Abstract
This large-scale survey aimed to evaluate frequencies and patterns of Chinese herbal medicine (CHM) used for Sjögren's syndrome (SS) in Taiwan by analyzing the National Health Insurance Research Database (NHIRD) for cases in which CHM was used as an alternative therapy to Western medicine for improving patients' discomforts. We analyzed cases of SS principal diagnosis (ICD-9:710.2) with a catastrophic illness certificate (CIC) in traditional Chinese medicine (TCM) outpatient clinics from three cohorts of the Longitudinal Health Insurance Database (LHID) in the NHIRD between 2002 and 2011. CHM prescription patterns for SS were evaluated from claimed visitation files and corresponding prescription files. There were 15,914 SS patients with CIC (SS/CIC) and we found only 130 SS/CIC cases visiting TCM clinics in LHID2000, 133 in LHID2005 and 126 in LHID2010. After removing duplicate data, 366 SS/CIC and 4,867 visits were analyzed. The 50–59 year age group showed the highest ratio (29.51%) in both women and men. “Qi-Ju-Di-Huang-Wan” and “Xuan-Shen” (Scrophularia ningpoensis Hemsl.) was the most commonly used formula and single herb, respectively. “Qi-Ju-Di-Huang-Wan, Gan-Lu-Yin, Xuan-Shen, Mai-Men-Dong (Ophiopogon japonicus (L. f.) Ker-Gawl.) and Sheng-Di-Huang (raw Rehmannia glutinosa Libosch)” were the core pattern prescriptions in treating SS/CIC.
Similar content being viewed by others
Introduction
Sjögren's syndrome (SS) is an autoimmune disease that mainly involves exocrine glands such as lacrimal and salivary glands. It causes glandular dysfunction, manifesting in dry mouth and dry eye1. SS can be classified as either primary or secondary2. Primary SS (pSS) presents as SS alone, whereas secondary SS occurs when another autoimmune disease, such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), or systemic sclerosis, is present. In Taiwan, the incidence of pSS from 2005 to 2007 was 6.0 (per 100,000 inhabitants) with a female/male ratio of 9.93. The prevalence of SS was ranked third among autoimmune rheumatic diseases in Taiwan from 2000 to 20084.
The pathogenesis of pSS remains unclear, but some clues support the hypothesis that the dysfunction of B cells and T cells leads to autoimmune epithelitis5. In addition, type I interferon and B cell-activating factor play important roles in the pathogenesis of pSS6.
Because some individuals with SS have a high risk of developing non-Hodgkin's lymphoma7 and some SS patients treated with conventional Western medicine still have discomforts, such as pain and fatigue8, these individuals have sought complementary and alternative medicine (CAM) for relieving symptoms.
Chinese herbal medicine (CHM)9 and acupuncture10 are common CAM therapies widely accepted by SS patients. Some randomized control trial have been performed in treating SS, but no specific CHM could be recommended for treating SS11. However, most of these trials suffered from poor methodological quality of trials and high heterogeneity of interventions. Hence, no specific CHM has been recommended for treating SS.
In Taiwan, National Health Insurance (NHI) has covered both Western medicine and traditional Chinese medicine (TCM) medical care since 199512. Most of the general population (98%) in Taiwan was covered in the NHI program at the end of 2012. A recent large-scale investigation about TCM usage for SS in Taiwan showed that Qi-Ju-Di-Huang-Wan was the most commonly prescribed Chinese herbal formula for SS13. However, the report included only one LHID cohort (1 million randomly sampled subjects) and the results may have been overestimated among patients recruited with regard to TCM visits and the average daily dose of Chinese formula. Hence, we conducted a national population-based study from the three cohorts of LHID in Taiwan for CHM usage among SS patients from 2002 to 2011. We focused on SS patients with CIC and SS as the principal diagnosis visiting for TCM.
Methods
Data Sources
The NHI program has a unique database that was implemented in Taiwan in 1995 and covers almost the entire population. Accordingly, TCM outpatient service for adults and children was analyzed from that time14,15. Nationwide medical information is recorded as electronic claim data in the National Health Insurance Research Database (NHIRD), which contains gender, age, dates of encounters, disease diagnosis of patients and prescriptions for all beneficiaries16. Scrambling cryptogram was performed on these data to protect patient and institutional privacy. The study population was defined by disease diagnosis according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). As we conducted a retrospective analysis of the NHIRD and all the individual information data are de-identified, we could not obtain informed consent from included patients. This study was approved by the Institutional Review Board of Taipei Veterans General Hospital (VGHIRB-2013-04-005E).
Identification of Patients with Sjögren's Syndrome
We designed a national population-based study to analyze three cohorts of 1 million random sample subjects selected from all beneficiaries of the NHI program in Taiwan and we surveyed the CHM usage rate and patterns to determine the utilization of subjects with the principal diagnosis of SS treated in TCM outpatient clinics. The usage of principal diagnosis of SS in TCM visits can reduce measurement bias that would be imposed by TCM visits for non-SS treatments.
SS is one of the 31 categories of major illnesses or injuries that result in a patient holding a catastrophic illness certificate (CIC). As SS and sicca syndrome have the same ICD-9 code, “710.2,” we identified “true” SS from CIC holders between 2002 and 2011. These populations were matched with the three cohorts of 1 million random samples from the Longitudinal Health Insurance Database (LHID2000, LHID2005 and LHID2010), which extracted 1 million random samples from 26 million individuals in the NHIRD in 2000, 2005 and 2010. SS subjects were included in this study after removing duplicate data. Figure 1 shows the subject recruitment flowchart from the 3 million random samples for SS with CIC from the NHIRD in Taiwan.
