different stages, Tumor. 30, 134–137, 10.3781/j.issn.1000-7431.2010.02.010 (2010).
Xian, H. B., Yu, H. B. & Zhang, J. R. Comparison of the grade of concordance in terms of K-ras status between primaries and related liver metastases in colorectal cancer [article in Chinese]. Chinese Journal of Cancer Prevention and Treatment 17, 926–929 (2010).
Cejas, P. et al. Concordance of K-Ras status between colorectal cancer (CRC) primaries and related metastatic samples considering clinicopathological features. http://meeting.ascopubs.org/cgi/content/abstract/27/15S/4053 [Accessed July 25, 2013].
Sood, A. et al. Beyond KRAS: The quest for novel genetic markers predictive for response to anti-epidermal growth factor receptor (EGFR) therapy in patients with metastatic colorectal cancer (mCRC). J Clin Oncol 28, 15s (2010).
Negri, F. V. et al. PTEN status in advanced colorectal cancer treated with cetuximab. Br J Cancer 102, 162–164, 10.1038/sj.bjc.6605471 (2010).
Santini, D. et al. High concordance of BRAF status between primary colorectal tumours and related metastatic sites: Implications for clinical practice. Ann Oncol 21, 1565, 10.1093/annonc/mdq318 (2010).
Cejas, P. et al. Analysis of the concordance in the EGFR pathway status between primary tumors and related metastases of colorectal cancer patients:implications for cancer therapy. Curr Cancer Drug Targets 12, 124–131, 10.2174/156800912799095162 (2012).
Oudejans, J. J., Slebos, R. J., Zoetmulder, F. A., Mooi, W. J. & Rodenhuis, S. Differential activation of ras genes by point mutation in human colon cancer with metastases to either lung or liver. Int J Cancer 49, 875–879 (1991).
Thebo, J. S., Senagore, A. J., Reinhold, D. S. & Stapleton, S. R. Molecular staging of colorectal cancer: K-ras mutation analysis of lymph nodes upstages Dukes B patients. Dis Colon Rectum 43, 155–159; discussion 159–162 (2000).
Al-Mulla, F. et al. Heterogeneity of mutant versus wild-type Ki-ras in primary and metastatic colorectal carcinomas and association of codon-12 valine with early mortality. J Pathol 185, 130–138, 10.1002/(sici)1096-9896(199806)185:2<130::aid-path85>3.0.co;2-m (1998).
Schimanski, C. C., Linnemann, U. & Berger, M. R. Sensitive Detection of K-ras Mutations Augments Diagnosis of Colorectal Cancer Metastases in the Liver. Cancer Res 59, 5169–5175 (1999).
Santini, D. et al. High concordance of KRAS status between primary colorectal tumors and related metastatic sites: implications for clinical practice. Oncologist 13, 1270–1275, 10.1634/theoncologist.2008-0181 (2008).
Melucci, E. et al. Relationship between K-Ras mutational status and EGFR expression evaluated using Allred score in primary and metastatic colorectal cancer. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed9&NEWS=N&AN=70259052 [Accessed July 25, 2013].
Italiano, A. et al. KRAS and BRAF mutational status in primary colorectal tumors and related metastatic sites: biological and clinical implications. Ann Surg Oncol 17, 1429–1434, 10.1245/s10434-009-0864-z (2010).
Cejas, P. et al. KRAS mutations in primary colorectal cancer tumors and related metastases: a potential role in prediction of lung metastasis. PLoS One 4, e8199, 10.1371/journal.pone.0008199 (2009).
Artale, S. et al. Mutations of KRAS and BRAF in primary and matched metastatic sites of colorectal cancer. J Clin Oncol 26, 4217–4219, 10.1200/jco.2008.18.7286 (2008).
Suchy, B., Zietz, C. & Rabes, H. M. K-ras point mutations in human colorectal carcinomas: relation to aneuploidy and metastasis. Int J Cancer 52, 30–33 (1992).
Losi, L., Benhattar, J. & Costa, J. Stability of K-ras mutations throughout the natural history of human colorectal cancer. Eur J Cancer 28A, 1115–1120 (1992).