Flowchart of recruitment of patients with Sjögren's syndrome and a catastrophic illness certificate from the 3 million random samples.
We identified Sjögren's syndrome in individuals with an ICD-9 code of “710.2” and a catastrophic illness certificate in Taiwan between 2002 and 2011 and they were matched with three cohorts of 1 million random samples from the LHID2000, LHID2005 and LHID2010. Subjects with a catastrophic illness certificate were included after duplicate data were removed.
Data Analysis
SPSS version 19.0 (SPSS Inc., Chicago, IL, USA) used applied to analyze the frequency and patterns of formulae or single herb usage and CHM utilization. Categorical data are presented as absolute numbers and percentages and continuous data are presented as means ± standard deviations. Data linkage analysis and processing were conducted with Structure Query Language (SQL server 2008, Microsoft Corp., Redmond, WA, USA). In addition, we identified core patterns of CHMs used in treating SS/CIC patients using an open-sourced freeware NodeXL (http://nodexl.codeplex.com/) and all the selected combinations were utilized for network analysis. The line width, ranging from 1 to 10 in the network figure was defined by counts of connections between a certain CHM and co-prescribed CHMs and thicker widths of line connections indicated crucial prescription patterns. If the line width is thicker between CHM-A and CHM-B than that between CHM-A and CHM-C, the connection between CHM-A and CHM-B is co-prescribed more frequently than CHM-A and CHM-C. The top five core patterns of CHMs were clearly identified within the network analysis of CHM utilization.
Results
There were 15,914 SS patients with CIC (SS/CIC) in Taiwan from 2002 to 2011; however, there were only 683 SS/CIC with a principal diagnosis of SS in LHID2000, 678 in LHID2005 and 635 in LHID2010, respectively. In these three LHID datasets, more than 90% of SS outpatients had visited TCM clinics. However, not all patients visited TCM clinics for SS and we only included principal diagnosis SS cases for TCM visits. After removing 23 cases of duplicate data, we found 130 SS patients in LHID2000, 133 in LHID2005 and 126 in LHID2010. There were 366 SS patients and 4,867 visits with a principal diagnosis of SS in TCM clinics from 2002 to 2011. The recruitment flowchart for subjects treated for SS/CIC with CHM from the 3 million random samples in the Taiwan NHIRD is shown in Figure 1.
There were 339 female and 27 male patients with SS/CIC treated with CHM. Female patients preferred using CHM for SS more than male patients did (female:male = 12.56:1). The age-sex-specific frequency of CHM used in SS/CIC patients is illustrated in Table 1 and the age and sex of SS/CIC were recorded only at the time of first visit to TCM clinics. The 50–59 year age group had the highest usage percentage (29.79% and 25.93% for males and females, respectively) and the mean ± SD for age was 54.82 ± 13.00 in females and 57.96 ± 16.42 in males, overall.
The mean ± SD TCM clinic visits among 366 SS/CIC patients was 13.30 ± 20.09. Most SS/CIC patients visited TCM clinics less than 10 times and the maximum was 129. The mean ± SD medical services provided from 472 TCM doctors was 10.31 ± 19.15. Most TCM doctors treated SS patients less than 10 times and the maximum was 143. Table 2 shows the SS/CIC visit distribution for patients and doctors in Taiwan.
Table 3 presents the top 10 formulae for treating SS among the 26,733 total CHM prescriptions. The most commonly used formula was “Qi-Ju-Di-Huang-Wan” (9.08%) and the average daily dosage was 4.78 ± 1.62 gram (g). The next most common formulae were “Gan-Lu-Yin” (8.16%), “Jia-Wei-Xiao-Yao-San” (6.02%), “Zhi-Gan-Cao-Tang” (2.06%) and “Xue-Fu-Zhu-Yu-Decoction” (2.03%) with average daily dosages of 4.37 ± 1.78 g, 4.70 ± 1.49 g, 3.65 ± 2.23 g and 4.50 ± 2.21 g, respectively.
The top 10 single herbs used for SS/CIC are listed in Table 4. “Xuan-Shen” (Scrophularia ningpoensis Hemsl., 2.98%) was the most commonly used single herb and the average daily dosage was 1.86 ± 0.41 g, followed by “Mai-Men-Dong” (Ophiopogon japonicus (L. f.) Ker-Gawl., 2.93%), “Sheng-Di-Huang” (raw Rehmannia glutinosa Libosch., 21.7%), “Tian-Hua-Fen” (Trichosanthes kirilowii Maxim., 2.04%) and “Huang-Qin” (Scutellaria baicalensis Georgi, 1.95%) with average daily dosages of 1.38 ± 0.58 g, 1.42 ± 0.52 g, 1.24 ± 0.46 g and 1.24 ± 0.46 g, respectively.
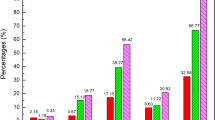
Supplementary Figure S1 shows that SS/CIC patients were given an average of 6.24 ± 2.47 CHM items in a single prescription and five CHM items (16.85%) was the most common prescription for combinations of formulae or single herbs. The next most common values were 6 (16.71%) and 7 CHM items (13.77%). Very few SS patients (0.05%) were prescribed more than 20 CHM items.
Among these prescriptions, we analyzed the co-prescription pattern of formulae and single herbs. Supplementary Table S1 shows the most common prescription patterns of two formula combinations and two single herb combinations. The most common two formula combination was “Qi-Ju-Di-Huang-Wan plus Gan-Lu-Yin,” followed by “Jia-Wei-Xiao-Yao-San plus Qi-Ju-Di-Huang-Wan,” “Jia-Wei-Xiao-Yao-San plus Ping-Wei-San,” “Jia-Wei-Xiao-Yao-San plus Zhi-Bo-Di-Huang-Wan,” and “Gan-Lu-Yin plus Sang-Ju-Yin.” The most common two single herb combinations were “Xuan-Shen plus Mai-Men-Dong,” “Sheng-Di-Huang plus Mai-Men-Dong,” “Xuan-Shen plus Sheng-Di-Huang,” “Gou-Qi plus Mai-Men-Dong,” and “Sha-Can (Glehnia littoralis F. Schmidt ex Miq.) plus Mai-Men-Dong.”
Table 5 shows the most common prescription patterns of double and triple formula/single herb combinations. The most common combination of two formulae/single herbs was “Qi-Ju-Di-Huang-Wan plus Gan-Lu-Yin,” followed by “Xuan-Shen plus Mai-Men-Dong,” “Sheng-Di-Huang plus Mai-Men-Dong,” “Xuan-Shen plus Sheng-Di-Huang,” and “Xuan-Shen and Gan-Lu-Yin.” The most common combination of three formulae/single herbs was “Xuan-Shen, Sheng-Di-Huang, plus Mai-Men-Dong,” followed by “Nu-Zhen-Zi (Ligustrum lucidum Ait.), Jia-Wei-Xiao-Yao-San, plus Gou-Qi,” “Nu-Zhen-Zi, Wu-Wei-Zi (Schizandra chinensis (Turcz.) Baill.), plus Jia-Wei-Xiao-Yao-San,” “Wu-Wei-Zi, Jia-Wei-Xiao-Yao-San, plus Gou-Qi,” and “Qi-Ju-Di-Huang-Wan, Gan-Lu-Yin, plus Dan-Can.” The network analysis presented in Figure 2 demonstrates that Qi-Ju-Di-Huang-Wan, Gan-Lu-Yin, Xuan-Shen, Mai-Men-Dong and Sheng-Di-Huang formed the core patterns of Chinese formulae and herbs used to treat SS/CIC patients.
The core pattern of Chinese formula and single herb usage for Sjögren's syndrome.
The top 50 Chinese formulae and single herbs for Sjögren's syndrome patients with a catastrophic illness certificate were analyzed through open-sourced freeware NodeXL and the core pattern of these CHMs showed that Qi-Ju-Di-Huang-Wan, Gan-Lu-Yin, Xuan-Shen, Mai-Men-Dong and Sheng-Di-Huang are among the most frequently used combinations.
Discussion
This was the first nationwide population-based survey of the utilization and core pattern analysis of CHM in SS/CIC from the three LHIDs in Taiwan. Female SS/CIC patients used CHM far more frequently than males did (12.56:1 ratio) and females and males aged between 50 and 59 years had the highest rates of CHM use for SS/CIC. This may be accounted for by a lack of active estrogens and androgens, leading to apoptosis in epithelial salivary gland cells17. A recent study demonstrated different serum endocrine levels according to SS symptoms, suggesting that oral dryness may be related to low androgen levels, while low estrogen levels manifest as ocular dryness18.
In total, there were 15,914 SS/CIC patients from the Taiwan CIC database from 2002 to 2011 (there were 72,391 total cases of generalized autoimmune syndrome requiring lifelong treatment with CIC up to 2012)19. There were 366 principal diagnosis SS/CIC patients who used CHM across the three LHIDs with duplicate data removed. The sample size in this study was not large enough, as the LHIDs only provided 1 million random samples and thus the sample size could not represent all SS/CIC patients undergoing CHM treatment. The database could only represent the ratio of 1 million samples over a total of 23.4 million inhabitants (4.27%). We found that the ratio of SS/CIC patients treated with CHM could be traced back to represent 63.55% of the entire SS/CIC population, a ratio that could also match the nationwide survey of TCM utilization20.
Hydroquinone is the main Western medicine used on SS patients in Taiwan; it has immune regulatory effects and can improve fatigue, arthralgia and myalgia. However, a recent study showed that hydroxychloroquine did not improve symptoms during 24 weeks of treatment for pSS21. Saliva and tear substitutes usually treat only dryness symptoms, but some patients received oral corticosteroids, NSAIDs, azathioprine and cyclosporine for anti-inflammation and immuno-suppression. Pilocarpine and cevimeline are muscarinic acetylcholine receptor agonists for treating dry mouth22, but these drugs can cause gastrointestinal discomfort, sweating, flush and blurred vision. For some SS patients with affected extra-glandular organs, biologic agents, like etanercept and rituximab, might be required to treat severe systemic involvement. However, these are more costly and they carry many adverse effects. Hence, an increasing number of SS patients seek TCM to treat SS or alleviate the adverse effects of the above drugs.
There were 366 subjects who made TCM clinic visits to 472 TCM doctors; four subjects visited over 100 times from 2002 to 2011, while 238 subjects (65.03%) visited less than 10 times. A similar situation was observed among doctors, such that only three doctors received more than 100 visits, while 343 doctors (72.67%) had been visited less than 10 times. The phenomenon of doctor shopping among patients with chronic illness may account for the observation that many SS/CIC patients received CHM treatment from different TCM doctors23. Doctor shopping likely occurred because the health service system of family doctors had not yet been well-established in Taiwan24; therefore, patients who have been bothered by persistent symptoms and medication side effects often seek a second opinion25. Healthcare resources may be also wasted due to this doctor shopping in TCM26.