Finkelstein, S. D., Sayegh, R., Christensen, S. & Swalsky, P. A. Genotypic classification of colorectal adenocarcinoma. Biologic behavior correlates with K-ras-2 mutation type. Cancer 71, 3827–3838 (1993).
Loupakis, F. et al. PTEN expression and KRAS mutations on primary tumors and metastases in the prediction of benefit from cetuximab plus irinotecan for patients with metastatic colorectal cancer. J Clin Oncol 27, 2622–2629, 10.1200/jco.2008.20.2796 (2009).
Atreya, C. E. et al. PTEN expression is consistent in colorectal cancer primaries and metastases and associates with patient survival. Cancer Med 2, 496–506 (2013).
Murata, A. et al. Methylation levels of LINE-1 in primary lesion and matched metastatic lesions of colorectal cancer. Br J Cancer 109, 408–415. (2013).
Kaneko, Y., Kuramochi, H., Nakajima, G., Inoue, Y. & Yamamoto, M. Degraded DNA may induce discordance of KRAS status between primary colorectal cancer and corresponding liver metastases. Int J Clin Oncol 19, 113–120 (2014).
Paliogiannis, P., Cossu, A., Tanda, F., Palmieri, G. & Palomba, G. KRAS mutational concordance between primary and metastatic colorectal adenocarcinoma. Oncol Lett 8, 1422–1426 (2014).
Baas, J. M., Krens, L. L., Guchelaar, H. J., Morreau, H. & Gelderblom, H. Concordance of predictive markers for EGFR inhibitors in primary tumors and metastases in colorectal cancer: a review. Oncologist 16, 1239–1249, 10.1634/theoncologist.2011-0024 (2011).
Bouchahda, M. et al. Acquired KRAS mutations during progression of colorectal cancer metastases: possible implications for therapy and prognosis. Cancer Chemother Pharmacol 66, 605–609, 10.1007/s00280-010-1298-9 (2010).
Whiting, P. F. et al. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann Intern Med 155, 529–536, 10.7326/0003-4819-155-8-201110180-00009 (2011).
Elm, E. v. et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335, 806–808, 10.1136/bmj.39335.541782.AD (2007).
Acknowledgements
The work is supported by the Health and Medical Research Fund from Food and Health Bureau of Hong Kong (Project no: 11120971 and 12130721) and the Direct Grant from the Chinese University of Hong Kong (Project no: 4054090).
Author information
Authors and Affiliations
Contributions
Study concept and design: J.L.T., C.M. Acquisition of data: Z.Y.Y., Y.Y.Y. Analysis and interpretation of data: X.Y.W., J.Q.Y. Drafting of the manuscript: C.M., X.Y.W., D.E.T. Critical revision of the manuscript for important intellectual content: J.L.T., C.M., D.E.T. Statistical analysis: X.Y.W., Y.Y.Y. Administrative, technical, or material support: J.Q.Y., Z.Y.Y. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplements
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Mao, C., Wu, XY., Yang, ZY. et al. Concordant analysis of KRAS, BRAF, PIK3CA mutations and PTEN expression between primary colorectal cancer and matched metastases. Sci Rep 5, 8065 (2015). https://doi.org/10.1038/srep08065
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep08065
This article is cited by
-
Tumor location matters, next generation sequencing mutation profiling of left-sided, rectal, and right-sided colorectal tumors in 552 patients
Scientific Reports (2024)
-
Biomarker concordance between primary colorectal cancer and ovarian metastases: a Dutch cohort study
Journal of Cancer Research and Clinical Oncology (2023)
-
Report of two patients in whom comparisons of the somatic mutation profile were useful for the diagnosis of metastatic tumors
Surgical Case Reports (2022)
-
Dynamic changes in longitudinal circulating tumour DNA profile during metastatic colorectal cancer treatment
British Journal of Cancer (2022)
-
Using single-cell sequencing technology to detect circulating tumor cells in solid tumors
Molecular Cancer (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.