SS is called “dry-Bi” or “dryness impediment” in TCM and the TCM pathogenesis of SS is highly correlated with “Yin-deficiency,” manifesting as “dryness-heat” and “consumption and deficiency of qi and body fluid”27. Thus, dry eye and dry mouth are considered the external symptoms of the impaired functions. Given this pathogenesis, clinical treatments usually seek to “Enrich yin and clear heat” or “Nourish yin and moisten dryness,” and “Qi-Ju-Di-Huang-Wan,” “Gan-Lu-Yin,” “Xuan-Shen,” and “Mai-Men-Dong” are the commonly used Chinese formulas/single herbs. Some SS patients have fibrotic changes in their salivary glands, which is compatible with the TCM pathogenesis of “Stasis.” “Xue-Fu-Zhu-Yu-Decoction” and “Dan-Can” could “Quicken the blood and dispel stasis.” However, there are some different patterns, like “Qi depression” or “dampness,” for which “Jia-Wei-Xiao-Yao-San” could “Course the liver and resolve depression,” and “Ping-Wei-San” could “Dry dampness and fortify the spleen.” TCM doctors usually recognize the TCM patterns of SS first and then prescribe different formula or single herbs accordingly.
“Qi-Ju-Di-Huang-Wan” was the most commonly used formula for SS/CIC; its therapeutic function is to “nourish the liver and brighten the eyes,” and it could be used for SS and dry eye. Recent studies have reported that “Qi-Ju-Di-Huang-Wan” is more effective than conventional medicine for SS, regardless of whether it is used alone28 or in addition to acupuncture29. Chang30 used “Qi-Ju-Di-Huang-Wan” with a randomized, double-masked, parallel grouped controlled study to treat dry eyes and the result showed reduction in corneal epithelium abnormalities and it could also act as an alternative to topical eye drops. However, subjects in Chang's study had dry eye syndrome, not SS and thus “Qi-Ju-Di-Huang-Wan” may have therapeutic effects for dry eye symptoms of SS.
“Gan-Lu-Yin” was the second most commonly used formula in our database; its therapeutic function is to “enrich yin and clear heat,” and it can be used for the treatment of SS and dry mouth. A study used “Gan-Lu-Yin” in post-radiotherapy nasopharyngeal cancer patients to alleviate mucositis and dry mouth31. “Jia-Wei-Xiao-Yao-San” can “course the liver and resolve depression,” and Yi et al.32 used it to treat xerophthalmia in perimenopausal women with significant improvement of visual fatigue sensation, red eye, dryness, foreign body sensation, burning sensation and photophobia. “Zhi-Gan-Cao-Tang” can “boost qi and enrich yin”; however, no studies have discussed it for treating SS-related symptoms. “Xue-Fu-Zhu-Yu-Decoction” can “quicken the blood and dispel stasis,” and it can modulate the immune function of B cells and T cells33 and alleviate tissue fibrosis34.
“Xuan-Shen” was the most commonly used single herb, with the function of “enrich yin and clear heat,” and it has some positive effects on anti-inflammation and tumor cell apoptosis35. “Mai-Men-Dong” was the second most commonly used single herb to “nourish yin and moisten dryness”; it can down-regulate mRNA expression of TGF-β1 and has potential antioxidant effects36. “Sheng-Di-Huang” can “enrich yin and clear heat,” and it also reduces eosinophil cationic proteins levels, which are positively correlated with “heat zheng”37 and has anti-inflammatory properties38. “Tian-Hua-Fen” can “clear heat and engender liquid,” and it can inhibit nitric oxide activity and elevate anti-inflammatory effects39. “Huang-Qin” can “clear heat and drain fire,” and it has the function of scavenging reactive oxygen species40. We also listed relevant studies for the top 10 most commonly used formulae and single herbs in Tables 3 and 4.
Figure 2 includes the top 50 Chinese formulas and single herbs for SS/CIC patients and shows the core pattern of these CHMs. This figure implies that “Qi-Ju-Di-Huang-Wan,” “Gan-Lu-Yin, Xuan-Shen,” “Mai-Men-Dong,” and “Sheng-Di-Huang” are among the most frequently used combinations. Although these items may have effects on antioxidant capacity, anti-inflammation and dry eye or dry month improvement, they have rarely been applied in clinical trials. Furthermore, these five CHMs from the core pattern identified did little have immune modulation or tissue fibrosis alleviation functions. The above CHMs may have effects on immune regulation, but there is little evidence to support this point. This kind of explanation according to modern biomedical categories may be biased and downplay TCM theory and CHM use. There may indeed be undiscovered immune regulation effects, so we are now conducting a clinical trial attempting to determine the mechanism of SS-1 and its components with antioxidant capacity, anti-inflammation, immune modulation and anti-fibrosis cell-line basic research. In the future, we may further use this model to screen other CHMs for treating SS. However, no specific CHM could be recommended for clinical use11.
For this purpose, we initiated a randomized, double-blind, placebo-controlled, cross-over design clinical trial (Clinicaltrials.gov NCT02110446) for SS/CIC patients in order to evaluate the efficacy of CHM (SS-1) on the regulation of oxidative stress-related cytokines and antioxidant capacity. “Gan-Lu-Yin, Sang-Ju-Yin and Xue-Fu-Zhu-Yu-Decoction” with a ratio of 2:1:1 is the composition of SS-1 and its therapeutic functions include antioxidant capacity, anti-inflammation, immune modulation, anti-fibrosis and dry mouth improvement31,33,34,41,42. This combination of SS-1 has been effective in our clinical experience. We use “Gan-Lu-Yin” for “Enrich yin and clear heat,” “Xue-Fu-Zhu-Yu-Decoction,” for “quicken the blood and dispel stasis,” and “Sang-Ju-Yin” for “Course wind and discharge heat.” Thus, SS-1 can improve dryness symptoms of dry eye, dry mouth and other exocrine glands. As the core patterns in our database were treated the patient with “enrich yin” most frequently and “Qi-Ju-Di-Huang-Wan” takes long time to enrich the internal yin (liver yin and kidney yin), before spreading to the exterior. Thus, we use “Gan-Lu-Yin” to enrich the exterior yin first and “Sang-Ju-Yin” can bring these fluids and yin outside to superficial areas for the mucosa of exocrine glands. However, some patients have had SS for a long time and the salivary glands come to a state of “Qi stagnation and blood stasis.” “Xue-Fu-Zhu-Yu-Decoction” can improve this situation. Although SS-1 is frequently used in our clinical practice for treating with SS, it was not yet have evidence-based support by a well-designed RCT to verify its efficacy and safety. Thus, we initiated a well-designed clinical trial and we expect improvements in quality of life and clinical manifestations through reduction of oxidative stress. We also plan to use an SS cell model to elucidate the antioxidant effects and the mechanism of action of SS-1.
As this study was a retrospective study, we could not recognize the different herbs or formulae that were selected for different presentations of SS according to TCM diagnosis. This is indeed the limitation of our study, but ours results could still demonstrate overall patterns in TCM treatment for SS. We might develop further studies to discuss the clinical thinking processes among TCM doctors. In our ongoing SS-1 clinical trial, we also want to observe whether the uniform treatment for the various patterns of SS-1 lead to different outcomes.
Years of practicing TCM experience may affect clinical treatment decision making - this is an important issue and a potential confounding factor. However, the NHIRD did not capture the information about patients' TCM patterns, years of practicing TCM experience and the practitioners' education, so we could not analyze these factors in our study. However, it deserves to conduct the survey for these TCM variables in the future.
Our analysis shows different results from a recent SS report surveying CHM prescription patterns in Taiwan from 1997 to 200813. (1) We included SS/CIC subjects from three LHIDs between 2002 and 2011 for a comprehensive and up-to-date nationwide survey. (2) We only included principal diagnosis of SS/CIC in TCM visits to reduce the measurement bias due to TCM visits for non-SS treatments. (3) The statistics of SS/CIC patient numbers and the dosage of the top 10 Chinese formulae demonstrated more rational and significant results in this study.
However, there are some limitations to this study. (1) Many potential SS patients accepted conventional therapy or TCM, but they were not CIC holders due to incompatibility of histopathology or autoantibody criteria. As the SS subjects included in this study were required to have a CIC, the CHM utilization among SS patients may have been underestimated. (2) The sample size in this study was not large enough; hence, we should conduct another larger survey on this issue in the future. (3) As the subjects included in this study were extracted from three LHIDs, multivariate logistic regression was not conducted to evaluate factors correlated with CHM utilization. (4) We studied only the utilization of CHM in the recruited SS/CIC patients; however, we did not investigate the utilization of acupuncture, Chinese tuina, or other CAMs, which might also be applied in SS therapies. (5) The safety data in this retrospective study is lacking and so we cannot evaluate the safety of CHM.
Conclusions
“Qi-Ju-Di-Huang-Wan” was the most commonly used formula, while “Xuan-Shen” was the most commonly used single herb in our database. Among different age groups, the highest utilization of CHM was found between ages 50 and 59 in both females and males. The most commonly used two formula combination was “Qi-Ju-Di-Huang-Wan plus Gan-Lu-Yin,” and the most commonly used two single herb combination was “Xuan-Shen plus Mai-Men-Dong.” The core pattern prescriptions were “Qi-Ju-Di-Huang-Wan,” “Gan-Lu-Yin,” “Xuan-Shen,” “Sheng-Di-Huang,” and “Mai-Men-Dong.” However, the therapeutic effects and safety of these commonly used CHMs for treating SS have not been clearly elaborated, so well-designed clinical trials for this purpose are required in the future.
Change history
25 May 2017
A correction has been published and is appended to both the HTML and PDF versions of this paper. The error has not been fixed in the paper.
08 October 2015
A correction has been published and is appended to both the HTML and PDF versions of this paper. The error has not been fixed in the paper.
25 May 2017
Scientific Reports 5: Article number: 9541; published online: 29 April 2015; updated: 25 May 2017. In this Article, Affiliation 2 is incorrectly listed as ‘Graduate Institute of Clinical Medicine, and Graduate Institute of Traditional Chinese Medicine, College of Medicine, Chang Gung University, Taoyuan, Taiwan’.
References
Tincani, A. et al. Novel aspects of Sjogren's syndrome in 2012. BMC Med 11, 93, 10.1186/1741-7015-11-93 (2013).
Bowman, S. J. & Fox, R. I. Classification criteria for Sjogren's syndrome: nothing ever stands still!. Ann Rheum Dis 73, 1–2, 10.1136/annrheumdis-2013-203953 (2014).
Weng, M. Y., Huang, Y. T., Liu, M. F. & Lu, T. H. Incidence and mortality of treated primary Sjogren's syndrome in Taiwan: a population-based study. J Rheumatol 38, 706–708, 10.3899/jrheum.100883 (2011).
Yu, K. H., See, L. C., Kuo, C. F., Chou, I. J. & Chou, M. J. Prevalence and incidence in patients with autoimmune rheumatic diseases: a nationwide population-based study in Taiwan. Arthritis Care Res (Hoboken) 65, 244–250, 10.1002/acr.21820 (2013).
Voulgarelis, M. & Tzioufas, A. G. Pathogenetic mechanisms in the initiation and perpetuation of Sjogren's syndrome. Nat Rev Rheumatol 6, 529–537, 10.1038/nrrheum.2010.118 (2010).
Nocturne, G. & Mariette, X. Advances in understanding the pathogenesis of primary Sjogren's syndrome. Nat Rev Rheumatol 9, 544–556, 10.1038/nrrheum.2013.110 (2013).
Johnsen, S. J. et al. Risk of non-Hodgkin's lymphoma in primary Sjogren's syndrome: a population-based study. Arthritis Care Res (Hoboken) 65, 816–821, 10.1002/acr.21887 (2013).
Segal, B. et al. Prevalence, severity and predictors of fatigue in subjects with primary Sjogren's syndrome. Arthritis Rheum 59, 1780–1787, 10.1002/art.24311 (2008).
Wu, G. L., Li, T. Y., Fan, Y. S. & Yu, G. Y. Therapeutic effect of Chinese herbal medicine for strengthening qi, nourishing yin and removing stasis on serum osteopontin and quality of life of patients with primary Sjogren's syndrome. Chin J Integr Med 17, 710–714, 10.1007/s11655-011-0850-8 (2011).
List, T., Lundeberg, T., Lundstrom, I., Lindstrom, F. & Ravald, N. The effect of acupuncture in the treatment of patients with primary Sjogren's syndrome. A controlled study. Acta Odontol Scand 56, 95–99 (1998).
Luo, H., Li, X., Liu, J., Andrew, F. & George, L. Chinese Herbal Medicine in Treating Primary Sjogren's Syndrome: A Systematic Review of Randomized Trials. Evid Based Complement Alternat Med 2012, 640658, 10.1155/2012/640658 (2012).
Lee, Y. C. et al. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res 10, 225, 10.1186/1472-6963-10-225 (2010).
Yu, M. C., Lin, S. K., Lai, J. N., Wei, J. C. & Cheng, C. Y. The traditional Chinese medicine prescription patterns of Sjogrens patients in Taiwan: A population-based study. J Ethnopharmacol, 10.1016/j.jep.2014.05.049 (2014).
Yen, H.R.., Huang, T.P.., Sun, M.F.. Chinese medicine usage in Taiwan: a nationwide population-based study. RCHM Journal 10, 21–27 (2013).
Huang, T. P. et al. A nationwide population-based study of traditional Chinese medicine usage in children in Taiwan. Complement Ther Med 22, 500–510, 10.1016/j.ctim.2014.04.002 (2014).
Cheng, S. H. & Chiang, T. L. The effect of universal health insurance on health care utilization in Taiwan. Results from a natural experiment. JAMA 278, 89–93 (1997).
Mavragani, C. P., Fragoulis, G. E. & Moutsopoulos, H. M. Endocrine alterations in primary Sjogren's syndrome: an overview. J Autoimmun 39, 354–358, 10.1016/j.jaut.2012.05.011 (2012).
Forsblad-d'Elia, H., Carlsten, H., Labrie, F., Konttinen, Y. T. & Ohlsson, C. Low serum levels of sex steroids are associated with disease characteristics in primary Sjogren's syndrome; supplementation with dehydroepiandrosterone restores the concentrations. J Clin Endocrinol Metab 94, 2044–2051, 10.1210/jc.2009-0106 (2009).
Administration, N. H. I. Medical Utilization of Major Illness/Injury. (National Health Insurance Administration, Taipei, 2012).
Chen, F. P. et al. Use frequency of traditional Chinese medicine in Taiwan. BMC Health Serv Res 7, 10.1186/1472-6963-7-26 (2007).
Gottenberg, J. E. et al. Effects of hydroxychloroquine on symptomatic improvement in primary Sjogren syndrome: the JOQUER randomized clinical trial. JAMA 312, 249–258, DOI:10.1001/jama.2014.7682 (2014).
Ramos-Casals, M., Brito-Zeron, P., Siso-Almirall, A., Bosch, X. & Tzioufas, A. G. Topical and systemic medications for the treatment of primary Sjogren's syndrome. Nat Rev Rheumatol 8, 399–411, DOI:10.1038/nrrheum.2012.53 (2012).
Sato, T., Takeichi, M., Shirahama, M., Fukui, T. & Gude, J. K. Doctor-shopping patients and users of alternative medicine among Japanese primary care patients. Gen Hosp Psychiatry 17, 115–125 (1995).
Mercer, S. W. et al. A qualitative study of the views of patients with long-term conditions on family doctors in Hong Kong. BMC Fam Pract 11, 46, 10.1186/1471-2296-11-46 (2010).
Siu, J. Y. “Seeing a doctor is just like having a date”: a qualitative study on doctor shopping among overactive bladder patients in Hong Kong. BMC Fam Pract 15, 27, 10.1186/1471-2296-15-27 (2014).
Wang, M. J. & Lin, S. P. Study on doctor shopping behavior: insight from patients with upper respiratory tract infection in Taiwan. Health Policy 94, 61–67, 10.1016/j.healthpol.2009.08.009 (2010).
Shui-yan, Z. The TCM Etiology, Pathogenesy and Differential Treatment for Sjogren's Syndrome. JTCM 31, 73–78 (2011).
Zhao, Z. W. & Wang, W. R. Modified Qiju Dihuang decoction in the treatment of 30 cases of primary Sjögren's syndrome. Chinese Journal of Traditional Medical Science and Technology 10, 314–315 (2003).
Zhou, Q. & Zhu, H. Q. Integrated traditional Chinese and western medicine in the treatment of 34 cases of Sjögren's syndrome. Journal of New Chinese Medicine 29, 29–30 (1997).
Chang, Y. H., Lin, H. J. & Li, W. C. Clinical evaluation of the traditional chinese prescription Chi-Ju-Di-Huang-Wan for dry eye. Phytother Res 19, 349–354, 10.1002/ptr.1687 (2005).
Lin, I. H. Mucositis and dry mouth due to NPC radiotherapy treated by Chinese herb Gan-Lu-Yin. Yearbook of Chinese Medicine abd Pharmacy 8, 127–145 (2000).
Yi, Y.-M., Yi, J.-L., Cheng, X.-H., Zuo, Z.-Q. & Luo, Y.-Y. Efficacy of Modified Xiaoyaosan in Perimenopausal Women with Xerophthalmia. Practical Clinical Medicine 14, 82–85 (2013).
Ji, C.-Z., Zhang, P.-Y., Wang, Y.-X., Zhang, D.-S. & Zhang, L. Effect of Xuefuzhuyu soup on the levels of IL-2 and SIL-2R in mice serum. Journal of Qiqihar Medical 1, 540–541 (1999).
Shao, S.-J. The clinical application and research progress of Xie-Fu-Zhu-Yu-Tang. Beijing Journal of Traditional Chinese Medicine 27, 724–727 (2008).
Shen, X., Eichhorn, T., Greten, H. J. & Efferth, T. Effects of Scrophularia ningpoensis Hemsl. on Inhibition of Proliferation, Apoptosis Induction and NF-kappaB Signaling of Immortalized and Cancer Cell Lines. Pharmaceuticals (Basel) 5, 189–208, 10.3390/ph5020189 (2012).
Chen, X. M. et al. Protective effect of the polysaccharide from Ophiopogon japonicus on streptozotocin-induced diabetic rats. Carbohydr Polym 94, 378–385, 10.1016/j.carbpol.2013.01.037 (2013).
Hsu, C. H., Yu, M. C., Lee, C. H., Lee, T. C. & Yang, S. Y. High eosinophil cationic protein level in asthmatic patients with “heat” Zheng. Am J Chin Med 31, 277–283, 10.1142/S0192415x03000965 (2003).
Chang, H. T. et al. Inhibition of the interactions between eosinophil cationic protein and airway epithelial cells by traditional Chinese herbs. BMC Syst Biol 4 Suppl 2S8, 10.1186/1752-0509-4-s2-s8 (2010).
Arawwawala, M., Thabrew, I., Arambewela, L. & Handunnetti, S. Anti-inflammatory activity of Trichosanthes cucumerina Linn. in rats. J Ethnopharmacol 131, 538–543, 10.1016/j.jep.2010.07.028 (2010).
Wang, S. C. et al. Baicalin Scavenges Reactive Oxygen Species and Protects Human Keratinocytes Against UVC-induced Cytotoxicity. In Vivo 27, 707–714 (2013).
Poon, P. M. et al. Immunomodulatory effects of a traditional Chinese medicine with potential antiviral activity: a self-control study. Am J Chin Med 34, 13–21, 10.1142/S0192415X0600359X (2006).
Fang, Z. et al. Replacements of rare herbs and simplifications of traditional chinese medicine formulae based on attribute similarities and pathway enrichment analysis. Evid Based Complement Alternat Med 2013, 136732, 10.1155/2013/136732 (2013).
Peng, H.-R. Great Compendium of Chinese Medical Formulae (People's Medical Publishing House, Beijing, 2005).
Chen, W. et al. High-frequency ultrasound imaging to evaluate liver fibrosis progression in rats and yi guan jian herbal therapeutic effects. Evid Based Complement Alternat Med 2013, 302325, 10.1155/2013/302325 (2013).
Gou, X. et al. Urine metabolic profile changes of CCl4-liver fibrosis in rats and intervention effects of Yi Guan Jian Decoction using metabonomic approach. BMC Complement Altern Med 13, 123, 10.1186/1472-6882-13-123 (2013).
Lin, H. J. et al. Hepatoprotective effects of Yi Guan Jian, an herbal medicine, in rats with dimethylnitrosamine-induced liver fibrosis. J Ethnopharmacol 134, 953–960, 10.1016/j.jep.2011.02.013 (2011).
Lin, H. J. et al. A Chinese Herbal Decoction, Modified Yi Guan Jian, Induces Apoptosis in Hepatic Stellate Cells through an ROS-Mediated Mitochondrial/Caspase Pathway. Evid Based Complement Alternat Med 2011, 459531, 10.1155/2011/459531 (2011).
Mu, Y. et al. Action mechanism of Yi Guan Jian Decoction on CCl4 induced cirrhosis in rats. J Ethnopharmacol 121, 35–42, 10.1016/j.jep.2008.09.032 (2009).
Huang, C. Y., Tsai, Y. T., Lai, J. N. & Hsu, F. L. Prescription pattern of chinese herbal products for diabetes mellitus in taiwan: a population-based study. Evid Based Complement Alternat Med 2013, 201329, 10.1155/2013/201329 (2013).
Lai, E. Y. C. Clinical Evaluation of the Effect of Sha-Sheng-Mai-Dong-Tang on the Serum Antioxidant Capacity and the Immune Modulation in Cancer Patients Receiving the Radiotherapy. Yearbook of Chinese Medicine and Pharmacy 23, 51–70 (2005).
Medicine, N. U. O. C. Chinese medical Great Dictionary (Shanghai Science and Technology Press, Shanghai, 2006).
Lu, K. H., Liu, C. T., Raghu, R. & Sheen, L. Y. Therapeutic potential of chinese herbal medicines in alcoholic liver disease. J Tradit Complement Med 2, 115–122 (2012).
Tang, W. M. et al. A review of the anticancer and immunomodulatory effects of Lycium barbarum fruit. Inflammopharmacology 20, 307–314, 10.1007/s10787-011-0107-3 (2012).
Liu, L. N., Guo, Z. W., Zhang, Y., Qin, H. & Han, Y. Polysaccharide extracted from Rheum tanguticum prevents irradiation-induced immune damage in mice. Asian Pac J Cancer Prev 13, 1401–1405 (2012).
Liu, L. et al. Immunomodulation of Rheum tanguticum polysaccharide (RTP) on the immunosuppressive effects of dexamethasone (DEX) on the treatment of colitis in rats induced by 2,4,6-trinitrobenzene sulfonic acid. Int Immunopharmacol 9, 1568–1577, 10.1016/j.intimp.2009.09.013 (2009).
Liu, L. et al. The beneficial effect of Rheum tanguticum polysaccharide on protecting against diarrhea, colonic inflammation and ulceration in rats with TNBS-induced colitis: the role of macrophage mannose receptor in inflammation and immune response. Int Immunopharmacol 8, 1481–1492, 10.1016/j.intimp.2008.04.013 (2008).
Liu, L. et al. The Effects of Rheum Tanguticum Polysaccharide on the Polarization of Th1 and Th2 Cells in TNBS-Induced Colitis in Murine. Int J Biomed Sci 1, 23–32 (2005).
Liu, L. N. et al. Protective effects of Rheum tanguticum polysaccharide against hydrogen peroxide-induced intestinal epithelial cell injury. World J Gastroenterol 11, 1503–1507 (2005).
Liu, L. et al. Effects of Rheum tanguticum polysaccharide on TNBS -induced colitis and CD4+T cells in rats. World J Gastroenterol 9, 2284–2288 (2003).
Gui, M. et al. Aqueous Extract of Chrysanthemum morifolium (Ju Hua) Enhances the Antimelanogenic and Antioxidative Activities of the Mixture of Soy Peptide and Collagen Peptide. J Tradit Complement Med 4, 171–176, 10.4103/2225-4110.128897 (2014).
Chung, T. W. et al. Salviae Miltiorrhizae BGE Radix increases rat striatal K(+)-stimulated dopamine release and activates the dopamine release with protection against hydrogen peroxide-induced injury in rat pheochromocytoma PC12 cells. Neurochem Res 31, 109–120, 10.1007/s11064-005-9264-3 (2006).
Ling, M. et al. The water-soluble component of Salvia miltiorrhiza Bge can promote macrophage synthesis of C4 in vivo and in vitro. Exp Clin Immunogenet 10, 45–49 (1993).
Gao, D., Mendoza, A., Lu, S. & Lawrence, D. A. Immunomodulatory Effects of Danshen (Salvia miltiorrhiza) in BALB/c Mice. ISRN Inflamm 2012, 954032, 10.5402/2012/954032 (2012).
Sanchez-Duffhues, G. et al. Denbinobin inhibits nuclear factor-kappaB and induces apoptosis via reactive oxygen species generation in human leukemic cells. Biochem Pharmacol 77, 1401–1409, 10.1016/j.bcp.2009.01.004 (2009).
Acknowledgements
This study utilized data that were extracted from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Ministry of Health and Welfare, Taiwan. This study was supported by the National Research Program for Biopharmaceuticals, Ministry of Science and Technology [MOST 103-2325-B-039-009], Taiwan, as well as by China Medical University under the Aim for Top University Plan of the Ministry of Education, Taiwan, R.O.C.
Author information
Authors and Affiliations
Contributions
C.M.C., T.J.C. and H.H.C. were responsible for study concept and design, modification of study design and review and interpretation of data. C.M.C., T.J.C. and H.H.C. were also responsible for drafting the manuscript. H.T.C., S.W.W. and P.C.W. provided modifications of the study design and revised the manuscript. Y.H.W., F.P.C. and H.R.Y. contributed to collection, analysis and interpretation of data and revised the manuscript. All authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chang, CM., Chu, HT., Wei, YH. et al. The Core Pattern Analysis on Chinese Herbal Medicine for Sjögren's syndrome: A Nationwide Population-Based Study. Sci Rep 5, 9541 (2015). https://doi.org/10.1038/srep09541
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep09541
This article is cited by
-
Characterization of hidden rules linking symptoms and selection of acupoint using an artificial neural network model
Frontiers of Medicine (2019)
-
Social-economic analysis of patients with Sjogren’s syndrome dry eye in East China: a cross-sectional study
BMC Ophthalmology (2018)
-
Utilization of Chinese medicine for respiratory discomforts by patients with a medical history of tuberculosis in Taiwan
BMC Complementary and Alternative Medicine (2018)
-
Complementary traditional Chinese medicine use in Children with cerebral palsy: a nationwide retrospective cohort study in Taiwan
BMC Complementary and Alternative Medicine (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.